Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Biomédica
Print version ISSN 0120-4157
Biomédica vol.32 no.2 Bogotá Apr./June 2012
PRESENTACIÓN DE CASO
1Division of Infectious Diseases, University of Colorado, Denver, USA
2División de Hematología-Oncología, Universidad Militar Nueva Granada, Bogotá, D.C., Colombia
Author contributions:
All authors contributed with the preparation and edition of the manuscript.
Recibido: 16/08/11; aceptado:17/02/12
Acinetobacter skin and soft tissue infection outside of the traumatic wound setting are rare occurrences. The majority of cases occur in the presence of significant comorbilities and by Acinetobacter baumanii. Herein a case is reported of community-onset, health-care-associated, non-traumatic cellulitis caused by Acinetobacter, species junii-johnsonii with bacteremia. This is the first reported case of Acinetobacter junii-johnsonii skin and soft tissue infection. Hemorrhagic bullae might be one of the clinical features of Acinetobacter cellulitis.
Key words:Acinetobacter, cellulitis, community-acquired infections, bacteremia, blister, therapy.
Celulitis por Acinetobacter junii-johnsonii adquirida en la comunidad: una presentación de caso
La infección de piel y tejidos blandos por Acinetobacter no relacionada con trauma es una presentación inusual. La mayoría de los casos descritos presentan enfermedades concomitantes y son causados por Acinetobacter baumanii. Se describe un caso de celulitis no traumática por A. junii-johnsonii con bacteriemia, de inicio en la comunidad y asociado con el tratamiento médico. De acuerdo con nuestro conocimiento, éste sería el primer caso reportado de infección de tejidos blandos y piel por A. junii-johnsonii. La vesícula hemorrágica podría ser una característica clínica de celulitis por Acinetobacter.
Palabras clave:Acinetobacter, celulitis, infecciones comunitarias adquiridas, bacteriemia, vesícula, tratamiento.
Acinetobacter is a widely recognized pathogen in the hospital setting. However, cases in the community are uncommon. Among community-acquired cases, the most frequent presentation is pneumonia. Non-traumatic skin and soft tissue infection remains an uncommonly described presentation in any setting, although necrotizing fasciitis by Acinetobacter baumanii has been well characterized.
Case report
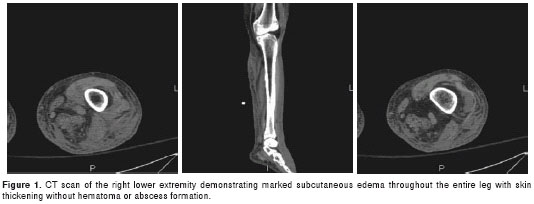
In August 2010, a 48 year old man with a history of metastatic, stage IV, prostate cancer was admitted to the University of Colorado Hospital after being transferred from an outside hospital. The case was complicated by bladder obstruction, T8 fracture, spinal cord involvement and had been treated with androgen-deprivation therapy and local radiation therapy. The patient had been admitted one month prior to this presentation with a pulmonary embolus, methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia of unclear origin and also with a multidrug resistant (MDR) Serratia marcescens urinary tract infection. The patient recovered from that episode and was discharged to his home on intravenous (IV) ertapenem, 1gram every 24 hours. Several weeks later, the patient was readmitted to an outside hospital after developing a rapid progression of symptoms characterized by the following: marked fatigue, light headedness, fever, chills and right lower extremity swelling, erythema, tenderness and warmness. On admission the patient was found to be in septic shock, requiring intensive care unit care. He received aggressive fluid resuscitation therapy and pressor support; and he was placed empirically on IV vancomycin, piperacillin-tazobactam and levofloxacin. His hemodynamic parameters improved over the next two days, and he was transferred to our hospital with the documentation of a non fermenting gram negative rod (GNR) in blood culture (1 of 2 bottles). Computerized tomography (CT) scan of his leg showed a marked subcutaneous edema (figure 1). The positive culture was from a peripheral site. The physical examination was remarkable for marked right lower extremity swelling, with erythema involving the distal 2/3 of the leg, and local tenderness, warmness and the presence of a purpuric rash and hemorrhagic bullae. The PICC line was present and was without local signs of inflammation. The laboratory tests were significant for leukopenia, anemia and thrombocytopenia. The gram negative rod was a nonmotile, catalase-positive, oxidase-negative bacteria; finally identified using the Vitek 2 system (an automated system for bacterial identification using a phenotypic approach) as Acinetobacter junii-johnsonii, sensitive to quinolones and B-lactams, and intermediate to aztreonam. His antibiotic therapy was narrowed to Levofloxacin only, and the patient was discharged 4 days later. He was seen again in the clinic 4 weeks later; complete resolution of his local right leg inflammatory changes were noted.
Discussion
Acinetobacter is a ubiquitous, encapsulated, non-motile, aerobic gram negative cocco-bacillus. It is widely recognized as an opportunistic pathogen and known to cause hospital acquired infections ranging from pneumonia to bacteremia, UTI and soft tissue infections (1,2). It is also recognized for its ability to develop multi-drug resistant mechanisms, making the treatment often difficult.
Although less common, community-acquired Acinetobacter (CA-AB) infections have also been described (3). A prior systematic review of 123 patients with CA-AB infections showed that the most prevalent type of infection was pneumonia followed by bacteremia. In that review, only one case of skin and soft tissue infections was reported (4). Among the descriptions of cases of ocular infections, conditions described are conjunctivitis, preseptal cellulitis, endophtalmitis and corneal perforation.
