Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Biomédica
versão impressa ISSN 0120-4157
Biomédica vol.35 no.3 Bogotá jul./set. 2015
https://doi.org/10.7705/biomedica.v35i3.2598
ARTÍCULO ORIGINAL
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2598
1 Grupo de Patología Oncológica, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
2 Grupo de Tumores Endocrinos, Instituto Nacional de Cancerología, Bogotá, D.C., Colombia
3 Subdirección Nacional de Trasplantes y Bancos de Sangre, Dirección de Redes en Salud Pública, Instituto Nacional de Salud, Bogotá, D.C., Colombia
Author´s contributions:
Alfredo Romero-Rojas confirmed the diagnosis and made the pathological description of cases.
Jairo Cuervo-Martínez carried out data search, collection, organization and analysis.
Karime Osorio-Arango was responsible for data epidemiological analysis.
Natalia Olaya carried out data analysis.
All authors participated in the writing of the manuscript.
Recibido: 04/11/14; aceptado: 11/05/15
Introduction: Thyroid cancer is the most common endocrine neoplasia and the papillary subtype is the most frequent; there are histological and clinical factors associated with a higher risk of recurrence and metastasis.
Objective: The aim of this study was to examine the histological, prognostic and clinical characteristics of papillary thyroid carcinomas diagnosed at the National Cancer Institute of Colombia.
Materials and methods: A retrospective cohort study was carried out on 619 patients with papillary thyroid carcinoma between 2006 and 2012; we analyzed the sociodemographic, histological, prognostic and clinical characteristics.
Results: 87.7% of cases were women. The presence of two or more variants in the same case was considered a particular variant, which we called combined pattern. Combined pattern was then the most frequent (50.9%), followed by the follicular variant (23.4%) including subtypes encapsulated and unencapsulated, and the classic variant (22.1%). Mean tumor size was 20.8 mm. More than half of the cases had capsular invasion, extrathyroidal invasion and lymph node involvement. When compared with the other variants, the combined pattern carcinomas had a higher risk of invasion of the thyroid capsule, extraganglionar invasion and metastasis.
Conclusions: Our results are in many aspects similar to those already reported. However, the presence of the combined pattern implied a higher risk for capsular invasion, nodal involvement, extranodal involvement and metastasis in comparison with those which had just one variant. Further studies are necessary to confirm these results.
Key words: Thyroid gland; thyroid neoplasms; papillary, carcinoma; epidemiology.
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2598
Variantes histológicas y factores pronósticos del carcinoma papilar de tiroides en el Instituto Nacional de Cancerología de Colombia, 2006-2012
Introducción. El cáncer de tiroides es la neoplasia más común y el subtipo papilar es el más frecuente; hay factores histológicos y clínicos asociados con un mayor riesgo de recidiva y metástasis.
Objetivo. Examinar las características histológicas, clínicas y de pronóstico de los carcinomas papilares de tiroides diagnosticados en el Instituto Nacional de Cancerología de Colombia.
Materiales y métodos. Se llevó a cabo un estudio de cohorte retrospectiva que incluyó a 619 pacientes con carcinoma papilar de tiroides entre 2006 y 2012; se analizaron las características sociodemográficas, histológicas, de pronóstico y clínicas.
Resultados. El 87,7% de casos correspondió a mujeres. La presencia de dos o más variantes histológicas en un mismo caso se consideró como una variante a la cual se denominó patrón combinado; esta fue la más frecuente (50,9 %), seguida de la variante folicular (23,4 %), incluidos los subtipos encapsulados o no encapsulado y la variante clásica (22,1 %). El promedio del tamaño tumoral fue de 20,8 mm. En más de la mitad de los casos se evidenció invasión capsular, invasión extratiroidea y metástasis en ganglios linfáticos. Comparados con otras variantes histológicas, los carcinomas con patrón combinado presentaron mayor riesgo de invasión de la cápsula tiroidea, de invasión extraganglionar y de metástasis.
Conclusión. En muchos aspectos los resultados fueron similares a los reportados previamente; sin embargo, se encontró que la presencia del patrón combinado aumentaba el riesgo de invasión capsular, metástasis en nódulos linfoides y extensión extratiroidea en comparación con los que tenían una sola variante. Sería necesario hacer estudios acerca del mecanismo biológico de la diferenciación en células cancerosas con el fin de ahondar sobre este fenómeno.
Palabras clave: glándula tiroides, neoplasias de la tiroides, carcinoma papilar, epidemiología.
