Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Biomédica
Print version ISSN 0120-4157
Biomédica vol.32 no.2 Bogotá Apr./June 2012
ARTÍCULO ORIGINAL
Liliana Alejandra Chicaíza-Becerra1, Mario García-Molina1, Óscar Gamboa2
1Facultad de Ciencias Económicas, Universidad Nacional de Colombia, Bogotá, D.C., Colombia
2Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
Contribución de los autores:
Todos los autores aportaron al diseño del trabajo, la recopilación y análisis de los datos y la escritura del documento final.
Recibido: 18/05/11; aceptado:22/12/11
Introduction. Contrast media can cause acute renal failure by direct toxic effects on the tubular cells and kidney ischemia. Diabetics and hospitalized patients have a greater risk of developing contrast-induced nephropathy than the general population.
Objective. The cost effectiveness of iso and low-osmolality contrast media was assessed in high risk outpatients.
Materials and methods. The analysis was based on a systematic literature review comparing the nephrotoxic effects of iso- to low-osmolality contrast media. Only direct costs were considered; these were obtained from the official tariff manual. Incremental cost-effectiveness ratios, efficiency curves and acceptability curves were calculated. Univariate sensitivity analyses were performed for costs and effects, as well as probabilistic analyses. Zero and 3% discounts were applied to results. The cost-effectiveness threshold was equal to the per capita GDP per life-year gained.
Results. Alternatives with Iopamidol and Iodixanol are preferable to the others, because both reduce risk of contrast-induced nephropathy and are less costly. The incremental cost-effectiveness of the Iodixanol alternative compared to the Iopamidol alternative is US$ 14,660 per additional life year gained; this is more than twice the threshold.
Conclusion. The low-osmolality contrast medium, Iopamidol, appears to be cost-effective when compared with Iohexol or other low-osmolality contrast media (Iopromide, Iobitridol, Iomeprol, Iopentol and Ioxilan) in contrast-induced nephropathy, high-risk outpatients. The choice of the iso-osmolality contrast medium, Iodixanol, depends on its cost per vial and on the willingness to pay.
Key words: contrast media; kidney tubular necrosis, acute; cost-benefit analysis.
Costo-efectividad de medios de contraste isoosmolales e hiposmolales en pacientes con alto riesgo de nefropatía inducida por medio de contraste
Introducción. Los medios de contraste pueden provocar falla renal aguda por toxicidad directa sobre las células tubulares e isquemia medular renal. Los pacientes diabéticos y los hospitalizados presentan mayor riesgo de desarrollar nefropatía inducida por medios de contraste que la población general.
Objetivo. Establecer el costo-efectividad de los medios de contraste isosmolales e hiposmolales en pacientes con alto riesgo.
Materiales and métodos. El análisis se basó en una revisión sistemática de la literatura científica, comparando los efectos nefrotóxicos de los medios isosmolales e hipoosmolales. Se consideraron sólo los costos directos, obtenidos del manual tarifario. Se calcularon las tasas del incremento del costo-efectividad, las curvas de eficiencia y de aceptabilidad. Se hicieron análisis univariados de sensibilidad para costos y efectos, así como probabilísticos. Se aplicaron tasas de descuento de 0 y 3 % a los resultados. Se usó como umbral de costo-efectividad por año de vida ganado, el producto interno bruto per cápita.
Resultados. Las alternativas con Iopamidol y Iodixanol dominan a las demás porque reducen el riesgo de nefropatía inducida por contraste a un menor costo. La razón del incremento del costo-efectividad del iodixanol comparado con el iopamidol es de US$ 14.660 por año de vida ganado que más que duplica el umbral.
Conclusión. El medio de baja osmolalidad, iopamidol, parece ser costo-efectivo comparado con iohexol u otros medios hiposmolares (iopromide, iobitridol, iomeprol, iopentol y ioxilan), en pacientes con alto riesgo de nefropatía inducida por contraste. La elección del medio hiposmolar, depende de la disponibilidad a pagar o del costo por ampolleta.
Palabras clave: medios de contraste, necrosis tubular aguda, análisis costo-eficiencia.
