Introduction
Healthcare workers-defined as individuals engaged in the provision of healthcare services either as employees of healthcare institutions and programs or in a capacity separate from their own, whether qualified or unqualified, and subject to either public or non-public regulations [1]-have received much attention in the last years due to their high rates of occupational stress, burnout, illness, labor turnover, sickness absence, cardiovascular risk, and risk of obesity in comparison with other working sectors [2-5]. Health personnel are particularly prone to the effects of stress [6]. Several studies have found that workload, leadership style, professional conflict, emotional cost of caring, lack of reward, shift working, a perceived increase in responsibility towards patients, role uncertainty, personal costs, and medical bureaucracy are the main sources of occupational stress in nurses and physicians [7-9]. Similarly, a relationship between work-related stress and burnout has been reported in Australian nurses, leading to absenteeism and nursing turnover and, therefore, deriving in staff deficiencies and work augmentation [10]. Among health workers, a high prevalence of obesity has been found associated with long working hours (more than 40 hours per week), shift work, and work-related stress [11,12]. Moreover, an association has been reported between health-impairing behaviors (i.e., infrequent exercise, higher fast food and alcohol consumption, and more frequent painkiller use) with stress in health professionals from seven European countries [13].
On the other hand, promoting an active lifestyle is an essential element of a global public health policy, and the workplace is a critical location for primary prevention through public health initiatives [14]. The World Health Organization (WHO), in its 1997 document titled "Health-Promoting Workplace: Making it Happen" [15], succinctly defined workplace health promotion (WHP) as a diverse range of workplace policies and activities that have been implemented for the express purpose of supporting employers and employees at all organizational levels in the bolstering of their autonomy and the advancement of their physical and mental wellbeing. Thus, healthy work environments are crucial not only to the preservation and enrollment of health personnel and the sustainability of health systems [16], but they also can confer considerable individual and organizational advantages such as diminishing absenteeism and boosting productivity [17]. Previous studies [18,19] have shown that employer-driven workplace wellness interventions centered on employee weight management, enhanced individual health, and employer costs. Likewise, there is also an increasing awareness of the direct costs derived from mental illness and of the effects on workers who remain on the job [20]. Only in 2017, mental illness had an impact on workplaces with depression and anxiety disorders costing US$1 trillion in lost productivity [21]. Additionally, it has been shown that presenteeism has a larger economic cost than absenteeism and employer health costs [22]. In this sense, the relative returns from investing in worksite wellness programs are favorable: savings of US$35 on monthly healthcare costs and US$2.73 linked to absenteeism for each dollar paid [23,24].
Interestingly, regardless of the proven effectiveness of worksite health interventions in diminishing multiple health risk factors, increasing productivity, minimizing absenteeism, and decreasing health care costs [17,25-27] as well as the research efforts to improve the health and well-being of healthcare workers, the acute and long term sickness absence, in particular scenarios, remains high [28]. Similarly, a recent systematic review of literature on worksite-based diet/physical activity interventions showed that the most effective methods tended to be the costliest in terms of both time and resources [29], which is potentially problematic when it comes to implementing them in a wider range of work setups. Finally, it is worth mentioning that, although an increase in mental health promotion programs has been reported in the last few decades, just a small percentage (7) was workplace-based [30]. Thus, additional research is needed to further establish the key aspects that determine the effectiveness of health activity interventions.
Therefore, this study aimed to identify the effect of workplace health promotion activities (WHPA) on the health status (both physical and mental) of health personnel by employing a systematic literature review. This information can help to make informed decisions and prioritize public health activities in the workplace.
