The most common defects found in newborns in South America are cardiac alterations (28 per 10,000 live births), defects of the neural tube closure (24 per 10,000 live births), Down syndrome (16 per 10,000 live births), cleft lip and cleft palate (15 per 10,000 live births), and defects of the abdominal wall (4 per 10,000 live births) 1. Some congenital defects, such as microcephaly, are reported less frequently due to their low prevalence. Given the introduction of Zika virus (ZV), however, microcephaly has gained clinical relevance.
Microcephaly is an important neurological manifestation that may result from insults to early brain development. It is part of the hundreds of genetic syndromes 2 and it has been variably defined in the literature. The World Health Organization (WHO) defines microcephaly as a head circumference less than two standards below the median for age and sex, and severe microcephaly as a head circumference less than three standard deviations below the median for age and sex 3.
One study reported that approximately 61% of children with a head circumference less than two standard deviations have no abnormal findings on evaluation with imaging techniques 4. When imaging techniques reveal brain malformations, the following findings have been documented: Ventricular dilatation, mild atrophy (31%), moderate to severe atrophy with ventricular dilation (28%), and isolated parenchymal abnormalities (2%) 4. Other studies using magnetic resonance imaging (MRI) have reported the presence of brain abnormalities in 67-80% patients with microcephaly 5,6. MRI is the most sensitive diagnostic tool for the evaluation of microcephaly.
Microcephaly may be congenital or postnatal 7, which means a failure in brain growth after birth. It is also described as syndromic or primary (known as vera microcephaly). This classification depends on the presence or absence of extra-cranial malformations or facial dimorphism 2. Microcephaly is sometimes the first sign of a congenital condition, a genetic anomaly or an acquired problem (due to congenital infection) 8. Genetic causes have been reported in approximately 15.5% to 53.3% of cases.
The prevalence of metabolic disorders is unknown, but it is estimated to be 1% to 5%. The conditions associated with microcephaly include epilepsy (40%), cerebral palsy (20%), intellectual disability (50%) and eye problems (20-50%) 2. A diagnosis of microcephaly has serious clinical implications, as there is a direct correlation between the degree of microcephaly and the degree of intellectual disability 9.
Since the end of 2015, microcephaly has received global attention due to the ZV epidemic in the Americas. Different criteria for causality have been established, including a spatial-temporal relationship and biological plausibility that entails identification of ZV in the brain tissue of affected fetuses 10. Animal models have been developed to try to provide a pathophysiological explanation for microcephaly via congenital infection with the virus 11. In February 2016, the first case of intrauterine transmission of ZV was reported, which featured neurological malformations in the fetus 12. In the months following the emergence of ZV in Brazil, an annual increase of up to 20 times the number of cases of birth defects has been reported, with a marked increase in microcephaly in particular 13. In 2015, 1,248 new suspected cases of microcephaly were reported in Brazil, with a prevalence of 99.7 per 100,000 live births. With these observations, the Brazilian Ministry of Health confirmed the relationship between ZV and microcephaly 14. Subsequently, WHO declared an epidemiological alert regarding ZV and its association with congenital malformations and neurological syndromes 15. Thus, ZV and its association with birth defects have recently become a public health problem of international importance 16.
So far, associative epidemiological links exist between ZV and microcephaly. This has resulted from the increase in the number of newborn infants with microcephaly 13,17 in countries where there is a high rate of suspected and confirmed cases of infection by ZV 18. Some hypotheses suggest that the teratogenic mechanisms of ZV are associated with the precipitation and deregulation of retinoic acid-dependent genes, extending the sequences in the genome that are closely involved with the development of the brain. This mechanism is known to be associated with other neurotropic viruses. For this reason, the spectrum of malformations generated by hypervitaminosis A presents with an embryopathy that appears similar to that of ZV 19,20. Other researchers suggest a direct immune effect of the virus on neuronal cells as demonstrated in animal models where the high replication rate of ZV in progenitors of neuronal cells, which have a high concentration of viral receptors, is suggested to be the gateway to the entrance of the virus to the brain. Immunoreactivity with markers associated with cell death, such as caspases, leads to apoptosis of these cells and pyramidal corticospinal neurons, which ultimately generate the appearance of microcephaly as an external feature 21.
