Cervical cancer persists as a relevant cause of cancer mortality among women from developing countries where 83.1% of cases and 85.5% of deaths occur 1. From 2007 to 2011, 4,462 cases and 1,861 deaths due to this cancer per year were estimated in Colombia and it remains a leading cause of cancer mortality among women 2.
Cervical cytology has been the main strategy for cervical cancer early detection. After the introduction of massive screening, a reduction of invasive cervical cancer incidence and mortality was observed in most developed countries 3; conversely, conventional cytology has not reduced cervical cancer mortality in the majority of developing nations. Cytology is a highly specific technique, however, it is only moderately sensitive (about 50%) 4; therefore, cytology-based screening programs require frequent examinations and multiple visits to healthcare centers in order to complete the entire process for screening, diagnosis, and treatment of cervical intraepithelial neoplasia (CIN). The above mentioned factors, combined with limited access to healthcare services, have been cited as the main restraints on successful cervical cancer screening in low- and middle-income countries 5.
Alternative approaches have been evaluated as a means of improving screening performance. HPV tests have demonstrated high sensitivity (about 90%) but no impact on the number of visits for follow-up of screened women with positive results 4,5. Recently, a new generation of HPV tests has been developed to provide rapid results allowing for the possibility of conducting immediate treatment of preneoplastic lesions 6; however, strategies for immediate triage to select women for treatment during the same visit are still under elucidation.
Direct visual inspection with acetic acid (VIA) or Lugol’s iodine (VILI) has been evaluated in several studies in developing countries 7. The main advantage of VIA and VILI is the immediate report that allows for treatment of preneoplastic lesions during the same visit thereby reducing the difficulties for follow-up of screened women with positive results. VIA and VILI have been compared with conventional cytology and HPV tests showing higher sensitivity than the former but lower than the latter 4,7. Moreover, the evaluation of VIA with magnification lenses (VIAM) has revealed no improvement in sensitivity or specificity compared with naked- eye visual inspection8.
On the other hand, colposcopy provides a potent magnified visual evaluation of the cervix with the help of acetic acid and Lugol’s iodine.The use of colposcopy for the diagnosis of cervical lesions and the orientation of cervical biopsies is widely accepted and studies of diagnostic accuracy in this field generally apply colposcopy (and oriented biopsy) as the reference standard. However, colposcopy as a screening test has reported only moderate proficiency 8;9.
The aim of our study was to compare the data on colposcopy and direct visual inspection proficiency as screening tools in see-and-treat scenarios for CIN2-3 or cancer detection in a Latin American population.
Materials and methods
A diagnostic accuracy study was conducted with 5,011 women from three low-income districts in Bogotá, Colombia. The protocol was approved by the Ethical Committee at the Instituto Nacional de Cancerología of Colombia.
The detailed methodology has been described elsewhere 10. Women were consecutively recruited at primary care centers. In one visit, each woman underwent consecutive conventional cytology, VIA, VILI, and colposcopy. Both VIA and VILI had the same provider, a nurse, who had taken a one-week training course. Colposcopy was performed by expert gynecologists from the Hospital de San José. Interpreters for conventional cytology, VIA-VILI, and colposcopy were blinded from each other and punch biopsies were obtained independently for any positive VIA, VIA-VILI or colposcopy (Reid index ≥1) results. If cytology reported a high-grade lesion (high-grade squamous intraepithelial lesion, HSIL) or more, and the visual techniques were negative, the patient underwent a second colposcopy.
Positive VIA corresponded to acetowhite growths or definite lesions close to the squamocolumnar junction. Positive VILI corresponded to yellow non- uptake iodine areas close to the squamocolumnar junction. For comparative purposes, we defined two colposcopy thresholds: Low-grade CIN and high- grade CIN diagnoses (Reid index: 0-2 and 3-8, respectively) 10.
Based on the independent collection of histological samples for any positive visual technique, the biopsy was assumed to be the gold standard. Excluding colposcopy from the gold standard induces a verification bias since only screened women with positive results underwent biopsy and, thus, neither sensitivity nor specificity could be directly estimated for comparative purposes. To tackle this problem, we compared detection rates and false positive rates conducting the analysis according to Sullivan (table 1)11.