Methodology
Literature search strategy
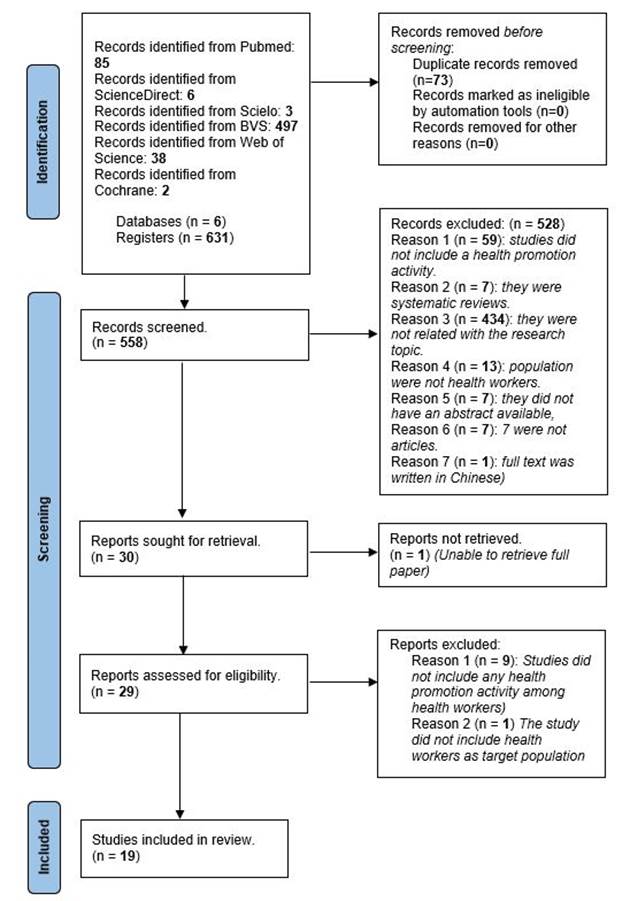
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [31]. Six databases were used to search studies on the effect of at least one health promotion activity on the health status of health personnel: PUBMED (National Library of Medicine, USA), ScienceDirect (Elsevier, Netherlands), Scielo (Portal de la BVS, Brazil), Biblioteca Virtual en Salud (BVS) (Portal Regional de la BVS, América Latina y el Caribe), Web of Science (WoS) (Clarivate Analytics, USA), and Cochrane (Central Register of Controlled Trials, UK). Since we wanted to identify as many studies as possible, we did not filter them by year. Searches were performed from Bogotá, Colombia on July 13th, 2022, using the following DeCS terms: health promotion, health personnel, and medical staff. Three different search strings were built depending on the database (see Table 1]. All records identified were imported to Zotero, where duplicates were removed. The remaining studies were reviewed by one of the authors based on inclusion and exclusion criteria defined by both researchers.
Table 1 Search string per database
| Database | Search String |
| PUBMED | “Health promotion"[Title/Abstract] AND ("health personnel"[Title/Abstract] OR "medical staff”) [Title/Abstract] AND (workplace [Title/Abstract] OR hospitals) [Title/Abstract] |
| ScienceDirect | “Health promotion" AND ("health personnel" OR "medical staff") AND (workplace OR hospitals) |
| Biblioteca Virtual en Salud | |
| Web of Science | |
| Cochrane | |
| Scielo | "Promoción de la salud" AND ("personal de salud" OR "personal médico") AND (lugar de trabajo OR hospitales) |
Eligibility criteria
Studies were included if they met all the following initial criteria: they were published in peer-reviewed and indexed journals; they were written either in English, Spanish, or Portuguese; they included health personnel as subjects of intervention; they included at least one health promotion activity among health workers. Systematic reviews were excluded from the sample.
Data extraction
Seven variables were extracted from each publication: the study’s first author, year of publication, country of affiliation of the first author, study population, sample size, type of study, outcome, health promotion activities performed, and language (see Table 2].