In Colombia, there were 657,126 reported cases of infection by ZV from April to June, 2016. Four percent of these cases were confirmed by PCR. The infection rate was two times higher in women than in men. Within this infected population, 11,944 pregnant women were reported, with 12% of these ZV cases confirmed by PCR; 90% of pregnant women who reported this infection gave birth to children with no apparent abnormalities. Fifty newborns were reported with possible microcephaly; 26 of these cases are still being investigated, while 20 have confirmed congenital defects that caused genetic and neural tube defects. Of these patients, four have evidence of congenital ZV infection that presents with microcephaly and without coinfections 22. It is important to understand the prevalence of microcephaly in Colombia in the years prior to the ZV epidemic in order to have a starting point to establish comparisons after its arrival to Colombia and assess its possible involvement in birth defects of the central nervous system, such as microcephaly.
In order to assess the prevalence of microcephaly in Colombia prior to the ZV epidemic, we conducted a systematic review of the literature. Articles included for consideration in the present study were those that addressed Colombian patients with microcephaly, as reported between 1982 and 2013. The primary outcome studied was the prevalence of microcephaly in Colombia during this period. The secondary outcome was the prevalence of birth defects of the central nervous system in Colombia during the period.
Materials and methods
The protocol for the systematic review was registered in the United Kingdom National Institute of Health and Research International Prospective Register of Systematic Reviews (PROSPERO) as number 48859.
The objective of the systematic review was to determine the prevalence of birth defects in Colombia from 1982 to 2013. Articles published in Spanish, English, and Portuguese were included. The inclusion criterium was cross-observational studies that determined the prevalence of birth defects in Colombia, including microcephaly as defined by the Latin American Collaborative Study of Congenital Malformations (ECLAMC). We excluded articles in which the diagnosis was done during the prenatal period, due to the absence of confirmation of microcephaly in these studies. The outcomes measured were the prevalence of microcephaly and the prevalence of central nervous system birth defects in Colombia between 1982 and 2013.
The search of the literature was performed in the different international, Latin American and national (Medline, Scopus, Science Direct, Lilacs, Dare, Bireme, and Cochrane) databases. The following Medical Subject Headings (MeSH) search terms were used: “birth defects,” “microcephaly,” “prevalence,” and “Colombia.” Additional Latin American and national data were obtained from the annual reports of the epidemiological surveillance of congenital malformations for articles published before April, 2015; the last search was performed in October, 2016. We searched for additional literature in the references reported in indexed articles. Moreover, some authors were contacted for additional sources of information. The eligible study designs included cross-sectional observational studies, cohort, case-control, ecological, and reports of the epidemiological surveillance of congenital malformations.
Articles and abstracts were examined independently by two reviewers in order to select those to be considered for complete text review based on the inclusion and exclusion criteria and, in case of disagreement, a third reviewer assessed the article and the decision was made by consensus. The data collected from each study were the number of cases of microcephaly, the period of time studied, the number of births and the number of defects of the central nervous system.
The limitations of the study include the fact that the definition of microcephaly varies in the literature.
The definition used for data collection in this study, as well as in the majority of the reviewed articles, was head circumference less than three standard deviations of the mean for age and sex. To control this selection bias, we included studies performed in institutions using the ECLAMC criteria, since the institutions using this surveillance system feature a greater sensitivity, uniformity, and coverage of defects compared to those monitored by the surveillance system (Sistema de Vigilancia en Salud Pública, Sivigila) of the Instituto Nacional de Salud23. In addition, another possible risk of bias was the failure to include a study in which microcephaly was evaluated. Therefore, we designed a system for searching those articles in which databases were searched and, subsequently, references in the articles found in order to minimize the loss of data.
Data analysis
We collected the data from eligible studies considering the study design, year of publication, authors, area, and period of the study. The following information was extracted from each article: The total number of malformations, the number of cases of microcephaly reported, the number of nervous system malformations, and the number of births in the period studied. These data were then combined and used to calculate the rates per 10,000 live births. In order to avoid repeating data, if the participants were included in more than one study, only the study with the greater sample size was included.
Results
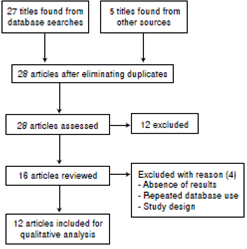
Using the MeSH terms defined in the methodology, 32 articles were identified in the different databases, references and monitoring systems of national birth defects. Initially, the repeated articles were excluded, and after filtering the articles and applying the inclusion and exclusion criteria, 28 articles were eligible, of which 12 were included in the review since they accomplished the primary and secondary objectives of the research (figure 1).