Contrast-induced nephropathy (CIN) is defined by the European Society of Urogenital Radiology as an increase in serum creatinine by more than 25% or 44 mmol/L (0.5 mg/dL) within 3 days after the intravascular administration of contrast medium, without an alternative etiology (1). CIN is one of the main etiological factors of acute kidney failure in hospitalized patients. It is also an important cause of morbidity, mortality, high cost and long hospital stays. Incidence of CIN in the general population is lower than 2% (2). Risk factors for CIN include pre-existing renal impairment, diabetes, dehydration, allergies and advanced age. In patients with high risk of CIN, such as diabetics with kidney damage, CIN occurs in 12%-50% of the cases (3). CIN is the third most common cause of kidney failure in hospitalized patients, being the putative cause in 12% of cases (4).
High-osmolality contrast media have more than 2-3 times the osmolality of plasma, low osmolality media have up to 2-3 times the osmolality of plasma; iso-osmolality contrast media have a similar osmolality to plasma. Low-osmolality contrast media include Gatoteridol, Iohexol, Ioversol, Metrizamide and Iopamidol; Iodixanol belongs to the iso-osmolality group.
Contrast media cause nephrotoxicity by direct toxicity upon the tubular cells and kidney ischemia. Meta analyses have found that the use of non-ionic low-osmolality media decreases CIN risk in high risk patients, compared to high-osmolality ionic media (5,6). For diabetic patients with medium to moderate kidney failure (i.e., with high risk of CIN), a recent randomized clinical trial found that an iso-osmolality contrast media (Iodixanol) decreases CIN risk compared to a low-osmolality contrast media (Iohexol) (7).
Based on these results, iso-osmolality media may cause fewer kidney failure episodes than low-osmolality media. However, media differ in other features, such as ionicity, viscocity and molecular size. Each can contribute to differing risk profiles for kidney failure, even though each may have the same osmolality (8).
In addition to variability in nephrotoxic effects, contrast media vary in their costs. Herein, the cost effectiveness of iso and low-osmolality contrast media is assessed for outpatients with high CIN risk.
Materials and methods
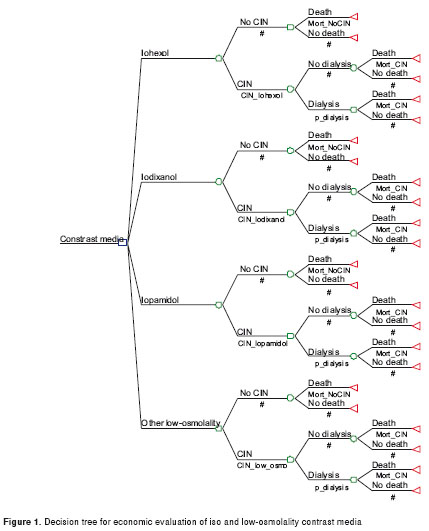
In order to assess the cost-effectiveness of contrast media in outpatients with high CIN risk, a decision tree model was used (figure 1). The alternative media assessed were (1) iohexol, (2) iopamidol, (3) iodixanol, and (4) other low osmolality media (Iopromide, Iobitridol, Iomeprol, Ioxaglate, Iopentol and Ioxilan). Effectiveness was measured in life years gained--as QALYs (quality-adjusted life year) have not been calculated for this case for Colombia. The effects (death due to NIMC) are immediate, but if the patient survives, he/she is assumed to survive to full life expectancy. Hence, the time horizon is the expectancy of life—a period assumed to lie between the life expectancy at birth (74 years in Colombia) and 84. Life years gained were calculated as the life expectancy minus the average age of the patients (assumed to be 63 years). The results and costs were calculated with 0% and 3% discounts. The threshold for cost effectiveness was the Colombian per capita GDP, US $5,356.
Clinical data
Probabilities were extracted from a systematic review of the literature performed by the Department of Radiology and Diagnostic Images, Faculty of Medicine, Universidad Nacional de Colombia, following the instructions of the Method Group for Clinical Practice Guidelines (CPG 2010) (9) in the development of the CPG for the use of contrast media in radiologic procedures. From this revision, information was taken on CIN risk for each of the contrast media (8,10,11). Data on secondary mortality were extracted from published observational studies and economic analyses (12-14).Data used in the model, as well as the sensitivity analyses intervals appear in table 1.