Assessment of methodological quality
Four instruments were considered to evaluate the quality of the included publications: The Cochrane risk-of-bias tool for randomized trials (RoB-2, version 2), The Quality Assessment Tool for Quantitative Studies, The National Institutes of Health (NIH) quality assessment tool, and The JBI’s critical appraisal tools. After considering aspects such as format (i.e., scale, items, checklist), overall quality assessment (yes/no), scoring range, scale/checklist development (reported/not reported), suitability according to the type of studies, validity, and reliability, we decided to use the Quality Assessment Tool for Quantitative Studies (Effective Public Healthcare Practice Project, 1988). This tool considers eight main components assessed using a scale ranging from 1 to 3, where 1 is considered “strong quality,” 2 is “moderate quality,” and 3 is “weak quality.” The components are as follows: (a) selection bias, (b) study design, (c) confounders, (d) blinding, (e) data collection methods, (f) withdrawals and drop-outs, (g) intervention integrity, and (h) analyses. The overall quality of each publication was estimated based on the number of “weak” ratings found in the evaluation as follows: strong = no “weak” ratings; moderate = one “weak” rating; and weak = two or more “weak” ratings. Both authors independently assessed all the included publications for methodological quality.
Results
Study selection
Figure 1 shows the flowchart of the literature search. In total, 558 potential studies were identified after removing the duplicates. Then, 528 titles were excluded for the following reasons: 434 were not related to the research topic; 59 did not include a health promotion activity; 13 were not implemented among health workers; 7 did not have an abstract available; 7 were systematic reviews; 7 were not articles; and 1 the full text was written in Chinese. Then, we did not grant access to one out of the 30 included papers; therefore, 29 articles were included for a full revision. After reading the full papers, 9 studies were removed because they did not incorporate any health promotion activity among health workers, and 1 did not include health workers as the target population. Thus, the final sample consisted of 19 papers that were included for methodological quality assessment.
Description of included studies
All the studies were written in English and most of them (n = 11) were conducted in the United States, two in Italy [32,33], two in the UK [14,17], two in Denmark [34,35], one in Germany [36], and one in Spain [37]. Sample sizes ranged from 20 [38] to 18,075 participants [39]. Nine out of 19 studies were randomized controlled trials (RCT), and ten were quasi-experimental designs or nonrandomized trials (six were pretest (pre)-posttest (post) comparisons [32,33,37,40-42], three observational studies [39,43,44], and one nonrandomized trial [38]). Most of the studies (n = 6) defined their population as “healthcare workers” [14,33,37,39,45,46], three referred to the population as “staff” [17,35,40], two as “employees” [44,47], one as “workers” [48], one as “ambulatory caregivers” [41], one as “personnel” [34], and one as “subjects” [32]. Four studies detailed their participants per occupation (i.e., physicians, nurses, administrators) [36,38,42,43] (see Table 2].
Table 2 Characteristics of the Publications Included
| ID | Study first author (year-country) | Study Population | Sample Size | Type of Study | Outcome | HPAs | Language |
|---|---|---|---|---|---|---|---|
| 1 | Abu Dabrh, A (2016 - United States) | Healthcare workers | 662 | Pre-post assessment | Cardiovascular exercise, Cigarette smoking | 1*, 2* 3* | English |
| 2 | Armitage, C (2015 - UK) | Healthcare workers | 79 | Randomized controlled trial | Diet, Metacognitive processing | 2 | English |
| 3 | Batlle, E (1991 - Spain) | Healthcare workers | 306 | Pre-post assessment | Percentage of participants that smoke | 3 | English |
| 4 | Blake, H (2017 - UK) | Healthcare workers | 296 | Randomized controlled trial | Work-related physical activity, Vigorous and moderate recreational physical activity, Active travel behavior | 1 | English |