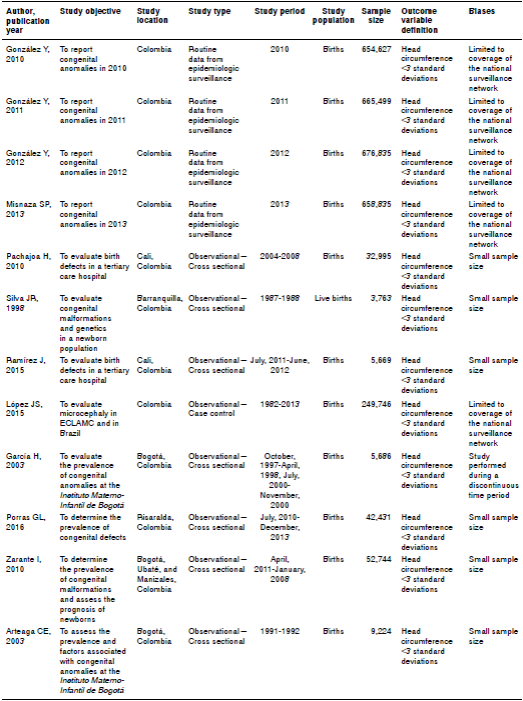
The studies reviewed were published between 2003 and 2015 in Brazil and Colombia, all using data from Colombia. The period evaluated included 2,808,308 births, 21,363 malformations, 1,680 neurological malformations and 420 cases of microcephaly (table 1).
Table 1 Prevalence of microcephaly and central nervous system anomalies per 10,000 births in Colombia
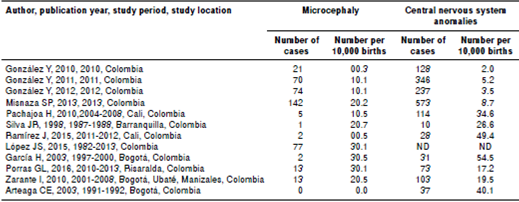
During the period evaluated, the surveillance system (Sivigila) of the Instituto Nacional de Salud was started started. In 2009, a pilot test was developed and an annual report for the 2010 period was published. During the period 2010-2013, there were 2,655,796 births, of which 0.35% had defects of some kind, including 1,248 reported malformations of the central and peripheral nervous system, which corresponded to an average of 15.8% of all congenital malformations reported, with a prevalence of 4.85 per 10,000. Of these, 3.38% corresponded to microcephaly, with an average prevalence of 1.17 cases per 10,000 births (table 2).
The prevalence of birth defects in the country varied between 8.7 and 68.9 per 10,000 live births from 2010 to 2013 according to Sivigila, an increase directly related with the coverage of this program nationwide. The highest reported rate of birth defects came from Bogotá, reaching 430.8 per 10,000 births. The lowest rate came from the department of Risaralda, reported as 89.8 per 10,000 births. The highest prevalence of microcephaly reported was from Bogotá, reaching 3.5 per 10,000 births in 2003. In the period of study, the rate of central nervous system defects in Colombia ranged from 2 to 8.7, with microcephaly ranging from 0.3 to 3.1 per 10,000 births. On average, the prevalence of these defects and microcephaly was 23.5 (95% CI 23.1-24) and 1.8 (95% CI 1.7-1.8) per 10,000 births, respectively. The study that reported the highest prevalence for microcephaly in the country was by ECLAMC during the period 1982-2013. In this study, 24,976 births were reported, of which 77 were registered with microcephaly, leading to a prevalence of 3.08 per 10,000 births for the follow-up period (table 2).
Discussion
Congenital defects are a worldwide public health problem. It is estimated that 7.9 million children are born with congenital defects every year, with 3.3 million children under 5 years of age dying due to these defects and 3.2 million surviving with disabilities 24. As a cause of infant death in Colombia in recent decades, congenital anomalies ranked seventh in 1970, fourth in 1980 and third in 1994 25. From 2000 to 2004, a total of 14,036 deaths from congenital anomalies was reported in Colombia, with a mortality rate of 8.43 per 10,000 births 26. From 2005 to 2011, congenital defects were reported as the second leading cause of death in children under one year of age, contributing to 20.8% of all deaths, according to the Departamento Administrativo Nacional de Estadísticas (DANE) 27. According to the analysis of the health situation in Colombia, congenital defects are the second leading cause of infant mortality. The available evidence suggests that the prevalence and the potential burden of congenital disorders in public health are high in developing countries and, in some circumstances, they are greater than in developed countries. Birth defects in Colombia are responsible for 23% of the total mortality in children under 5 years of age 28, a clinically significant issue that has been declared a public health problem 29.