Cost data
The perspective was that of the third payer (costs incurred by Colombian National Health System). Only direct costs related to contrast media, and the handling of renal complications resulted from them, were taken into account (table 2). Prophylaxis costs were not included, although these costs do not alter the incremental cost-effectiveness ratio (ICER) as they were the same for both alternatives. Costs of contrast media were market prices; the cost of handling complications was calculated according to official rates in SOAT (SOAT is the Colombian tariff handbook for drugs and medical procedures). Costs were expressed in US dollars at official exchange rate of December 31, 2009 (2,044.23 Col pesos per US dollar).
Analysis
ICER, efficiency curves, and acceptability curves were calculated, comparing each alternative to the Iopamidol strategy. Univariate sensitivity analyses were performed for costs and effects, as well as a probabilistic analysis with the distributions of the variables extracted of the literature.
Results
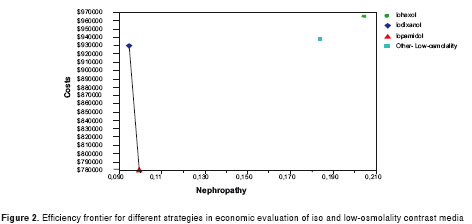
Results of the analyses appear in table 3 and table 4. Alternatives with Iopamidol and Iodixanol were the preferred alternatives compared with iohexol or other low-osmolality contrast media, as they were less expensive and more effective in reducing CIN risk and gaining life years. With a 3% discount (table 3), the cost of the iodixanol alternative compared to the iopamidol alternative was US $15,476 per additional avoided nephropathy and $14,660 for additional life-year gained (almost three times the threshold). With 0% discount (table 4) the ICER of Iodixanol compared to Iopamidol was $6,216.77, which again was higher than the threshold. Without discount, Iopamidol still was the preferred outcome over Iohexol and other low osmolality media.
The efficiency frontier appears in figure 2. The Iopamidol and Iodixanol alternatives were on the efficiency line, whereas the others were above this line. Choice of preferred strategy depends on willingness to pay (WTP). The Iodixanol alternative was cost-effective for a WTP higher than US $14,660 per life-year gained. This corresponds to a budget higher than US $455 per avoided additional CIN. Iopamidol was considered cost-effective for a lower budget.
Univariate sensitivity analyses
In the one-way sensitivity analyses for clinical data, the main variables affecting results were as follows: the risk of CIN with iopamidol, hospitalization days, life expectancy and the probability of requirement of dialysis for patients with CIN. However, the only variable with an impact on decision was the risk of CIN with iopamidol: if it became higher than 0.11, this alternative would be dominated by Iodixanol.
In the one-way sensitivity analyses for costs, the variables with higher impact were the hospitalization costs and the price of the contrast media. Iopamidol became less cost-effective when price per 50 ml vial was higher than US $51; Iodixanol became cost-effective when the price for 50 ml vial was lower than $28. Hospitalization days affected total costs, but not the decision. Iohexol and other low osmolality media were preferable at any price. Life expectancy does not affect the results.
Probabilistic sensitivity analysis
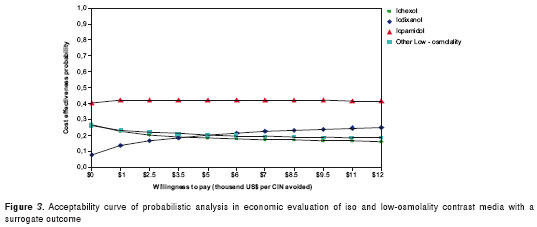
As can be seen in the acceptability curve (figure 3), the iopamidol alternative is more likely to be cost-effective, followed by the iodixanol alternative, within the willingness-to-pay range of US $0 to $11,740.
Discussion
The economic burden of CIN is important and the adoption of targeted interventions reducing CIN incidence are relevant. Patients who develop CIN are more likely to experience adverse events, to undergo prolonged dialysis, to have longer hospital and intensive care unit stays and to have higher mortality rates. One study has estimated that the average in-hospital cost of CIN is higher than US $10,345 and the 1-year cost of treating a patient with CIN is US $11,812 (15).