| 5 | Brunges, M (2006 - United States) | Perioperative nurses | 20 | Nonrandomized controlled trial | Glucose, Lipids, Weight, Body fat | 1 | English |
| 6 | Christensen, J (2011 - Denmark) | Personnel in care units | 98 | Randomized controlled trial | Body weight BMI, Body fat percentage, Waist circumference, Blood pressure, Musculoskeletal pain maximum, Oxygen uptake, Muscle strength | 1, 2, 4* | English |
| 7 | Doran, K (2018 - United States) | Workers from nursing homes | 98 | Randomized controlled trial | Mood, Sleep hours, Sleep Quality, Dietary sodium intake | 1, 2, 5* | English |
| 8 | Duncan, A (2011 - United States) | Health and support staff | 2756 | Longitudinal Evaluation of study outcomes | Sense of relaxation, Stress, Energy level, Pain level | 5, 6*, 7* | English |
| 9 | Estabrook, B (2012 - United States) | Hospital employees | 806 | Longitudinal Evaluation of study outcomes | Perception of their hospital’s commitment to employee wellness BMI | 1, 2, 6, 8* | English |
| 10 | Fragala, G (2016 - United States) | Ambulatory caregivers | 32 | Pre-post assessment | Physical exertion | 1 | English |
| 11 | Hjorth, P (2016 - Denmark) | Healthcare workers | 337 | Randomized controlled trial | Waist circumference Diastolic blood pressure | 1, 2, 3 | English |
| 12 | Lazzeri, G (2019 - Italy) | Health and support staff | 2400 | Randomized pre-post comparison | BMI Sedentariness | 1, 2 | English |
| 13 | Low, V (2015 - United States) | Healthcare workers | 57 | Unblinded randomized trial | Weight loss, Stress, Days per week of exercise | 1, 2, 3, 5 | English |
| 14 | Mache, S (2018 -Germany) | Junior physicians | 70 | Randomized controlled trial | Perceived stress, Emotional exhaustion, Emotion regulation skills, Job Satisfaction, Work Engagement | 4 | English |
| 15 | Mistretta, E (2018 - United States) | Healthcare workers | 60 | Randomized controlled trial | Stress and well-being, Emotional exhaustion, Self-compassion | 5, 9*, 10* | English |
| 16 | Parkinson, M (2014 - United States) | Healthcare workers | 18075 | Observational study | Health risk levels | 1, 2, 3, 5, 11*, 12* | English |
| 17 | Pipe, T (2012 - United States) | Health and support staff | 44 | Pre-post assessment | Stress | 5* | English |
| 18 | Scapellato, M (2018 - Italy) | Healthcare workers | 167 | Pre-post assessment | Physical activity, Dietary habits, Weight loss, LDL/HDL cholesterol, Triglyceride levels, Blood glucose levels, Systolic and diastolic pressure | 1, 2 | English |
| 19 | Sorensen, G (2016 - United States) | Healthcare workers | 482 | Randomized controlled trial | Sleep, Diet, Physical activity, Pain, Ergonomic practices, Supervisor and coworker support, Safety practices, Meal break frequency | 1, 2, 7 | English |
1* Physical activity, 2* Nutrition, 3* Smoking cessation, 4* Mental health training, 5* Stress management, 6* Social relationships. 7* Sleep hygiene, 8* Institutional support, 9* Well-being improvement, 10* Burnout reduction, 11* Safety belt usage, 12* Alcohol usage
Outcomes - health conditions
Nine out of 19 publications targeted physical health outcomes (i.e., physical activity, recreational physical activity, physical exertion, muscle strength, cardiovascular exercise, sedentariness, energy level, pain level, dietary habits, meal break frequency, body weight, body fat percentage, body mass index (BMI), waist circumference, low-density lipoprotein (LDL)/high-density lipoprotein (HDL) cholesterol levels, triglyceride levels, blood glucose levels, oxygen uptake, systolic and diastolic pressure, ergonomic practices, safety practices, and smoking habits) [32-35,37-41]. Three out of 19 publications focused on mental health outcomes (i.e., perceived stress, emotional exhaustion, emotion regulation skills, job satisfaction, work engagement, well-being, self-compassion) [36,42,47], whereas seven adopted a mixed approximation [17,43-46,48,49] that included mood, sleep hours, sleep quality, metacognitive processing, dietary sodium intake, weight loss, days per week of exercise, sense of relaxation, and energy and pain levels. Only 3 studies considered social outcomes (i.e., active travel behavior, supervisor and coworker support, and perception of their hospital’s commitment to employee wellness) [14,44,46].
