Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Biomédica
versão impressa ISSN 0120-4157
Biomédica vol.33 no.1 Bogotá jan./mar. 2013
https://doi.org/10.7705/biomedica.v32i4.750
ARTÍCULO ORIGINAL
doi: http://dx.doi.org/10.7705/biomedica.v32i4.750
1Departamento de Medicina, Facultad de Medicina, Universidad Nacional de Colombia, Bogotá, D.C., Colombia
2Unidad de Enfermedades Infecciosas, Facultad de Medicina, Universidad Nacional de Colombia, Bogotá, D.C., Colombia
3Grupo de Enfermedades Infecciosas, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
4Comité de Infecciones Hospitalarias, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
5Departamento de Epidemiología, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
6Laboratorio de Microbiología, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
This work was presented as "Neutropenia febril en el trópico: descripción de hallazgos clínicos, microbiológicos y desenlace en un centro de referencia oncológico" at the XIX Congreso Colombiano de Medicina Interna, Cartagena, Colombia, 16 a 19 de octubre de 2006.
Author contributions:
Jorge A. Cortés and Sonia I. Cuervo participated in the design, execution and analysis of this work.
Patients were followed by Jorge A. Cortés, Sonia I. Cuervo, together with Diana Bermúdez, who also contributed to the analysis.
Carlos Gómez and Jorge A. Cortés wrote the first draft.
Teresa Martínez participated in the design of the study and statistical analysis of the data.
Patricia Arroyo performed the microbiological studies. All authors reviewed and approved the final version of this manuscript.
Recibido: 14/09/11; aceptado:24/08/12
Introduction. Febrile neutropenia is a common complication of chemotherapy treatment of malignant hematological diseases. However, there is insufficient information regarding the infectious complications of febrile neutropenia in our country.
Objective. We will evaluate the microbial characteristics of bacterial and fungal isolates and the clinical outcome of patients with febrile neutropenia who received medical attention at an oncological reference center in Colombia.
Materials and methods. A prospective case series included patients with histologically confirmed oncological disease, who were admitted because of febrile neutropenia or presented with febrile neutropenia during hospitalization. Patients with benign hematological diseases were excluded. Demographic, microbiological, and clinical features as well as treatment and outcome information from patients with febrile neutropenia were obtained. We performed univariate and multivariate analyses, with mortality defined as the outcome.
Results. One hundred and thirty episodes of febrile neutropenia were identified in 104 patients. The mean patient age was 19, and 53% of the patients were male. Approximately 86% of the episodes occurred in patients with hematological disorders. An infectious site was identified in 65% of patients; 41% and 24% of the febrile neutropenia pateints´ episodes exhibited a localized infectious focus and developed bloodstream infections, respectively. The majority of infections were found in blood, urine, gastrointestinal tract, and soft tissue. Distribution analysis of microbiological isolates revealed 46.4% Gram-negative bacilli, 38.4% Gram-positive cocci, 8% fungi, and 7.1% parasites; there was a 7.7% mortality rate. Appropriate empirical antimicrobial therapy was a protection-related factor in multivariate analyses (OR= 0.17; 0.034 – 0.9 95% CI; p= 0.037).
Conclusions. The mortality rate was relatively low and comparable to the rate reported by developed countries. Inappropriate empirical antimicrobial therapy was the main factor associated with mortality.
Keywords: Neutropenia/microbiology, neutropenia/mortality, neoplasm/complications, antineoplastic agents/adverse events, Colombia.
doi: http://dx.doi.org/10.7705/biomedica.v32i4.750
Neutropenia febril en el trópico: una descripción de los hallazgos clínicos y microbiológicos y el impacto de la terapia inapropiada que utilizan en un centro de referencia oncológica en Colombia
Introducción. La neutropenia febril es una complicación frecuente de la quimioterapia para las neoplasias hematológicas. Se dispone de escasa información de sus complicaciones infecciosas en nuestro medio.