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2598
Thyroid cancer is the most frequent of all endocrine neoplasms (1). In Colombia it ranks eighth among all cancers with an incidence rate of 5.1 cases per 100,000 inhabitants (2,3). In general terms, its incidence has increased worldwide, a fact partially related to environmental risk, but also due to the availability of more sensitive diagnosis and tracking technology (1,4-6). Nowadays, small tumors are frequently detected and treated (7,8).
The World Health Organization (WHO) classifies malignant epithelial thyroid tumors into four major groups (papillary, follicular, medullary and undif ferentiated) (9). Papillary thyroid carcinoma (PTC) is the most common type, for about eight out of ten thyroid cancers belong to this histological type (1,4).
PTC is usually an indolent disease with a chronic course. The classic lesion appears as a proliferation of papillary structures lined by cells with eosino philic cytoplasm and enlarged nuclei, superimposed and with irregular contours. Some of these nuclei appear as optically empty or like frosted glass, which is made more evident in the cytological smears; they may have nuclear cleavage, and psammoma bodies can be found (1,9) They grow slowly, usually appear in only one thyroid lobe and often propagate to the neck lymph nodes (1,9).
Furthermore, PTC includes several histological variants which imply lesser or greater degrees of risk (6,10), and which are determined by size, specific growth and stromal reaction patterns; nonetheless, they also preserve specific papillary carcinoma nuclear characteristics (figure 1).

Quantitative criteria to include a particular lesion in one of the variants are not universal (figure 1) (6,10-14). Not one of them includes a method for an objective measure of the amount of each variant contained into a lesion. The College of American Pathologists check list, widely used in the world, recommends mentioning the variants but gives no particular guide for quantification (15).
Cancer registries in Colombia are relatively new and fragmentary. The population-based cancer registry of Cali ( Registro Poblacional de Cali , RPCC) collects information about the new cancer cases occurring in Colombia (16-18). Some studies about the disease have shown an increasing trend in the incidence of papillary carcinoma in women and a slight increase in men (17-19). However, the available information does not include detailed data about histological characteristics in Colombia (17,18). In order to shed light on the subject, we decided to describe the histological and clinical characteristics of the patients in a single institution.
Materials and methods
We conducted a retrospective cohort study which included all patients diagnosed with PTC by the Grupo de Patología Oncológica at the Instituto Nacional de Cancerología , between 2006 and 2012. A systematic and manual review of all pathology reports was carried out in order to ensure that no case would be omitted from the study. Then, all cases were confirmed and reclassified by the pathologist of the group, expert in diagnosing neuroendocrine disease; this allowed for the collection of data on histological variants and tumoral characteristics in accordance with WHO guidelines, the Classification of malignant tumors (TNM), the College of American Pathologists and local clinical guidelines (10,15,20,21).
Variant definition
As there is no universal consensus about the criteria for including a case in a particular PTC variant (1,9,13,21-27), and considering that the assessment of cell percentage is often subjective, we defined combined pattern" as the presence of two or more histological variants in the same case. Each of the composing variants must be represented at least in 30% of tumoral cells. This combined pattern is made up of a predominant subtype, which corresponds to the histological variant with the greatest percentage of tumor cells, and of a secondary subtype, which relates to the subsequent histological variant with the next highest percentage of tumor cells.
Tumor characteristics included as variables of interest were: Thyroid capsule invasion, extrathyroid invasion, vascular invasion, lymph node and extranodal metastasis, tumor size and focality. We are aware of the discrepancy between pathologists concerning the existence of the thyroid capsule (28-30). However, we have included and used the term since our local guidelines include it, and because the concept is still important for a proper TNM classification (20,21,31).
We followed the protocol of the College of American Pathologists for the evaluation of extrathyroid invasion (15,29-31).
Tumor size was categorized into three groups:
1) Papillary microtumor (PMiT), i.e., those which:
a) are unifocal of 10 mm or less,
b) have no metastasis at the time of diagnosis;
c) appear in adult patients;
d) are multifocal and have a diameter that is still less than 10 mm;
e) have no capsular or vascular invasion;
f) are of low risk from a histological stand point, and
g) were non-detectable through imaging (32,33).
2) Microcarcinomas (PMC), i.e., tumors that measure 10 mm or less and have any histological risk factor. Some authors report multifocality percentages ranging from 7% to 56%, a fact which increases recurrence and regional metastasis (5,31,32). In patients with multifocal microcarcinomas when the sum of the diameter of the lesions is greater than 10 mm they are considered carcinomas.
