Small cell cancer may be associated with a number of paraneoplastic syndromes, including the syndrome of inappropriate antidiuretic hormone (SIADH) 1.To our knowledge, only two cases of small cell cancer associated with Fanconi syndrome have been previously reported 2,3. Small cell cancer associated with isolated phosphate wasting without Fanconi syndrome has also been rarely reported, leading some to consider whether fibroblast growth factor 23 (FGF23) played a role in those cases. Despite this speculation, FGF23 level was not measured in these patients.
We present a case of small cell cancer of the lung associated with three discreet paraneoplastic syndromes, including syndrome of inappropriate antidiuresis (SIAD), Fanconi syndrome, and tumorinduced osteomalacia arising from an inappropriate increase in FGF23. This is the third reported case of SCC associated with generalized renal proximal tubule dysfunction (Fanconi syndrome) and the first report of small cell cancer associated with an inappropriately elevated FGF23 hormone level.
Case presentation
A 57-year-old woman with a 35-year smoking history presented with a cough productive of clear sputum, nausea, and decreased oral intake ongoing for one month. Her past medical history included hypertension, hyperlipidemia, chronic obstructive pulmonary disease, obesity, obstructive sleep apnea, and chronic hepatitis B infection. Her family history included leukemia (father), cancer of unknown primary (mother), thyroid cancer (sister), and bladder cancer (brother).
Investigations
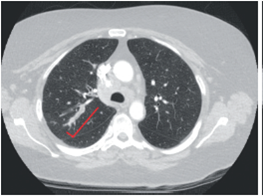
As shown in figure 1, computed tomography of the chest revealed a 3 x 1 cm mass in the posterior bronchus of the right upper lung and rightsided paratracheal and supraclavicular adenopathies. Lymph node biopsy demonstrated a nonhematopoietic malignant neoplasm with strong expression of CD56, consistent with small cell neuroendocrine carcinoma.
Figure 1. Computed tomography of the chest showing the mass in the right upper lung
Initial laboratory studies revealed multiple electrolyte abnormalities at presentation, including hyponatremia, hypobicarbonatemia, and hypophosphatemia.
Although initially attributed to her anorexia and hypovolemic state, the patient's hypoosmolar hyponatremia (Osm 266 mosmol/kg, Na 123 (135-145 mmol/L) was found to persist despite restoration of euvolemia after several days in the hospital. In the setting of euvolemia and normotension, normal renal clearance (eGFR>60 ml/minute/1.73 m2), normal thyroid and adrenal studies, adequate solute intake, and absence of renal sodium wasting (fractional excretion of sodium 0.005), the hyponatremic state continued (Na 122 mEq/L) along with increased urine osmolality (Uosm 545 mOsm/kg). This confirmed the presence of SIAD, likely related to the patient's SCC.
A non-anion gap metabolic acidosis (arterial pH: 7.374, pCO2: 30.5, serum HCO3-: 16 (22-29 mmol/L)) was also identified. A high urine anion gap (46) was measured, consistent with a renal tubular acidosis. Glucosuria (1.0 mg/dl) in the setting of normal serum glucose (86 [70-100 mg/dl]), generalized aminoaciduria, and hyperphosphaturia in the setting of hypophosphatemia were also observed. These findings were consistent with generalized dysfunction of the renal proximal tubule (i.e., Fanconi syndrome).
In the setting of severe hypophosphatemia and normal estimated glomerular filtration rate (eGFR), FGF23 would be expected to be low. However, an elevation of FGF23 was discovered: 500 RU/ml (reference value: <180 RU/ml). Other phosphaturic hormones were normal, including parathyroid hormone (47 pg/ml; reference: 15-65 pg/ml) and parathyroid hormone-related peptide (<0.2 pmol/L). As expected with an increased level of FGF23, 1,25-dihydroxyvitamin D (1,25(OH)2D) was low (8 pg/ml; reference: 18-78 pg/ml), despite a normal concentration (28 ng/ml; reference: 25-80 ng/ml) of 25-hydroxyvitamin D (25(OH)D) and normal eGFR (>60 ml/minute/1.73 m2). In this setting, the elevation of FGF23 was inappropriate and consistent with the presence of an independent paraneoplastic process related to SCC.