Objetivo. Evaluar las características clínicas y microbiológicas de pacientes con neutropenia febril, así como su resultado clínico en una institución de referencia oncológica en Colombia.
Materiales y métodos. Se conformó prospectivamente una serie de casos con pacientes con enfermedad oncológica confirmada, que consultaron o presentaron neutropenia febril durante la hospitalización. Se excluyeron aquellos con enfermedad hematológica benigna. Se recolectaron datos sobre variables demográficas, microbiológicas, clínicas, de tratamiento y de resultado de los pacientes. Se llevaron a cabo un análisis univariado y uno multivariado, con la mortalidad como resultado.
Resultados. Se identificaron 130 episodios de neutropenia febril en 104 pacientes, con una edad media de 19 años y 53 % masculinos. El 86 % de los episodios ocurrieron en pacientes con alteraciones hematológicas. Se demostró infección en 65 % de los casos: 41 % con un foco infeccioso localizado y 27,7 % con bacteriemia. Los principales focos infecciosos se localizaron en el torrente sanguíneo, el aparato urinario, el sistema gastrointestinal, la piel y los tejidos blandos. De los aislamientos microbiológicos, 46,4 % fueron bacilos Gram negativos, 38,4 %, cocos Gram positivos, 9 %, hongos y, 7,1%, parásitos. La mortalidad global fue de 7,7 %. En el análisis multivariado la utilización de un tratamiento empírico apropiado se correlacionó con una menor mortalidad, de forma independiente (OR=0,17; IC 95% 0,034-0,9; p=0,037).
Conclusiones. La tasa de mortalidad fue relativamente baja y fue comparable con lo reportado en países desarrollados. El tratamiento antimicrobiano inapropiado fue el principal factor asociado con mortalidad.
Palabras clave: neutropenia/microbiología, neutropenia/mortalidad, neoplasias/complicaciones, antineoplásicos/efectos adversos, Colombia
doi: http://dx.doi.org/10.7705/biomedica.v32i4.750
Approximately 50% of febrile neutropenic patients have an established or developing infection, whereas 20% of patients with a neutrophil count of less than 100 cells per milliliter have established bacteremia (1). The risk of death associated with febrile neutropenia (FN) has been considerably reduced during the last few years due to advances in diagnostic methods and broad-spectrum antibiotic therapies. Mortality over a 30-day period currently ranges from 6% to 10% among patients suffering from FN and bacteremia (2).
The clinical outcome for a patient suffering from FN is dependent on several factors; these include the patient´s underlying disease, age, clinical condition at the beginning of the clinical picture, number of infectious foci present, duration of the neutropenia, onset of antibiotic or antifungal therapy, geographical location and local antimicrobial resistance profiles (3). These antimicrobial resistance profiles have gained importance, as these patients are at risk of acquiring community or nosocomial infections. The microbiological findings offer valuable information about the most frequent etiological agents, antimicrobial resistance profiles, and the prevalence of the least frequent microbiological isolates. The clinical findings based on exhaustive physical examinations guide diagnostic and therapeutic efforts aimed at identifying non-apparent infectious foci.
A series of prospective studies carried out in an oncological reference center in Colombia is presented. Our study evaluated clinical and microbiological findings, treatment, and important clinical outcomes for patients suffering from cancer and FN.
Materials and methods
Population: We studied a series of prospective cases from February to August 2003, which included patients who were admitted because of FN or were hospitalized at the moment of the identification of FN at the Instituto Nacional de Cancerologia in Bogotá, Colombia.
Inclusion criteria: We accepted patients of all ages diagnosed with oncological disease who were confirmed by histology and who met the criteria for FN at admission or during hospitalization.
Exclusion criteria: Patients suffering from FN who had not received chemotherapy or showed benign hematological pathology were excluded.
Procedure: Potential patients were identified by hemograms in the hematology laboratory. An active search identified patients suffering from FN, and clinical histories were gathered from medical records after patients with FN were identified. Information included demographic data, clinical diagnosis, risk factors present at the onset of neutropenia, such as invasive devices and prolonged hospital stay, state of oncological disease at the occurrence of neutropenia, and FN severity.