Health promotion activities
A total of seven studies investigated the effect of a single WHPA on health personnel [14,17,36-38,41,42], whereas two considered the effect of two WHPAs [32,33], and ten researched the effect of three or more WHPAs [34,35,39,40,43-48]. In total, 13 studies used the promotion of physical activity as WHPA [14,32-35,38-41,44-46,48], 11 included nutritional recommendations [17,32-35,39,40,44-46,48], 13 focused on mental health training (i.e., stress management, resilience training, sleep, and emotion tracking, quality of life, smoking cessation, safety belt usage, alcohol usage, and cognitive behavioral training) [14,34-37,39,40,42,43,45-48], and only 2 implemented social activities (i.e., workplace or personal relationships, perceived institutional support and social norms) [43,44] (see Table 3].
Table 3 Characteristics of the Health Promotion Activities (HPA)
| ID | Study first author (year-country) | HPA | Basis | Duration | Activities |
|---|---|---|---|---|---|
| 1 | Abu Dabrh, A (2016 - United States) | Physical activity | Not reported | 12 months | Not described |
| Smoking cessation | |||||
| Nutrition | |||||
| 2 | Armitage, C (2015 - UK) | Nutrition | Prochaska and DiClemente’s transtheoretical model | 1 month | To consume an extra portion of fruit each day |
| 3 | Batlle, E (1991 - Spain) | Smoking cessation | Not reported | 30 months | Sessions about smoking and its harmful consequences |
| 4 | Blake, H (2017 - UK) | Physical activity | Theory of planned behavior | 3 months | Educational material regarding the importance of physical activity. |
| 5 | Brunges, M (2006 - United States) | Physical activity | Not reported | 12 months | Physical therapy |
| 6 | Christensen, J (2011 - Denmark) | Nutrition | Danish dietary recommendations | 12 months | Dietary advice and 10-15 minutes of physical exercise training |
| Physical activity | |||||
| Mental health training | |||||
| 7 | Doran, K (2018 - United States) | Nutrition | The theory of self-efficacy and the social-ecological mode | 12 months | A 30-minute group education session |
| Physical activity | |||||
| Stress management | |||||
| 8 | Duncan, A (2011 - United States) | Stress management | Chinese medicine | Between 1 to more than 12 sessions (1 per week) | Ear acupuncture, clinical acupressure, zero balancing |
| Sleep | |||||
| Social relationships | |||||
| 9 | Estabrook, B (2012 - United States) | Nutrition | The RE-AIM framework* | 24 months | Leadership engagement and employee input |
| Physical activity | |||||
| Perceived institutional support | |||||
| Social norms | |||||
| 10 | Fragala, G (2016 - United States) | Physical activity (load handling) | Not reported | 1 day | To assist dependent patients to fixed-height examination tables |
| 11 | Hjorth, P (2016 - Denmark) | Physical activity | Not reported | 12 months | Group discussions about health, smoking cessation, and preventive measures at the facility |
| Smoking cessation | |||||
| Nutrition | |||||
| 12 | Lazzeri, G (2019 - Italy) | Nutrition | The Tuscan Dietary Pyramid and the IARC guidelines | 12 months | Fresh fruit and vegetables were made available at least three days a week |
| Physical activity | |||||
| 13 | Low, V (2015 - United States) | Nutrition | Not reported | 6 months | Goal setting and suggestions for overcoming obstacles. Gymnasium and organized walks. |
| Stress management | |||||
| Physical activity | |||||
| Smoking cessation | |||||
| 14 | Mache, S (2018 - Germany) | Mental health training | Lazarus’s transactional model of stress | 3 months | Theoretical input, oral group discussions, experiential exercises, and home assignments |