After the ZV outbreak in the Americas, birth defects such as microcephaly have gained particular clinical relevance. Before the epidemic, the definition of microcephaly was heterogeneous, controversial, and varied between institutions 30. Some authors classify microcephaly as a head circumference less than two standard deviations from median values 31. Other authors suggest that this measure should be necessarily adjusted to prematurity and to the length of patients’ head circumference 9,32. Assuming that the cephalic perimeter has a normal distribution across the population, 2.3% of all children would be defined as having microcephaly. Despite this, literature estimates that less than 0.54% to 0.56% of children are classified with a head circumference less than two standard deviations, which suggests a non-normal distribution of this measure 9. The true number of cases of microcephaly in Brazil, where the ZV epidemic was first associated with the condition, was unknown since this event was overestimated, no active search was done, and its diagnosis was based on non-standardized criteria before the associations between Zika and congenital defects 30.
We conducted a systematic review of the literature regarding the frequency of microcephaly in Colombia. The objective was to determine the prevalence of microcephaly in the country before the ZV epidemic and to establish whether there was a change in the prevalence of microcephaly per 10,000 births. Such information would allow us to determine if the increase of microcephaly cases was significant and develop a better approach to the Zika virus epidemic in Colombia and its association with congenital defects.
During the study period, microcephaly was equivalent to 3.38% of congenital defects and its prevalence rate fluctuated between 0.3 to 3.1 per 10,000 live births, with an average rate of 1, 56 per 10,000 live births from 1982 to 2013. Compared with the rate of microcephaly in the rest of Latin American countries, Colombia’s rate falls within the average since ECLAMC rate per 10, 000 live births was 4.53 (95% CI 4.05-5.02) in Brazil and 4.30 (95% CI 2.57-3.22) in Chile, compared with 3.08 per 10,000 live births (95% CI 2.04-3.84), which does not surpass the global rate of microcephaly according to ECLAMC, which was 3.30 (95% CI 3.09-3.50) per 10,000 live births between 1982 and 2013. According to ECLAMC, from 1982 to 2013, Brazil and Chile had the highest prevalence of microcephaly in Latin America 33.
In the study period, few Colombian departments and cities had surveillance systems for reporting birth defects such as microcephaly. Among the studies found in literature, microcephaly, defined as a head circumference less than three standard deviations when adjusted for age and sex, we found those from Cali, Barranquilla, Bogotá, Risaralda, Manizales, and Ubaté. Besides these studies, microcephaly had also been reported in articles assessing birth defects across Colombia.
This relatively small amount of reporting on microcephaly could be explained by the low frequency of the event, which leads to its exclusion in the final statistics. Nevertheless, the number of reports of congenital malformations has increased in recent years, as noted in the annual report of Sivigila, which may be explained by an increase in reporting or an increase in the rate of microcephaly. We were unable to make this distinction in the present study, which represents a limitation.
Compared to the prevalence of microcephaly reported by ECLAMC from 1982 to 2013, the prevalence reported by Sivigila from 2010 to 2013 was lower, with an average prevalence of 1.5 births with microcephaly per 10,000 births. The studies reported and included in this review only classified the defects and described the frequency of microcephaly, but did not discriminate according to etiology. In the present review, we could not find any observational cohort studies or case-control studies evaluating the risks and other measures of association of microcephaly in Colombia. However, the different cross-sectional studies reported in the country confirmed the existence of microcephaly before the emergence of autochthonous ZV in the country.
One limitation of this study was the variability of the diagnostic criteria of microcephaly. We used the more rigorous criteria, that of less than three standard deviations of head circumference, adjusted for age and sex. Consequently, studies using other criteria for microcephaly were not included. Additionally, it is possible that not all relevant studies were found and included in the review, although we adopted measures to reduce the likelihood of this limitation.
Finally, the prevalence of microcephaly in Colombia from 1982 to 2013, before the introduction of ZV, ranged from 0.3 to 3.1 per 10,000 births, with an average of 1.8 (95% CI 1.7 - 1.8) per 10,000 births.
These findings are important to determine if the prevalence after the introduction of the Zika virus has meant significant changes.