Data such as clinical manifestations, infectious foci present, microbiological findings, and empirical antibiotic therapy were collected at the time of FN diagnosis. The patients were followed during the FN period. Differences in neutropenia duration, changes in microbiological findings, antibiotic therapy adjustment, neutropenia resolution, and the patient´s state at the time of discharge were also recorded.
Microbiological information was obtained from the institution´s microbiology laboratory. Hemocultures and urocultures were routinely collected at the time of admission to the emergency room or following FN diagnosis. Other samples were collected if the attending physician considered it necessary during the patient´s hospitalization. All isolates were processed and identified using automated identification cards (MicroScan, Dade Behring, USA). Interpretations were made according to Clinical and Laboratory Standards Institute ( CLSI )´s criteria (2005).
Definitions: A definition of neutropenia included an absolute neutrophil count of less than 500 cells per milliliter or less than 1,000 cells per milliliter with a downward trend over time. Fever was defined as a single measurement of auxiliary temperature greater than 38.3ºC or greater than 38ºC for more than one hour. State of base disease : Active or in remission. FN severity : severe: absolute neutrophil count (ANC): = 100 cell/ml. Slight-moderate: ANC >100 cell/ml and =1 000 cell/ml or a decreasing tendency.
The following definitions were taken into account when classifying patients according to infection focus. Clinical sepsis: a systemic inflammatory response syndrome without clinical or microbiological findings, revealing an infectious focus. Local focus : local infection as evidenced by clinical or microbiological findings without dissemination into the bloodstream. Primary bacteremia: a microbiological isolate from the bloodstream without documentation of any other local focus of infection. Secondary bacteremia: microbiological isolate from the bloodstream concomitant with a microbiological isolate or clinical findings regarding local infection. Appropriate empirical antibiotic therapy : suitable antibiotic coverage for 72 hours following the identification of a microbiological isolate with identified suceptibility. Prolonged hospital stay : an in-hospital stay longer than 7 days.
Clinical management: At the time of the study, rutine antimicrobial prophylaxis was not used among neutropenic patient or patients receiving chemotherapy. Empirical treatment for patients with febrile neutropenia included cefepime or piperacillin-tazobactam, as first line. Patients with persistent fever were started on meropenem and antifungal therapy was added. Antimicrobial adjustment was performed when appropiate cultures showed a causative microorganism.
Statistical analysis: Data were processed using SPSS software (version 11.5). P values were calculated using Fischer´s exact test for discrete variables and Student´s test for continuous variables. Variables with a p value = 0.1 for univariate analysis were included in a multivariable logistical regression model with mortality outcome.
Ethical considerations
This is an observational study using data from medical records and laboratory findings collected from an institutional program with patients diagnosed with FN. No ethical approval was required.
Results
A total of 130 episodes of fever were identified in 104 neutropenic patients during the study period. Patients´ age ranged from 6 months to 75 years (average age of 19 years). Fifty-five (53%) patients were male. Eighty-nine patients (85.6%) presented with hematological neoplasia as the underlying oncological disease. Seventy-eight (75%) patients presented with a single episode, 23 (22%) presented with 2 episodes, and 3 patients (3%) presented with 3 episodes of FN.
The underlying oncological disease was active during 86 (66%) of FN episodes. FN was severe in 106 (81.5%) episodes. Prolonged hospital stay was associated with 41 (31.5%) episodes of FN. The average duration of neutropenia was 8 days, with a range of 2 to 42 days (table 1).
Infectious foci were identified in 85 (65%) of FN episodes. An infectious focus could not be identified in 45 (35%) episodes of FN, as those patients only presented signs of systemic inflammatory response syndrome (SIRS). At least one clear focus of infection was identified by clinical and/or microbiological procedures without confirmed bacteremia in 49 (37.7%) episodes of FN. Bloodstream infection, central venous catheter-associated bacteremia, primary bacteremia, and bacteremia with an infectious focus were documented in 36 cases (27.7%) (table 2).