Several strategies have been developed for reducing the risk of CIN, including the prophylactic use of N-acetylcysteine, theophylline, sodiumbicarbonate, HMG Co-A reductase inhibitors, ascorbic acid,fenoldopam, diuretics, and saline or half saline media (16-18). Moreover, new techno-logical developments have resulted in progressive improvement in the safety and tolerability of iodinated contrast media, especially for patients at risk for contrast-associated complications. Clinical trials have demonstrated an improved safety profile for low-osmolality contrast media compared with high-osmolality contrast media in terms of CIN risk (6,19,20).
In the Colombian setting, the alternative with Iopamidol was cost-effective in the prevention of contrast-induced acute nephropathy, because Iopamidol has lower cost and higher effectiveness when compared with Iohexol and other low-osmolality contrast media strategies. On the other hand, the alternative with Iodixanol is cost-effective if the budget per patient was higher than US $455 or the cost of the 50 ml vial lower than US $28. Also, Iodixanol became cost effective when a higher threshold was used, i.e., three times the per capita GDP.
The dependence of the cost-effectiveness of Iodixanol on willingness-to-pay (WTP) in a developing country was in agreement with the result for developed countries, which have higher WTP. An economic analysis conducted for 17 European hospitals showed that Iodixanol appeared to be cost-effective when compared with Iohexol in diabetic patients with renal impairment undergoing angiography (21), although this study measured effectiveness in terms of adverse drug reactions avoided. No previous studies of the cost-effectiveness of contrast media in the prevention of CIN in a developing country setting were found in a the review of the literature. Only one study evaluated the cost-effectiveness of contrast media in a European country in CT examination (22). The authors found that the net differential cost between universal and selective use of low-osmolality contrast medium was US $43.90 per patient when all outcomes were considered. The selective alternative (low-osmolality in only CIN high risk patients) was safe and effective, and resulted in a substantial reduction in costs.
A limitation of the present analysis was that the difference in the probability of nephropathy between Iopamidol and Iodixanol were very small and not statistically significant. Therefore, the incremental effectiveness of Iopamidol strategy was also small, and hence, the interpretation of the ICER is subject to discussion. However, the difference with the other two alternatives was statistically significant, and the analysis performed permitted their assessment. If the focus was only on Iopamidol and Iodixanol, and the probability of nephropathy considered to be equal, a cost minimization exercise is recommended. If the information provided here were to be interpreted in this way, Iopamidol remains to be preferred over Iodixanol, since the total costs of its use are lower.
Another approach is to focus on a surrogate (cases of CIN avoided), rather than on life years. CIN is recognized to have possible long-term consequences, even leading to increased morbidity and mortality (3,23); however, the information on the cost of avoiding an additional case of CIN may be of greater importance in some contexts. figure 3 shows that when the acceptability curve was calculated in terms of avoided CIN, the results became consistent. This information is useful if the preferred a cost benefit analysis focused on the monetary costs of treating a CIN. In this case (given that the cost of treating a CIN case is approximately US $11,000), figure 3 indicates Iopamidol as the better alternative on a cost benefit basis. These comparisons suggest that the results are robust to different foci and preferences regarding the type of economic analysis.
Conflict of interests
All authors declare no conflicts of interests.
Financing
This economic analysis was carried out under the project “Clinical Practice Guidelines for the University Hospital”, led by the Instituto de Investigaciones Clínicas at the Faculty of Medicine and funded by the Universidad Nacional de Colombia.