Acinetobacterskin and soft tissue infections frequently complicates traumatic injuries as a consequence of war or natural disasters, especially in areas like Afghanistan, Iraq or tropical Southeast Asia (5-8). Non traumatic Acinetobacterskin and soft tissue infections has been rarely reported. However, when it is reported, the bacterium involved is by Acinetobacter baumanii and associated with more extensive infections such as necrotizing fasciitis and increase mortality (1,9,10). In the best of our knowledge, there are no other cases of reported with skin and soft tissue infections caused by A. junii-johnsoni.
Based on prior descriptions; it seems that older age, prior antibiotic use and comorbilities such as cirrhosis, nursing home residency, dementia and diabetes may play a role as potential risk factors for this type of infection. In the case presented here, the patient had metastatic cancer and was on IV antibiotics at the time of presentation to the hospital. Notably, this infection was acquired while on a broad spectrum antibiotic: ertapenem, an antibiotic known to be less effective against non fermenting GNR such as Acinetobacter.Another important consideration gleaned from the described cases is that the development of necrotizing fasciitis from a multi-drug resistant A. baumanii is translated to a high mortality (1,9). A trend to a MDR pattern has also been recognized in the antibiotic susceptibility profiles of the community Acinetobacter strains.
As described previously with an Acinetobacter infected traumatic wound injury cases (5) and in a necrotizing fasciitis case (9), hemorrhagic bullae can be found in this type of skin and soft tissue infection—as indicated in the case presented herein. Therefore, although infrequent, the presence Acinetobacter cellulitis must be determined in patients that are not responding to the initial antibiotic therapy, especially in the presence of hemorrhagic bullae. No clinical data are available on which to base selection of combination therapy vs. monotherapy for this type of infection. However depending of the severity of the infections like in this case, a reasonable approach is to double the antibiotic coverage initially while awaiting final susceptibilities. Once they are available, the treatment can be simplified to a monotherapy.
Finally, it is important to recognize that A. baumanii is not the only possible cause of SSTI, but that other species such as A. junii-johnsonii may be responsible. The severity described with the former may be due to the MDR profile or virulent factors. Acinetobactor baumanii has been isolated from multiple body sites. However, its main impact is as a cause of ventilator associated pneumonia. In contrast A. junii-johnsonii has been described as a skin colonizer and as a cause of catheter related bacteremias in the setting of prior antibiotic use, malignancy or invasive procedures (11,12).
Conflicts of interest
No conflicts of interest were reported by Drs. Andrés F. Henao-Martínez, Guido R. González-Fontal and Steven Johnson.
Financing
No funding agencies had a role in the preparation, review or approval of the manuscript. The views expressed in the article are those of the authors and do not necessary represent the views of the University of Colorado Denver or Universidad Militar Nueva Granada.
Corresponding author: Andrés F. Henao-Martínez, University of Colorado Denver, 12700 E, 19th Avenue, Denver, USA, Mail Stop B168, Aurora, CO 80045. Telephone: (303) 724 6451; fax: (303) 724 6462 andres.henaomartinez@ucdenver.edu
References [ Links ]
2. Muñoz-Price LS, Zembower T, Penugonda S, Schreckenberger P, Lavin MA,Welbel S, et al. Clinical outcomes of carbapenem-resistant Acinetobacter baumannii bloodstream infections: Study of a 2-state monoclonal outbreak. Infect Control Hosp Epidemiol. 2010;31:1057-62. [ Links ]
3. Chiang WC, Su CP, Hsu CY, Chen SY, Chen YC, Chang SC, et al. Community-acquired bacteremic cellulitis caused by Acinetobacter baumannii. J Formos Med Assoc. 2003;102:650-2. [ Links ]
4. Falagas ME, Karveli EA, Kelesidis I, Kelesidis T. Community-acquired Acinetobacter infections. Eur J Clin Microbiol Infect Dis. 2007;26:857-68. [ Links ]
5. Sebeny PJ, Riddle MS, Petersen K.Acinetobacter baumannii skin and soft-tissue infection associated with war trauma. Clin Infect Dis. 2008;47:444-9. [ Links ]
6. Murray CK, Yun HC, Griffith ME, Hospenthal DR, Tong MJ.Acinetobacter infection: What was the true impact during the Vietnam conflict? Clin Infect Dis. 2006;43:383-4. [ Links ]
7. Scott P, Deye G, Srinivasan A, Murray C, Moran K, Hulten E, et al. An outbreak of multidrug-resistant Acinetobacter baumannii-calcoaceticus complex infection in the US military health care system associated with military operations in Iraq. Clin Infect Dis. 2007;44:1577-84. [ Links ]
8. Maegele M, Gregor S, Steinhausen E, Bouillon B, Heiss MM, Perbix W, et al. The long-distance tertiary air transfer and care of tsunami victims: Injury pattern and microbiological and psychological aspects. Crit Care Med. 2005;33:1136-40. [ Links ]
9. Villalba F, Manana P, Limongi G. Necrotizing cellulitis caused by Acinetobacter baumannii. Enferm Infecc Microbiol Clin. 2000;18:479-80. [ Links ]
10. Sullivan DR, Shields J, Netzer G. Fatal case of multi-drug resistant Acinetobacter baumannii necrotizing fasciitis. Am Surg. 2010;76:651-3. [ Links ]
11. Hung YT, Lee YT, Huang LJ, Chen TL, Yu KW, Fung CP, et al. Clinical characteristics of patients with Acinetobacter junii infection. J Microbiol Immunol Infect. 2009;42:47-53. [ Links ]
12. Seifert H, Strate A, Schulze A, Pulverer G. Vascular catheter-related bloodstream infection due to Acinetobacter johnsonii (formerly Acinetobacter calcoaceticus var. lwoffi): Report of 13 cases. Clin Infect Dis. 1993;17:632-6. [ Links ]