The main infectious foci were bacteremia (27.7%), urinary tract infections (19%), gastrointestinal tract infections (19%), cellulitis (15%), oropharynx infections (mucositis and oral herpes) (12%), pneumonia (6%), and other foci (including sinusitis) representing less than 5%.
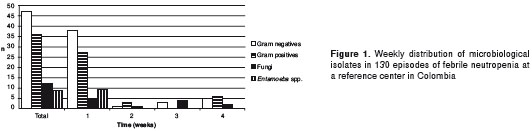
A total of 112 microbiological isolates were identified and included bacteria, fungi, and amoebas. These isolates included 52 Gram-negative bacilli (46.4%), 43 Gram-positive cocci (38.4%), 9 fungi (8%) and 8 Entamoeba histolytica/dispar (7.1%) (table 3). The most frequent isolate was Escherichia coli (21 isolates in urine and 13 isolates in blood cultures), followed by Staphylococcus aureus (7 isolates in blood cultures) and Klebsiella pneumoniae (5 isolates in blood and 3 in urine cultures). Although 9 fungal isolates were identified, only 1 isolate was identified in blood ( Candida albicans ) and one isolate in a skin biopsy (disseminated candidiasis); 6 isolates were detected in urine ( C. albicans , C. tropicalis and other yeast), and one in a bronchoalveolar lavage, representing most likely colonization instead of truely infection. No filamentous fungi were identified. Microbiological isolate distribution changed over the course of an episode of febrile neutropenia; 79 (76%) of all microbiological isolates were collected during the first week of FN (Gram-negative bacilli represented 48% of all isolates). E. histolytica isolates were detected during the first week of FN and were isolated from patients with diarrhea as the sole clinical symptom. Figure 1 shows the distribution of microbiological isolates during the course of FN.
It is worth noting that an analysis of resistance profiles of Gram-negative bacilli during an FN episode revealed an increase in b -lactamase-(ESBL) extended spectrum and meropenem-mediated resistance among isolates during weeks 2, 3, and 4, compared with the first week. Resistance to third-generation cephalosporins in Gram-negative bacilli during the first week of FN was 26% and increased to 33% during weeks 2, 3, and 4 (p=0.69). Meropenem-resistance was observed in 3% of isolates during the first week of FN and in 22% of isolates during weeks 2, 3, and 4 (p=0.08). Eight percent of Gram-negative bacilli were resistant to quinolone. All Pseudomonas aeruginosa isolates were identified during the first week of FN. There was no difference in resistance profiles during the FN period among Gram-positive cocci, including S. aureus . Methicillin-resistant S. aureus represented 66% of S. aureus the isolates. No vancomycin-resistant microorganism was identified in this study.
Ten patients died from FN, which represents a 7.7% mortality rate (deaths per episode); 50% of patients who died received inappropriate empirical antibiotic therapies compared with only 13% in surviving patients.
Based on the univariate analysis, acquiring secondary bacteremia was associated with increased mortality (p=0.01), whereas receiving appropriate empirical antibiotic therapy was a mortality protection-related factor (p<0.001). In the multivariate analysis, receiving appropriate empirical antibiotic therapy was the sole significant variable that acted as a protection-related factor (OR= 0.17; 0.034–0.9 95%CI; p= 0.037).
Discussion
Febrile neutropenia is a frequent complication of chemotherapy, especially among patients diagnosed with malignant hematological disease. A significant percentage of FN episodes are associated with infection and infection is one of the main causes of mortality in cancer patients (2). The characteristics of microbiological isolates in FN patients have changed over the past 25 years, and Gram-positive cocci are currently the predominant group. This could be explained by the use of new antibiotics, the extended use of antibiotic prophylaxis, and increased invasive device-related infections (4-6).