Treatment
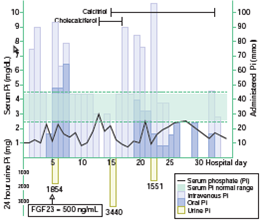
As shown in figure 2, the patient received multiple doses of both oral and intravenous phosphate with minimal overall effect on serum phosphate concentration. The patient's SCC was treated with carboplatin and etoposide.
Figure 2. Graph showing the serum and urine phosphate levels with IV and oral phosphate replacements
Outcome and follow-up
Unfortunately, the patient's multiple electrolyte abnormalities did not improve after initial tumor directed therapy. Follow-up imaging revealed a rapid progression of tumor burden. Subsequently, the patient made the decision to enter hospice care, and she expired.
Discussion
This is the third report of small cell cancer associated with Fanconi syndrome 1,2. One of the two previously reported cases also involved concurrent SIAD.
FGF23 is a hormone produced in osteocytes and osteoblasts that regulates phosphate and vitamin D metabolism. It acts in the proximal tubule by down regulating the expression of luminal sodiumdependent phosphate transporters leading to phosphaturia, and by down-regulating 1a-hydroxylase reducing vitamin D synthesis. It is synthesized as a pro-protein that is cleaved and glycosylated to produce FGF23 fragments 4.
FGF23 is measured by immunometric enzymelinked immunosorbent assay (ELISA). Commercially there are two formats available: The "intact" assay (iFGF23), that recognizes distant epitopes at the cleavage site, and the 'C-terminal' assay (cFGF23), which recognizes two distinct epitopes, in the terminal portion of molecule allowing the measurement of the FGF23 fragments 4,5.
Circulating FGF23 levels are governed chiefly by changes in serum phosphate and by the vitamin D endocrine system. In states of relative hyperphosphatemia or increased production of 1,25(OH)2D, FGF23 concentration rises, promoting renal phosphate wasting and inhibition of 1a-hydroxylase with subsequent attenuation of serum phosphate and 1,25(OH)2D levels. In the condition of tumor-induced osteomalacia, unregulated phosphatonin (e.g., FGF23) production leads to hyperphosphaturia, low circulating levels of 1,25(OH)2D, severe hypophosphatemia, and, eventually, osteomalacia. In this case, neither osteomalacia nor symptoms of osteomalacia were noted. Most documented cases of tumor-induced osteomalacia have involved benign mesenchymal tumors, specifically solitary, non-aggressive appearing soft tissue or osseous lesions 6. However, there are cases in which infiltrating aggressive tumors are seen 7.In a recent review of patients with small cell cancer with apparent tumorrelated disturbances of phosphate metabolism, six patients demonstrated isolated renal phosphate wasting without Fanconi syndrome and two demonstrated oncogenic osteomalacia 3. Of those cases, three had concurrent SIADH, one had concurrent Cushing's syndrome, and one had both concurrent SIADH and Cushing's syndrome. In none of those cases was FGF23 measured. In this patient, hypophosphatemia was promoted by two independent processes: Generalized proximal tubular dysfunction and an inappropriately elevated FGF23.
Conclusions
Small cell cancer may be associated with a variety of paraneoplastic syndromes, including rarely encountered processes such as Fanconi syndrome and tumor-induced osteomalacia. Restoration of serum phosphate to normal levels in individuals with small cell cancer-associated Fanconi syndrome or tumor-induced osteomalacia may prove difficult despite aggressive oral and intravenous phosphate replacement. FGF23 should be measured in any patient with difficulties to manage hypophosphatemia and hyperphosphaturia.