Corresponding author: Mario García-Molina, Escuela de Economía, Facultad de Ciencias Económicas, Universidad Nacional de Colombia, Carrera 30 N° 45-03, edificio 311, oficina 306, Bogotá, D.C., Colombia. Phone and fax number: (571) 316 5000, ext. 16809 mgarciamo@unal.edu.co
References
1. Thomsen HS, Morcos SK. Contrast media and the kidney: European Society of Urogenital Radiology (ESUR) guidelines. Br J Radiol. 2003;76:513-8. [ Links ]
2. Berg KJ. Nephrotoxicity related to contrast media. Scand J Urol Nephrol. 2000;34:317-22. [ Links ]
3. Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259-64. [ Links ]
4. Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930-6. [ Links ]
5. Barrett BJ, Carlisle EJ. Metaanalysis of the relative nephrotoxicity of high- and low-osmolality iodinated contrast media. Radiology. 1993;188:171-8. [ Links ]
6. Taliercio CP, Vlietstra RE, Ilstrup DM, Burnett JC, Menke KK, Stensrud SL, et al. A randomized comparison of the nephrotoxicity of iopamidol and diatrizoate in high risk patients undergoing cardiac angiography. J Am Coll Cardiol. 1991;17:384-90. [ Links ]
7. Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Berg KJ. Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med. 2003;348:491-9. [ Links ]
8. Solomon R. The role of osmolality in the incidence of contrast-induced nephropathy: A systematic review of angiographic contrast media in high risk patients. Kidney Int. 2005;68:2256-63. [ Links ]
9. Pardo R, editor. Manual metodológico para la elaboración y adaptación de guías de práctica clínica basadas en la evidencia. 1ª edición. Bogotá: Universidad Nacional de Colombia; 2010. [ Links ]
10. Nguyen SA, Suranyi P, Ravenel JG, Randall PK, Romano PB, Strom KA, et al.Iso-osmolality versus low-osmolality iodinated contrast medium at intravenous contrast-enhanced CT: Effect on kidney function. Radiology. 2008;248:97-105. [ Links ]
11. Solomon R, Dumouchel W. Contrast media and nephropathy: Findings from systematic analysis and Food and Drug Administration reports of adverse effects. Invest Radiol. 2006;41:651-60. [ Links ]
12. From AM, Bartholmai BJ, Williams AW, Cha SS, McDonald FS. Mortality associated with nephropathy after radiographic contrast exposure. Mayo Clin Proc. 2008;83:1095-100. [ Links ]
13. Klarenbach SW, Pannu N, Tonelli MA, Manns BJ. Cost-effectiveness of hemofiltration to prevent contrast nephropathy in patients with chronic kidney disease. Crit Care Med. 2006;34:1044-51. [ Links ]
14. Caicedo MA. Nefropatía por medios de contraste. Acta Med Colomb. 2007;32:68-79. [ Links ]
15. Subramanian S, Tumlin J, Bapat B, Zyczynski T. Economic burden of contrast-induced nephropathy: Implications for prevention strategies. J Med Econ. 2007;10:119-34. [ Links ]
16. Pannu N, Wiebe N, Tonelli M. Prophylaxis strategies for contrast-induced nephropathy. JAMA. 2006;295:2765-79. [ Links ]
17. Thomson VS, Narayanan K, Singh JC. Contrast induced nephropathy in urology. Indian J Urol. 2009;25:437-45. [ Links ]
18. Lee PT, Chou KJ, Fang HC. Preventing contrast-induced nephropathy in patients with baseline renal dysfunction undergoing coronary angiography. Curr Treat Options Cardiovasc Med. 2009;11:71-8. [ Links ]
19. Barrett BJ, Parfrey PS, Vavasour HM, McDonald J, Kent G, Hefferton D, et al. Contrast nephropathy in patients with impaired renal function: High versus low osmolar media. Kidney Int. 1992;41:1274-9. [ Links ]
20. Rudnick MR, Goldfarb S, Wexler L, Ludbrook PA, Murphy MJ, Halpern EF, et al. Nephrotoxicity of ionic and nonionic contrast media in 1196 patients: A randomized trial. The Iohexol Cooperative Study. Kidney Int. 1995;47:254-61. [ Links ]
21. Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Lundkvist J. Cost-effectiveness of iodixanol in patients at high risk of contrast-induced nephropathy. Am Heart J. 2005;149:298-303. [ Links ]
22. Valls C, Andia E, Sánchez A, Moreno V. Selective use of low-osmolality contrast media in computed tomography. Eur Radiol. 2003;13:2000-5. [ Links ]
23. Gruberg L, Mehran R, Dangas G, Mintz GS, Waksman R, Kent KM, et al. Acute renal failure requiring dialysis after percutaneous coronary interventions. Catheter Cardiovasc Interv. 2001;52:409-16. [ Links ]