Gram-negative bacilli (GNB), especially E. coli and other enterobacteria, constituted the most common group of isolates found among all the isolates identified and during the first week of FN. In contrast, studies from developed countries reported a predominance of Gram-positive cocci among FN isolates (7). We postulated that these differences are due to the absence of antibiotic prophylaxis in our setting. A previous study showed that administering antibiotic prophylaxis with levofloxacin to neutropenia patients following chemotherapy reduced the episodes of fever and bacteremia caused by GNB; no impact on mortality was evident (8). Data from Venezuela (9), Chile (10), and Taiwan (11) reflect a similar trend in the frequency of Gram-negative isolates.
It is an unusual finding that amoebas, which cause colitis and diarrhea, represented 8% of all microbiological isolates. This trend is usually observed in countries with high E. histolytica/dispar infection prevalence and has been previously described in cancer and immunosuppressed patients in our setting (12,13). E. histolytica/dispar infections were present during the first week of FN, suggesting that these infections are opportunistic. The accuracy of diagnosis (because Entamoeba is easily mistaken for blood-loaded macrophages) and the clinical impact of Entamoeba spp . findings are not clear.
The characterization of antibiotic resistance profiles revealed a trend toward increased meropenem- and ESBL-mediated resistance among GNB during FN. Although not statistically significant, this data indicate the emergence of resistance mechanisms against the first-line if antibiotics used to treat FN. The high frequency in our data of GNB isolates resistant to third-generation cephalosporins is worth noting (28%). This finding has significant implications for other empirical antibiotic therapies (e.g., fourth-generation cefepime was used in our center at the time of the study). Although cefepime is not a strong ESBL inducer (in contrast to third-generation cephalosporins), the high prevalence of GNB with ESBL indicates that improvements in isolation and infection control is essential to avoid the further spread of antibiotic resistance. Several studies have previously highlighted the implications of ESBL-carrier GNB isolates in patients with cancer and FN. GNB are characterized by the easy dissemination among patients in oncological units and their association with increased mortality (14,15).
Another important fact related to antibiotic resistance is the low rate of resistance to antibiotics rarely used for our patients with FN. Quinolone-resistance was only observed in 8% of GNB isolates in our study. In contrast, the rates of resistance in other hospital units in Colombia, such as in intensive care units, varied between 22% and 31% over the past few years (16). The extended use of quinolones leads to the development of resistance in E. coli and S. epidermidis as well as the selection of methicillin-resistant Staphylococcus aureus (MRSA) (17,18). The role of antibiotic prophylaxis is still controversial because little is known regarding how long prophylaxis remains effective following its administration (i.e., there is currently no convincing evidence on the impact on antibiotic resistance rates among isolates from FN patients after several cycles of chemotherapy). Studies evaluating Gram-positive resistance rates to the latest-generation quinolones (moxifloxacin and gatifloxacin) in patients with hematological disease who have been submitted to antibiotic prophylaxis with quinolones such as ciprofloxacin or levofloxacin, have shown selection of multi-resistant Gram-positives, such as MRSA and methicillin-resistant Staphylococcus epidermidis (MRSE) (19). These findings suggest an increase in and selection for multi-resistant Gram-positive isolates that are caused by the use of quinolones as antibiotic prophylaxes.
Pseudomonas aeruginosa infections are a major concern in immunosuppressed patients, as these patients have multiple risk factors that make them more susceptible to colonization and infection by this microorganism (20). Only 3% of the episodes in our study involved P. aeruginosa bacteraemia, all of which occurred during the first week of FN. This is a similar result to those reported by other studies (21). Maschmeyer, et al ., reported that the prevalence of P. aeruginosa bacteremia is 5%-12% among patients with FN (20). Such findings establish P. aeruginosa as an infrequent microorganism in patients with cancer and FN, representing less than 10% of the total isolates in previous studies
The absence of an appropriate empirical antibiotic therapy was the only risk factor associated with mortality in multivariate analysis. A recent study highlighted the relationship between the presence of bacteria with multiple resistance mechanisms and increased mortality when compared with isolates from multi-sensitive microorganisms. Increased mortality was related to the failure of empirical antibiotic therapy to provide suitable coverage against microorganisms with multiple resistance mechanisms (22). We thus found that initiating the appropriate empirical antibiotic therapy was the main protection-inducing factor against mortality in this study, which should be supported by findings from local resistance profiles.