Table 1 Framework for screening tests analysis
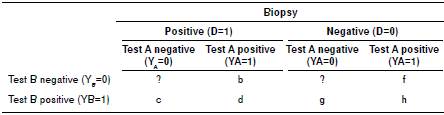
To compare colposcopy with direct visual inspection we did not assume colposcopy as the gold standard; consequently, we solved the verification bias by comparing detection and false positive rates between the two techniques according to Sullivan 11. Detection rates correspond to the product of multiplying test sensitivity by the prevalence of disease and false-positive rates correspond to the proportion of false-positive results multiplied by the complement of disease prevalence
The detection rate (DR) corresponds to the joint probability for the test and the gold standard to be positive (DR = P(Y=1, D=1)), false positives correspond to the joint probability for the test to be positive and the gold standard to be negative (FP = P(D=0,Y=1)), and the disease prevalence corresponds to the probability for the gold standard to be positive (P(D=1)). Therefore, the DR for a given test (A or B) corresponds to the product of multiplying its sensitivity by the prevalence of the disease (DRA = ((b+d)/(c+d+b+?)) * ((c+d+b+?)/N) in table 1), FP for a given test (A or corresponds to its proportion of false positive results multiplied by the complement of the disease prevalence (FPA = ((f+h)/(g+h+f+?))*((g+h+f+?)/N) in table 1). Since our study had a parallel design, the prevalence of the disease was the same for all tests allowing for direct comparison.
Accordingly, we compared colposcopy with VIA and VIA-VILI by determining sensitivity ratios (SR=DRVIA/DRColpo and SR=DRVIA-VILI/DRColpo) and false positive ratios (FPR=FPVIA/FPColpo and FPR=FPVIA-VILI/FPColpo). A comparison of VIA and VIA-VILI had already been reported estimating sensitivity and specificity for both tests when using colposcopy and biopsy as the gold standard 10. The biopsy was considered positive with a report of CIN grade 2 or more.
The variance for sensitivity ratios and false positive ratios was estimated, and the corresponding 95% confidence intervals reported: Var (log SR) = (DRA + DRB - 2SR)/(N DRA* DRB) Var (log FPR) = (FPA + FPB - 2FPR)/(NFPA* FPB), where SR corresponds to the joint probability for both tests and the gold standard to be positive (P (YA = YB =1, D=1)), and FPR corresponds to the joint probability for both tests to be positive and the gold standard to be negative (P(YA=YB=1,D=0)). The analysis was carried out with Stata13.0™.
Results
In total, 54 women were excluded for various reasons 12 and 4,957 underwent screening from whom 602 biopsies were obtained (figure 1). The average age was 39.2 years (range: 25-59). Positivity rates for colposcopy were 1.6% when using the high-grade CIN threshold, and 10.8% for the low-grade CIN threshold. Positivity rates for VIA and VIA-VILI were 7.4% and 9.9%, respectively.
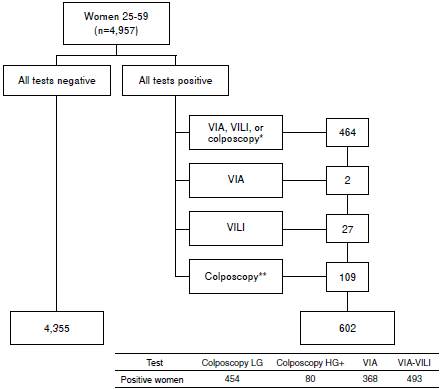
Figure 1 Study flow chart VIA: Visual inspection with acetic acid; VILI: Visual inspection with Lugol iodine; LG: Low grade; HG: High grade * VIAand VILI 45; VIA and colposcopy 4; VILI and colposcopy 103; VIA, VILI, and colposcopy 312; colposcopic evaluation without previous screening report ** Initial colposcopic evaluation negative with a second colposcopic evaluation after low-grade lesion reported on conventional cytology. They were included to integrate the histopathology evaluation in the gold standard without considering them for assessment of colposcopy detection or false positive rates. The figure describes specific test positivity.
VIA revealed a significantly lower detection rate than colposcopy low- grade CIN threshold (SR 0.72, 95%CI: 0.57-0.91) and simultaneously reported a significantly lower false-positive rate (FPR 0.70, 95%CI 0.65-0.76) (table 2). No significant differences between VIA-VILI and colposcopy were observed when using this colposcopy threshold.
Table 2 Detection and false positive rates contrasting VIA, VIA-VILI, and colposcopy
VIA: Visual inspection with acetic acid; VILI: Visual inspection with Lugol iodine; SR: Sensitivity ratio; FPR: False positiveratio
Using the high-grade CIN threshold for colposcopy, both VIA and VIA-VILI showed significantly higher detection and false positive rates (table 2). Detection rate for VIA-VILI was twice the correspondent detection rate for colposcopy and its false positives were eight times higher than those for colposcopy.