| 15 | Mistretta, E (2018 - United States) | Stress management | Not reported | 3 months | Sleep and emotion tracking and mindfulness meditation |
| Well-being improvement | |||||
| Burnout reduction | |||||
| 16 | Parkinson, M (2014 - United States) | Nutrition | Not reported | 12 months | Educational materials, self-help tools, and group support related to managing lifestyle issues |
| Stress management | |||||
| Smoking cessation | |||||
| Safety belt usage | |||||
| Physical activity | |||||
| Alcohol usage | |||||
| 17 | Pipe, T (2012 - United States) | Stress management | Behavioral interventions | Two sessions approximately 3 weeks apart | Two workshop sessions: Transforming Stress and Level 5 |
| 18 | Scapellato, M (2018 - Italy) | Nutrition | Food pyramid | 6 months | Food and physical activity |
| Physical activity | |||||
| 19 | Sorensen, G (2016 - United States) | Physical activity | "Be well, work well" intervention | 17 months | Safe patient handling training; a healthy eating question and answer session; a presentation and conversation with a sleep expert. |
| Nutrition | |||||
| Sleep |
* Reach, Effectiveness, Adoption, Implementation, and Maintenance of intervention
Effectiveness of interventions
All the studies but one reported the effectiveness of their interventions [32]. Six studies reported lower scores on perceived stress [36,39,42,43,45,47], and two on emotional exhaustion for the intervention group (IG) at different follow-up moments [36,47]. Higher scores on emotion regulation skills, job satisfaction, and work engagement for the IG were shown in one study compared with the levels observed in the waitlist control group [36]. Statistically significant improvements in well-being and self-compassion (being kind to oneself and having a nonjudgmental attitude towards one’s faults) were confirmed in one study [47]. One study evidenced a significant reduction in mood symptoms (such as stress, anxiety, and/or depressive symptoms) [48], an increase in sleep hours from 6.4 at baseline to 7.3 at 12-month follow-up, a better sleep quality, and a reduction in dietary sodium intake in the IG over time.
On the other hand, seven studies showed that the participants’ dietary habits improved, and the IG prompted weight loss, which was reflected in a substantial reduction in either waist circumference, body weight, BMI, or body fat percentage [15,33,35,39,45,51,54]. Increased physical activity (e.g., exercise days per week, recreational activity, and duration and frequency of active travel) for the IG was reported in six studies [14,33,39,40,43,45], and a reduction in pain levels was reported in one study [43]. Lastly, a reduction in the prevalence of cigarette smoking was reported in three studies [37,39,40].
As for metabolic variables, two studies reported a statistically significant reduction in blood glucose levels in the IG [33,38]. Five studies found that both systolic and diastolic pressure measurements in the IG were lower compared with the control groups or the post-assessment measures [33-35,38,39]; and in one study [33], the interventions led to a reduction in total LDL and HDL cholesterol. Triglyceride levels dropped overall but only changed significantly among women. Lastly, one study showed that the intervention improved their perception of their hospital’s commitment to employee wellness [44].
Quality assessment
All the papers included were independently read and evaluated by both authors. Any discrepancy was resolved in a consensus meeting. Based on the Quality Assessment Tool for Quantitative Studies Effective Public Health Practice Project criteria, eleven articles were categorized as “weak” in methodological terms, three as “moderate,” and five as “strong” (see Table 4].