Sixty percent of patients who died had not received appropriate empirical antibiotic-therapies. This fact highlights the importance of administering the appropriate antibiotics according to local resistance profiles and the patient´s clinical symptoms during the first hours of FN.
Mortality in patients with FN is therefore linked to suitable empirical antibiotic coverage, depending on the antimicrobial resistance profiles in various hospitals. Further studies are needed to evaluate the microbiological findings and the prevalence of local resistance profiles. This will enable institutions to determine the most appropriate empirical antibiotic therapy and to document atypical pathogens, such as those prevailing in tropical areas.
There is no specific founding source. This work was supported by Universidad Nacional de Colombia (JAC, SIC) and Instituto Nacional de Cancerología (DB, TM, PA).
No competing interests were declared by the authors.
Corresponding author: Jorge Alberto Cortés, Departamento de Medicina (oficina 510), Facultad de Medicina, Universidad Nacional de Colombia, Ciudad Universitaria, Bogotá, D.C., Colombia. Phone: (571) 269 2662; fax: (571) 316 5000, extensión 15012 jacortesl@unal.edu.co
1. Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al . Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America . Clin Infect Dis. 2011;52:427-31. http://dx.doi.org/10.1093/cid/ciq147 [ Links ]
2. Viscoli C, Varnier O, Machetti M. Infections in patients with febrile neutropenia: Epidemiology, microbiology, and risk stratification . Clin Infect Dis. 2005;40(Suppl.4):S240-5. http://dx.doi.org/10.1086/427329 [ Links ]
3. Rolston KV. Challenges in the treatment of infections caused by Gram-positive and Gram-negative bacteria in patients with cancer and neutropenia . Clin Infect Dis.2005;40(Suppl.4):S246-52. http://dx.doi.org/10.1086/427331 [ Links ]
4. Viscoli C. The evolution of the empirical management of fever and neutropenia in cancer patients . J Antimicrob Chemother.1998;41(Suppl.D):65-80.http://dx.doi.org/10.1093 /jac/41.suppl_4.65 [ Links ]
5. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: Emphasis on gram-positive and resistant bacteria . Clin Infect Dis. 1999;29:490-4. http://dx.doi.org/10.1086/598620 [ Links ]
6. Wisplinghoff H, Seifert H, Wenzel RP, Edmond MB. Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States . Clin Infect Dis. 2003;36:1103-10. http://dx.doi.org/10.1086/374339 [ Links ]
7. Oppenheim BA. The changing pattern of infection in neutropenic patients . J Antimicrob Chemother. 1998;41 (Suppl.D):7-11. http://dx.doi.org/10.1093/jac/41.suppl_4.7 [ Links ]
8. Bucaneve G, Micozzi A, Menichetti F, Martino P, Dionisi MS, Martinelli G, et al . Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia . N Engl J Med. 2005;353:977-87. [ Links ]
9. Figuera M, Carballo M, Silva M, Figueredo A, Avilan J. Microbiological isolates in patients with febrile neutropenia and hematological neoplasias . Rev Esp Quimioter. 2006;19:47-51. [ Links ]
10. Rabagliati BR, Fuentes LG, Orellana UE, Oporto CJ, Domínguez MI, Benítez GR, et al . Etiología de episodios de neutropenia febril en pacientes adultos con cáncer hematológico y de órganos sólidos en el Hospital Clínico Universidad Católica, Santiago-Chile . Rev Chilena Infectol. 2009;26:106-13. http://dx.doi.org/10.4067/S0716-10182009000200001 [ Links ]