3) Carcinomas, i.e., tumors that measure over 10 mm (30,31).
We defined relapse as the reappearance of the malignant tumor or tumor cells after a treatment. In order to discern relapse in this series a search was carried out through medical records using the SAP information system of medical records; the diagnosis made by the prescribing physician during checkups was taken into account as was the appearance of nodes or metastasis (local, loco- regional or distant) following surgery.
Out of the 619 cases, relapse was analyzed in only 211 given that they were the only cases for which the pathology departments had post-surgery follow- up data. Age and gender were obtained from the medical charts. Age was categorized into groups according to the clinical interest: a) under 18 years of age, b) between 18 and 45 years of age and c) over 45 years of age. All data were included in an excel database (Microsoft Excel).
Statistical analysis
Initially, descriptive statistics were used to perform univariate analysis. Central tendency and dispersion were calculated for quantitative variables. For the remaining variables, calculations were made for absolute, relative and proportional frequencies using SPSS ® 19.1 software.
Later, we performed an analysis of subgroups to observe how the principal histological variants and clinical characteristics behaved according to establishe d gender and groups. The associ ation between tumor characteristics and major histological variants was explored in the bivariate analysis by calculating relative risks (RR) with their respective raw confidence intervals of 95% and taking as significant a value of p<0.05.
Relapse was considered from the time of surgery to December, 2013.
Ethical considerations
This project was approved by the Board of Ethics of the Instituto Nacional de Cancerología .
Results
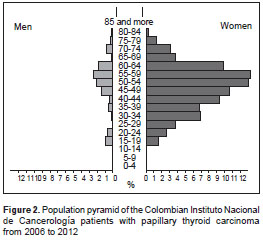
A total of 619 cases of papillary thyroid carcinoma were diagnosed at the Instituto Nacional de Cancerología from 2006 to 2012. Mean age at the time of diagnosis was 51 years (SD=13.95 range 12-82) and most were women (87.7%). Other patient characteristics are shown in table 1. Population pyramid is shown in figure 2.
The most frequent histological variant was the combined pattern (50.9%), followed by the follicular variant (23.4%), the classic variant (22.1%), and in a lesser proportion, the cribriform, fasciitis nodular-like, clear and squamous cell variants (0.2%) each .
Among patients who reported the combined pat-tern, 90.6% included the predominant classic variant in their composition, followed by the follicular variant (4.18%); secondary subtypes included the follicular variant (90.9%) and the solid variant (2.89%).
Data on the histological characteristics of papillary thyroid carcinoma registered median tumor size of 20.8 mm (SD=15.24, range: 1-89). Thyroid capsu lar invasion was present in 78.0% of the cases, e xtrathyroid invasion in 61.8%, lymphovascular invasion occurred in 29.5% and venous invasion in 23.6%. Lymph node metastasis was encountered in 60.1% of cases and extranodal metastasis in 36.5% (table 2).
Distribution by gender revealed that some histo logical variants occurred exclusively among women: clear cell, columnar cell, cribriform cell, diffuse sclerosis, fasciitis-like cell, macrofollicular cell and oncocytic cell variants. In contrast, the predominant histological variants in men were the classic (16.8%) and tall cell (9.1%) variants. The combined pattern occurred in an equal proportion of men and women. The histological variant analysis according to age group revealed that even though PTC may appear at any age, some variables show up more frequently in certain groups (table 2).
When histological variants were related to tumor size, it was observed that the combined pattern was present in most carcinomas (52.3%) and many microcarcinomas (44.1%), in contrast to microtumors, which characteristically had a greater percentage of the classic variant (40%).
We established a relationship between extrathyroid invasion and the type of histological variant since the former is a characteristic which determines tumoral behavior. Results showed a 19.3% and 14% of extrathyroidal invasion for follicular and classic variants respectively, while the combined pattern displayed a 66.7%.
The relapse analysis could only be performed on 211 cases, 83.88% of which had shown no relapse from the time of surgery until the time of inclusion in the study. Among the patients who suffered relapse, 9.95% had loco-regional relapse; 4.26%, distant relapse, and 1.89%, local relapse.
The bivariate analysis of the most common variants and their histological characteristics showed that the classic variant has less chance of developing thyroid capsule invasion (RR=0.77, p=0.0001) and extrathyroid invasion (RR=0.67, p=0.0001); follicular variant presented RR less than 1 in all associations and the combined pattern showed a higher relative risk of 1 in all evaluated parameters (table 3).