Table 4 Methodological Quality Assessment of Included Publications using the Quality Assessment Tool for Quantitative Studies Effective Public Health Practice Project
| Study first author (year-country) | Selection | Study design | Confounders | Blinding | Data collection | Withdrawals and drop-outs | Global rating |
|---|---|---|---|---|---|---|---|
| Mache, S (2018 -Germany) | 1 | 1 | 1 | 2 | 1 | 2 | STRONG |
| Lazzeri, G (2019 - Italy) | 3 | 3 | 3 | 2 | 2 | 2 | WEAK |
| Scapellato, M (2018 - Italy) | 3 | 2 | 3 | 2 | 3 | 2 | WEAK |
| Doran, K (2018 - United States) | 3 | 1 | 1 | 2 | 1 | 2 | MODERATE |
| Mistretta, E (2018 - United States) | 3 | 1 | 3 | 2 | 1 | 2 | WEAK |
| Blake, H (2017 - UK) | 3 | 1 | 1 | 2 | 1 | 3 | WEAK |
| Fragala, G (2016 - United States) | 3 | 2 | 3 | 2 | 1 | 3 | WEAK |
| Sorensen, G (2016 - United States) | 1 | 2 | 3 | 2 | 2 | 1 | MODERATE |
| Abu Dabrh, A (2016 - United States) | 2 | 2 | 3 | 2 | 3 | 2 | WEAK |
| Hjorth, P (2016 - Denmark) | 2 | 1 | 1 | 2 | 2 | 2 | STRONG |
| Low, V (2015 - United States) | 2 | 1 | 1 | 2 | 1 | 1 | STRONG |
| Armitage, C (2015 - UK) | 2 | 2 | 3 | 2 | 1 | 2 | MODERATE |
| Parkinson, M (2014 - United States) | 2 | 2 | 1 | 2 | 1 | 2 | STRONG |
| Pipe, T (2012 - United States) | 2 | 2 | 3 | 2 | 2 | 3 | WEAK |
| Estabrook, B (2012 - United States) | 2 | 2 | 3 | 2 | 3 | 3 | WEAK |
| Duncan, A (2011 - United States) | 1 | 2 | 3 | 3 | 3 | 3 | WEAK |
| Christensen, J (2011 - Denmark) | 2 | 1 | 1 | 2 | 2 | 1 | STRONG |
| Brunges, M (2006 - United States) | 2 | 2 | 3 | 3 | 2 | 1 | WEAK |
| Batlle, E (1991 - Spain) | 1 | 2 | 3 | 3 | 3 | 1 | WEAK |
1 = “strong,” 2 = “moderate,” 3 = “weak”
Discussion
The purpose of this study was to determine the effect of WHPA on the health conditions of health workers by employing a systematic literature review. This review included 19 publications that reported changes in health outcomes associated with WHPA. Although quality assessment showed that publications’ quality was heterogeneous (from weak to strong) and the intervention designs were very different, the overall results suggest that WHPAs can improve physical and mental health, and wellbeing and encourage healthier behaviors in health personnel.
The fact that nine out of 19 studies utilized a randomized controlled design shows that RCTs are the most used methodological approach to studies aiming to determine the effect of HPAs on healthcare workers’ health status and well-being. This is certainly congruent when the objective is to assess the efficacy of a relatively standard intervention producing a discrete outcome [20]. Nevertheless, in this review, there was no association between the study design with the type of HPA or the outcome. Now, knowing that RCT design can have some disadvantages such as logistics (power calculation might demand vast sample sizes, external validity may be threatened by factors such as atypical populations units, and long trial run time may result in the loss of relevance), statistics (allocation of participants may be expectable resulting in selection bias when the study groups are unmasked), applicability (trials which test for efficacy may not be broadly applicable, trials which test for effectiveness are larger and more expensive, and results may not always imitate real-life treatment situation), and ethical challenges (withholding potentially beneficial interventions from control population units) [50,51], pre-post designs may also be appropriate to address this research topic.
Regarding health conditions, the majority of the papers reported interventions primarily focused on physical health conditions. This was followed by interventions addressing both physical and mental health aspects, interventions targeting solely mental health, and interventions addressing the social contexts in which health personnel work. Concerning health promotion activities, most interventions included three or more activities followed by the implementation of a single activity and, finally, the implementation of two activities. This result agrees with previous literature that has shown that mental disorders are not considered with the same importance as physical health and that the association between health and mental health is either overlooked or unrealized [52]. This can be explained due to the evolution of the health concept, which only changed nearly 70 years ago when the WHO in 1948 defined health as “a state of complete physical, mental and social well-being, not merely the absence of infirmity or disease,” expanding the notion of health from a simple concern about the physical features of a disease to a contemplation of the social determinants of a patient’s health outcomes and quality of life. Moreover, it centered on the need to accomplish well-being, which diverges from the mere lack of disease by also incorporating psychosocial, behavioral, and environmental considerations [53]. Nevertheless, although this definition was a step forward for health improvement, it was not practical due to being too fundamental and could not be reliably and equitably enforced [54]. It has been only until recent times that in light of some of the shortcomings of the WHO definition, others have proposed broader definitions such as “a holistic state of physical, mental, emotional, and social wellness supported by an integrated and technologically sophisticated healthcare delivery system tailored to meet the entirety of a patient’s medical needs, including disease prevention and management of undesirable conditions, comorbidities, complications, and unique patient circumstances” [53], p.7, allowing researchers and policymakers to truly transcend from the physical characteristics of health to a holistic perspective of it.