Sensitivity rates for VIA and VIA-VILI decreased with age (figure 2). Between ages 25 and 49, VIA-VILI showed higher sensitivity rates than VIA alone when compared to colposcopy but without significant differences. Both tests had significantly higher detection rates than colposcopy between ages 30-39 (SRVIA/Colpo2.4, CI95%: 1.3-4.2; and SRVIA-VILI/Colpo2.8, CI95%: 1.5-5.0). No major changes with age were observed for sensitivity rates when using the low-grade CIN colposcopy threshold.
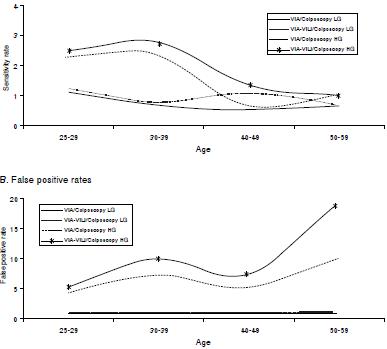
Figure 2 Sensitivity ratios and false positive ratios according to age group VIA: Visual inspection with acetic acid; VILI: Visual inspection with Lugol iodine; LG: Low grade; HG: High grade
The false positive rates for VIA and VIA-VILI increased with age, being particularly high over age 50 (figure 2). For all age groups, the VIA and VIA- VILI probability of false positives was significantly higher than colposcopy. Between ages 30-59, VIA-VILI revealed higher sensitivity rates than VIA alone when compared with colposcopy but without significant differences. For the low-grade colposcopy threshold no major changes with age were observed; nevertheless, VIA had a significantly lower false-positive rate than colposcopy in all age groups.
Discussion
Several studies have evaluated alternatives to conventional cytology attempting to improve the performance of screening programs in developing countries and the accuracy of cervical cancer screening tests is currently a topic of major discussion. In addition, low access to regular healthcare is observed as one of the major restraints for such settings inducing low screening adherence and follow-up of screened women with positive results; accordingly, see-and-treat approaches have been proposed as a promising alternative to reduce cervical cancer mortality in low-income regions 8.
Colposcopy and directed biopsy are considered the gold standard for CIN diagnosis. High specificity is the principal advantage of colposcopy and guidance for the diagnostic biopsy is frequently highlighted as the principal role of colposcopy; moreover, earlier data revealed an 83-84% agreement for CIN2+ diagnosis between colposcopy guided biopsies and loop excision 12.
Although direct visual inspection for cervical cancer screening uses the same technical principles as colposcopy, it is still controversial. The main concerns about VIA and VILI are their low specificity and reliability 7. Indeed, several studies have shown significantly lower specificity for direct visual inspection than for conventional cytology but, simultaneously, they have demonstrated a similar or higher sensitivity (particularly for VILI) 7.
Taking into account the advantages and restraints of visual screening techniques means that careful application is paramount in areas where high cervical cancer risk and low access to healthcare services sustains its greatest suitability, spaced out from areas with proper access to healthcare where women can seek screening, diagnosis, and treatment in several visits 10. Hence, the availability of immediate results allowing for immediate treatment, the low cost, and the implementation feasibility of visual screening in the former scenarios stress the need for an unbiased appraisal.
Our study is one of the first to compare colposcopy, VIA, and VILI in Latin America where many areas lack the necessary infrastructure and resources to maintain an organized screening program based on Pap-smear (several visits). The results show higher detection rates for VIA and VIA-VILI over colposcopy when the high-grade CIN colposcopic diagnosis is used as the positive threshold but the difference disappears if the threshold for colposcopy is changed to low-grade CIN diagnosis; for this latter cutoff point, colposcopy detects more CIN2+ than VIA alone.
These data revealed a lack of correlation between high-grade colposcopic appearance and CIN2+ diagnosis. The use of colposcopy without the guidance of a previous test (screening) has been debatable. Blinded colposcopies have shown lower accuracy than diagnostic colposcopies after a positive screening test 8,13,14. In addition, previous reports have demonstrated that colposcopy sensitivity increases considerably when taking additional biopsies to those guided by the colposcopic appearance of high-grade CIN 15,16. The detection of CIN2+ increases up to 37% when additional biopsies are obtained 15,17 and this increase has been demonstrated to be determined by the number of biopsies, regardless of the provider. The reason for the expanded detection is apparently related to the small size of several CIN2+ lesions because a correlation between false- negative colposcopy and thinner lesions has been observed 14,18-20.