Discussion
To date this is the first report on papillary thyroid carcinoma characteristics in Colombia. The distri bution of papillary thyroid carcinoma according to gender and age in our study is similar to that reported in universal literature (5), thus confirming that women of reproductive and middle age are the most affected. Among the men in our series the disease is rare, except among older men (Group C).
The combined pattern is the most frequent histology in both genders and it seems to constitute an aggressive subtype that implies a higher risk of local relapse. This phenomenon allows us to suppose that the carcinogenesis progression in thyroid cells occurs simultaneously in several clones, as some authors have proposed (34). Another hypothesis is that other cell lines could derive from an initial clone.
We believe that the follicular variant is a derivation of the classic variant, which would be the first to appear in the majority of cases, either pure or combined. The follicular variant was more common in women, thus indicating that this behavior could be associated with hormonal factors, as has been reported in the literature (22,23). However, men present more aggressive phenotypes, as seen in the percentage of men with some risk variant or combined pattern which came to 45.58%; this concurs with previous studies on papillary thyroid carcinoma in Japan (11,35).
We did not observe a high frequency of microcarci nomas. This can be explained because Instituto Nacional de Cancerología is a reference center mostly receiving already diagnosed patients for treatment. We seldom diagnose PTC in low risk population (36). In addition, Colombia does not have a widespread access to health services and many cancer patients are diagnosed and treated in later stages.
In our study, the combined pattern and follicular variant were the most frequent variants found in both carcinomas and microcarcinomas. A percentage of 44.1% of microcarcinomas presented a combined pattern that developed metastases, and of these 46.6% developed lymph node metastasis and 26.6 % extranodal metastasis . This allows us to propose that the combined pattern, regardless of tumor size, should be considered as a high risk variant (35,37,38). It should be pointed out that among both the predominant subtypes and the secondary subtypes high risk variants were present.
Out of the total number of microcarcinomas reported, only 25.58% presented multifocality and none presented relapse; these results are not very different from those reported by other authors who conclude that between 7% and 57% of microcarcinomas present multifocality. It has been considered that this feature is a strong factor in relapse occurrence (31-33,37).
The analysis performed among the principal histological variants (classic, follicular and combined pattern) with tumoral histological characteristics revealed that the follicular variant had less probability of developing any type of invasion or metastasis; the opposite was true for the combined pattern, which showed a greater possibility of invasion or metastasis (table 3).
A considerable percentage of patients (83.7%) presented no relapse; this percentage is inferior to that already reported (13). These results are limited due to the fact that this parameter was not evaluated in all cases. Of those patients who suffered relapse, the most common was loco-regional relapse, a fact which coincides with findings described in the literature (13). Nevertheless, metastasis in our study occurred with alarming frequency, which could be associated with various risk factors in our patients, such as the significant frequency of extrathyroidal invasion, large tumoral size and the presence of the combined pattern (table 3).
We reviewed clinical data of patients before PTC diagnosis and we tried to identify links between the combined pattern variant and benign thyroid conditions. Predominant benign or concomitant conditions were Hashimoto´s thyroiditis (33.9%) and goiter (33.1%) We did not find any significant relation between the combined pattern and these benign conditions (data not shown).
In conclusion, we propose including the combined pattern as a high risk variant, and we consider that more studies are needed in order to clarify the biological mechanism of variant development. Our study has limitations, including the relatively short, mean follow-up of our cohort and the retrospective nature of the review. Our results are similar to those previously reported in many aspects. The large size of the lesions and the high percentage of invasion maybe indicate that our patients were treated at later stages. It is probably different in other health institutions of the country where the microcarcinomas and small lesions are more frequent. These findings are important in order to establish health politicies in Colombia.
We thank Andrés González-Rangel, Larry Niño, Franklin Prieto and Felipe Fierro for their support in the design and revision of the manuscript.
The authors declare no conflicts of interest in this investigation.
This study was conducted in the framework of the project Presence of the BRAF V600E mutation in papillary thyroid carcinomas from patients at the NCI, and description of the clinical and histopathologic features," approved and funded by the Instituto Nacional de Cancerología.