Based on this analysis, being mentally healthy should be given the same urgency by policymakers as maintaining physically fit [55]. This is because there is substantial evidence demonstrating the association between physical and mental health and lifestyle choices, such as diet, exercise, smoking, and alcohol consumption [56]. To achieve these goals, policies are needed to preserve good mental health instead of only caring for acute mental illness; there should be a larger emphasis on delivering effective services for individuals with common issues, such as depression and anxiety, and helping to keep people mentally well [55]. Therefore, it is imperative to adopt a “whole person” perspective when it comes to providing healthcare services, otherwise the notion of having a fixed differentiation between “mental health professionals” and “physical health professionals” can create a reduced sense of responsibility, meaning that opportunities to improve outcomes are neglected [57].
On the other hand, due to the heterogeneity of types of studies and measures used in the included articles, it is not possible to make meaningful comparisons between the studies. Nevertheless, we would like to draw particular attention to three results. First, only one study did not show any statistically significant difference after having implemented the HPA [32]. As per the authors’ analysis, this result seemed to indicate that in that specific context, lifestyle improvements (healthier eating and increased physical activity) cannot be registered in the short term (12 months); however, we proposed an alternative explanation. The intervention on dietary habits focused mainly on making fresh fruit and vegetables available at least three days a week and placing campaigns to publicize the “Tuscan Dietary Pyramid” (Piramide Alimentare Toscana, PAT), the IARC guidelines, instructions for calculating BMI, and material regarding the project. These educational strategies have shown to be less effective than behavioral approaches for short-term weight loss [58] as the one described in the study where no differences were found. Now, despite this, it is undeniable that at least in the field of health promotion, researchers must face issues regarding the selection of indicators and the timing of measurements that are often complex and controversial, in addition to having to manage anonymous data, which impedes the analysis of intra-subject variations in risk factors (considered as the major limitation of this type of investigation) [32].
Second, most of the studies targeting mental health focused their efforts primarily on reducing healthcare workers’ perceived stress. This may be explained due to the growing recognition of multiple situations that challenge health personnel to meet work-related demands, leading them to illness, labor turnover, and absenteeism [4], as well as impeding organizations from recruiting new workers and retaining those already present in the workplace [59]. It is worth mentioning that most of these interventions had a sustained effect over time that exposed two main elements: on the one hand, the efficacy of mindfulness-based stress reduction training as described in other studies [36,60,61]; and on the other hand, the effectiveness of using well-established problem-solving, emotion-regulation strategies, coping skills as well as approaches for improved communication skills to reduce stress in the long term [62].
Third, HPAs that addressed both diet and physical activity behaviors were more effective in improving weight outcomes than those that used only one approximation. This finding is in agreement with previous studies [5]. Finally, we noticed that most of the interventions were centered on enhancing individual coping skills, rather than impacting the workplace environment such that it promotes healthier behaviors, which is something that has been reported in other studies as well [63].
As with any research, this study entails certain inherent limitations that warrant consideration. Firstly, the restricted number of articles incorporated in our analysis curtails the extent to which our results can be extrapolated and applied to a broader context. Secondly, the substandard quality of most of these publications hampers the formulation of overarching conclusions. Nevertheless, although these limitations are evident, to the best of our knowledge, this systematic review is the first to assess the impact of at least one health promotion activity on healthcare workers in the workplace. This study offers valuable information to public and occupational health researchers on the impact of worksite-based health promotion interventions, including the effect of different strategies applied. Occupational health professionals should continue applying evidence guidance frameworks/tools, and developing multicomponent interventions that allow them to identify, reduce, and, if possible, eliminate work-related hazards that jeopardize workers’ health and well-being.