The present study results corroborate the high specificity of colposcopy but this goes together with a lower detection rate suggesting that colposcopy diagnosis (low-grade or high-grade) merits careful review as the basis for orienting biopsies. These findings highlight the limitations ofvisual techniques for screening purposes (with or without magnification), but they also reveal to some extent the need for improving CIN diagnostic methods.
VIA-VILI reproduces the colposcopic procedure (without magnification) and certain studies have shown no gain when adding magnification to direct visual inspection with acetic acid (8). However, colposcopy provides considerably more detailed information on the cervical epithelium leading to more precise CIN diagnoses as demonstrated by its lower false positive rates. Furthermore, a meta-analysis showed a high correlation between direct VIA or VILI (higher for VILI) and colposcopy used as the gold standard7 confirming our results where VIA-VILI had no significant differences with colposcopy low-grade threshold On the other hand, the false positive rates showed an opposite tendency with higher values for VIA and VIA-VILI when compared to colposcopy high-grade CIN threshold but, again, the difference disappeared for the low-grade threshold highlighting the fact that the accuracy of VIA-VILI was equivalent to colposcopy low-grade CIN threshold for both detection and false positive rates.
The analysis according to age groups showed no major changes in sensitivity and false positive rates for colposcopy low-grade CIN threshold. Conversely, for the high-grade CIN threshold, colposcopy proved to be more specifica cross age groups than either VIA or VIA-VILI because there were no differences in detection rates but false positive rates were significantly higher. This latter observation is particularly relevant in postmenopausal women (over age 50) and the variation was greater for VIA alone since the detection rates for ages 40 and over significantly decreased. Previous studies on visual inspection have found lower positive rates in postmenopausal women due to the characteristics of the transformation zone for this age group 7-10; the addition of high false positive rates might suggest a contraindication for direct visual inspection among women over fifty. A higher false positive rate induces higher overtreatment in see-and-treat scenarios; yet, overtreatment with ablative methods do have a low rate of side effects 21.
Additional limitations of visual screening are low reproducibility and lack of experience in everyday settings.The existing information shows extensive world wide variation for direct visual inspection among studies7,which indicates that the training level, the experience in carrying out the tests, and the regular evaluation of providers are key components for these techniques as it would be for colposcopic screening. Furthermore,in Latin America, colposcopy is provided only by trained gynecologists, are sources carcely available in areas with low access to health care; however, nurse colposcopy extends over many developed and developing countries. Additionally, accuracy of colposcopy and visual inspection has been shown to be similar when delivered by nurses or physicians but dependent upon the level of training and expertise22,23.
Despite the aforementioned restraints, a clinical trial revealed a reduction in cervical cancer mortality of around 37% using VIA and immediate treatment (same visit) 21, but this reduction could not be reproduced in a second trial where the treatment was provided during a subsequent visit after colposcopic evaluation thus resulting in a lower treatment rate 24. In a second study, only HPV tests achieved a significant reduction in cervical cancer mortality demonstrating the relevance of highly sensitive tests in which only a few contacts for the target population are expected. Concordantly, economic evaluations for developing countries have reported bettercost-effectiveness ratios for screening and treatment in one visit, as well as a progressive reduction in screening proficiency when the number of visits is incremented 25.
VIA, and particularly VIA-VILI, have proven higher sensitivity than cytology 7. In this sense, our study showed they have similar detection rates than colposcopy using the low-grade diagnosis as the threshold, which opens a window for the use of these techniques as screening methods in the context of see-and-treat approaches aimed at reducing the number of visits. Accordingly, if rapid HPV tests capable of producing immediate results were available, both techniques used as reflex or triage tests for immediate treatment represent the chance for reducing cervical cancer mortality for underserved women where see-and-treat is a more suitable approach than screening programs based on multiple visits.
Although cervical cancer screening studies in developing countries frequently have a verification bias, a proper analysis could lead to accurate comparisons between screening alternatives avoiding underutilization of available data. Visual techniques could help reducing cervical cancer mortality by decreasing the number of visits between screening and treatment. In this context, VIA-VILI and colposcopy with low-grade threshold were equivalent and reported acceptable proficiency for screening purposes.