Corresponding author: Karime Osorio-Arango, Subdirección Nacional de Trasplantes y Bancos de Sangre, Dirección de Redes en Salud Pública, Instituto Nacional de Salud, Avenida calle 26 N° 51-20, Bogotá, D.C., Colombia Telephone: (571) 220 7700, extension 1567 lkarime15@gmail.com
1. Al-Brahim N, Asa SL. Papillary thyroid carcinoma: An overview. Arch Pathol Lab Med. 2006:130;1057-62. [ Links ]
2. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-917. http://dx.doi.org/10.1002/ijc.25516 [ Links ]
3. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al . Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2014:136:E359-86. http://dx.doi.org/10.1002/ijc.29210 [ Links ]
4. Aschebrook-Kilfoy B, Ward MH, Sabra MM, Devesa SS. Thyroid cancer incidence patterns in the United States by histologic type, 1992-2006. Thyroid. 2011;21:125-34. http://dx.doi.org/10.1089/thy.2010.0021 [ Links ]
5. Cameselle J, Sobrinho-Simoes M. Carcinoma papilar de la glándula tiroides. Problemas en el diagnóstico y controversias. Revista Española de Patología. 2003;36: 373-82. [ Links ]
6. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013:965212. http://dx.doi.org/10.1155/2013/965212 [ Links ]
7. Basolo F, Torregrossa L, Giannini R, Miccoli M, Lupi C, Sensi E, et al . Correlation between the BRAF V600E mutation and tumor invasiveness in papillary thyroid carcinomas smaller than 20 millimeters: Analysis of 1060 cases. J Clin Endocrinol Metab. 2010;95:4197-205. http://dx.doi.org/10.1210/jc.2010-0337 [ Links ]
8. Ahn H, Kim H, Welch H. Korea´s thyroid-cancer epidemic"- -screening and overdiagnosis. N Engl J Med. 2014;671: 1765-7. http://dx.doi.org/10.1056/NEJMp1409841 [ Links ]
9. World Health Organization Classification of Tumors. Pathology and genetics of tumours of endocrine organs. Lyon: International Agency for Research on Cancer (IARC); 2004. p. 49-134. [ Links ]
10. Cano-Valdez A. Aspectos histológicos del cáncer diferen-ciado de la tiroides. Revista Colombiana de Cancerología. 2004;4:73-84. [ Links ]
11. Kakudo K, Tang W, Ito Y, Mori I, Nakamura Y, Miyauchi A. Papillary carcinoma of the thyroid in Japan: Subclassification of common type and identification of low risk group. J Clin Pathol. 2004;57:1041-6. http://dx.doi.org/10.1136/jcp.2004.017889 [ Links ]
12. Lang BH, Lo CY, Chan WF, Lam KY, Wan KY. Staging systems for papillary thyroid carcinoma: A review and comparison. Ann Surg. 2007;245:366-78. http://dx.doi. org/10.1097/01.sla.0000250445.92336.2a [ Links ]
13. Lopes JP, Fonseca E. BRAF gene mutation in the natural history of papillary thyroid carcinoma: Diagnostic and prognostic implications. Acta Med Port. 2011;24:855-68. [ Links ]
14. Santarpia L, Myers JN, Sherman SI, Trimarchi F, Clayman GL, El-Naggar AK. Genetic alterations in the RAS/RAF/mitogen-activated protein kinase and phosphatidylinositol 3-kinase/Akt signaling pathways in the follicular variant of papillary thyroid carcinoma. Cancer. 2010;116:2974-83. http://dx.doi.org/10.1002/cncr.25061 [ Links ]
15. Ghossein R, Asa S, Barnes L, Chan J, Harrison L, Heffess C, et al . Protocols for the examination of specimens from patients with carcinomas of the thyroid gland. Washington, D.C: College of American Pathologists; 2012. p. 2-27. [ Links ]
16. Correa P. The Cali cancer registry, an example for Latin America. Colomb Med. 2012;43:244-5. [ Links ]
17. Chala A, Franco H, Aguilar C, Cardona J. Estudio descriptivo de doce años de cáncer de tiroides, Manizales, Colombia. Revista Colombiana de Cirugía. 2010;25:276-89. [ Links ]
18. Bravo LE, Collazos T, Collazos P, García LS, Correa P. Trends of cancer incidence and mortality in Cali, Colombia. 50 years experience. Colomb Med. 2012;43:246-55. [ Links ]
19. Rodríguez A, De Francisco J, Hakim A, Páez G. Cáncer de tiroides: su tratamiento quirúrgico. Revista Colombiana de Cirugía. 1990;5:95-8. [ Links ]