11. Chen CY, Tsay W, Tang JL, Tien HF, Chen YC, Chang SC, et al . Epidemiology of bloodstream infections in patients with haematological malignancies with and without neutropenia . Epidemiol Infect. 2010;138:1044-51. http://dx.doi.org/10.1017/S0950268809991208 [ Links ]
12. Cardona AF, Combariza JF, Reveiz L, Ospina EG, Poveda CM, Ruiz CA, et al . Clinical and microbiological characteristics of neutropenic enterocolitis in adults with blood cancer in the National Cancer Institute of Bogota D.C. (Colombia) . Enferm Infecc Microbiol Clin. 2004;22:462-6. [ Links ]
13. Botero JH, Castaño A, Montoya MN, Ocampo NE, Hurtado MI, Lopera MM. A preliminary study of the prevalence of intestinal parasites in immunocompromised patients with and without gastrointestinal manifestations . Rev Inst Med Trop Sao Paulo. 2003;45:197-200. http://dx.doi.org/10.1590/S0036-46652003000400004 [ Links ]
14. Siu LK, Lu PL, Hsueh PR, Lin FM, Chang SC, Luh KT, et al . Bacteremia due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a pediatric oncology ward: Clinical features and identification of different plasmids carrying both SHV-5 and TEM-1 genes . J Clin Microbiol. 1999;37:4020-7. [ Links ]
15. Palasubramaniam S, Subramaniam G, Muniandy S, Parasakthi N. SHV-5 extended-spectrum beta-lactamase from Klebsiella pneumoniae associated with a nosocomial outbreak in a paediatric oncology unit in Malaysia . Int J Infect Dis. 2005;9:170-2. http://dx.doi.org/10.1016/j.ijid.2004.07.005 [ Links ]
16. Briceño DF, Correa A, Valencia C, Torres JA, Pacheco R, Montealegre MC, et al . Actualización de la resistencia a antimicrobianos de bacilos Gram negativos aislados en hospitales de nivel III: años 2006, 2007, 2008 . Biomédica. 2010;30:371-81. [ Links ]
17. Cometta A, Calandra T, Bille J, Glauser MP . Escherichia coli resistant to fluoroquinolones in patients with cancer and neutropenia . N Engl J Med. 1994;330:1240-1. [ Links ]
18. Gómez L, Garau J, Estrada C, Márquez M, Dalmau D, Xercavins M, et al . Ciprofloxacin prophylaxis in patients with acute leukemia and granulocytopenia in an area with a high prevalence of ciprofloxacin-resistant Escherichia coli. Cancer. 2003;97:419-24. http://dx.doi.org/10.1002/cncr.11044 [ Links ]
19. Rolston KV, Yadegarynia D, Kontoyiannis DP, Raad, II, Ho DH. The spectrum of Gram-positive bloodstream infections in patients with hematologic malignancies, and the in vitro activity of various quinolones against Gram-positive bacteria isolated from cancer patients . Int J Infect Dis. 2006;10:223-30. http://dx.doi.org/10.1016/j.ijid.2005.05.007 [ Links ]
20. Maschmeyer G, Braveny I. Review of the incidence and prognosis of Pseudomonas aeruginosa infections in cancer patients in the 1990s . Eur J Clin Microbiol Infect Dis. 2000; 19: 915-25. http://dx.doi.org/10.1007/s100960000410 [ Links ]
21. Sigurdardottir K, Digranes A, Harthug S, Nesthus I, Tangen JM, Dybdahl B, et al . A multi-centre prospective study of febrile neutropenia in Norway: Microbiological findings and antimicrobial susceptibility . Scand J Infect Dis. 2005;37:455-64. [ Links ]
22. Giamarellos-Bourboulis EJ, Papadimitriou E, Galanakis N, Antonopoulou A, Tsaganos T, Kanellakopoulou K, et al . Multidrug resistance to antimicrobials as a predominant factor influencing patient survival . Int J Antimicrob Agents. 2006;27:476-81.http://dx.doi.org/10.1016/j.ijantimicag. 2005.12.013, [ Links ]