20. Garavito G. Factores pronósticos para la recaída en pacientes con cáncer papilar de tiroides. Revista Colombiana de Cancerología. 2005;9:21-30. [ Links ]
21. Sobin LH, Gospodariwicz M, Wittekind C. TNM classification of malignant tumors. New York: UICC International Union against Cancer; 2009. [ Links ]
22. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al . Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167- 214. http://dx.doi.org/10.1089/thy.2009.0110 [ Links ]
23. Emad R, Maha A, Kfoury HK, Al-Sheikh AM, Zaidi SN. Three cases of macrofollicular variant of papillary thyroid carcinoma. Ann Saudi Med. 2011;31:644-7. http://dx.doi.org/10.4103/0256-4947.87104 [ Links ]
24. Kondo T, Ezzat S, Asa SL. Pathogenetic mechanisms in thyroid follicular-cell neoplasia. Nat Rev Cancer. 2006;6: 292-306. [ Links ]
25. Lloyd R V., Buehler D, Khanafshar E. Papillary thyroid carcinoma variants. Head Neck Pathol. 2011;5:51-6. http://dx.doi.org/10.1007/s12105-010-0236-9 [ Links ]
26. Mishra A, Jayalakshmi V, Pankaj U, Chikhale N, Patel R, Cherian S. Oncocytic variant of papillary thyroid carcinoma and associated lymphocytic thyroiditis: A case report with review of literature. Int J Head Neck Surg. 2013;4:89-91. http://dx.doi.org/10.5005/JP-journals-10001-1147 [ Links ]
27. Wu Z, Chu X, Fan S, Meng X, Xu C. Papillary thyroid carcinoma with fibromatosis-like stroma: A case report and review of the literature. Oncol Lett. 2013;5:215-7. http://dx.doi.org/10.3892/ol.2012.993 [ Links ]
28. Lawrence CA, Russell ME, Davis RP, Johnson RF Jr, Gorten RJ. The effect of capsule content variations on thyroid uptake results. J Nucl Med. 1970;11:561-3. [ Links ]
29. Mete O, Rotstein L, Asa SL. Controversies in thyroid pathology: Thyroid capsule invasion and extrathyroidal extension. Ann Surg Oncol. 2010;17:386-91. http://dx.doi.org/10.1245/s10434-009-0832-7 [ Links ]
30. Tan YH, Du GN, Xiao YG, Guo SQ, Wu T, Chen PZ, et al . The false thyroid capsule: New findings. J Laryngol Otol. 2013;127:897-901. http://dx.doi.org/10.1017/S0022215113001667 [ Links ]
31. Cadena E, Romero A, Moreno A. Microcarcinoma papilar de tiroides (MCPT) metastásico a hueso. Reporte de caso. Revista Colombiana de Cancerología. 2011;15:98-103. [ Links ]
32. Asioli S, Odasso C, Macrì L, Palestini N, Bussolati G. Merits of the PMiT (papillary microtumor) terminology in the definition of a subset of incidental papillary microcarcinomas of the thyroid. Int J Surg Pathol. 2009;17:378-83. http://dx.doi.org/10.1177/1066896908321181 [ Links ]
33. Rosai J, LiVolsi V, Sobrinho-Simoes M, Williams E. Renaming papillary microcarcinoma of the thyroid gland: The Porto proposal. Int J Surg Pathol. 2003;11:249-51. http://dx.doi.org/10.1177/106689690301100401 [ Links ]
34. Romero A, Meza I. Carcinoma papilar de tiroides, variante esclerosante difusa: un subtipo histológico de difícil diag- nóstico. Revista Colombiana de Cancerología. 2004;4:240-4. [ Links ]
35. Mazzaferri EL, Kloos RT. Clinical review 128: Current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001;86:1447-63. [ Links ]
36. Romero A, Melo M. Implementación del Sistema Bethesda para el informe de citología aspirativa de tiroides con seguimiento histopatológico: experiencia en un centro de tratamiento de cáncer. Revista Colombiana de Cancerologí a. 2014;18:3-7. [ Links ]
37. Hay ID, Hutchinson ME, González-Losada T, McIver B, Reinalda ME, Grant CS, et al . Papillary thyroid microcarcinoma: A study of 900 cases observed in a 60-year period. Surgery. 2008;144:980-7. http://dx.doi.org/10.1016/j [ Links ]
38. Zafon C, Baena JA, Castellvi J, Obiols G, Monroy G, Mesa J. Differences in the form of presentation between papillary microcarcinomas and papillary carcinomas of larger size. J Thyroid Res. 2010;2011:639156. http://dx.doi.org/10.4061/2011/639156 [ Links ]













