Leishmaniasis is a parasitic disease caused by flagellated protozoa of the genus Leishmania which are transmitted by the bite of female phlebotomine sand flies and can give rise to any of the three main clinical forms in the human host: Cutaneous, mucosal or visceral.
According to data from the World Health Organization (WHO), there have been cases reported in 102 countries, with an annual estimate of 0.2 to 0.4 million cases of visceral leishmaniasis, and 0.7 to 1.2 million of cutaneous leishmaniasis 1. With the exception of the islands of San Andrés and Providencia, leishmaniases are diseases endemic to Colombia, with 10,743 confirmed cases in 2016. Of these, 10,561 corresponded to the cutaneous form, 122 to the mucosal form, and 60 to the visceral form 2. As such, Colombia is among the top ten countries with the highest incidence of cutaneous leishmaniasis in the world, where 60 % of the population is at risk of acquiring this clinical form 3.
In Colombia, five studies have been conducted to establish the geographical distribution of Leishmania spp. 4-8. The identification of species was made from parasites isolated from patients, sand flies, and animal hosts. Geographical distribution maps were drawn that indicated the origin of the patient or the infected organism. However, these studies achieved only partial coverage of the different areas of the country and the distribution of circulating species is still largely unknown in many parts of Colombia. Other smaller-scale studies, which reported disease outbreaks through active case finding or the capture of sand flies as well as potential reservoirs, have filled in some gaps regarding the presence of Leishmania spp. in other geographical zones 9-13.
Currently, there is no publication that compiles the reports of species in Colombia; for this reason, this work aimed to search, review, and compile the available scientific literature regarding Leishmania spp. and their geographical distribution in Colombia.
Materials and methods
Search strategy and selection criteria
A bibliographic search was carried out in PubMed, Web of Knowledge, Google Academic, SciELO and LILACS databases in order to collect all available information related to the identification of Leishmania species in Colombia. The search was made with the combination of the boolean terms “(Leishmania OR Leishmaniasis) AND species AND Colombia”, without restrictions on the year of publication, language or infected organism. In addition, the records of national scientific events (among them those of eleven Colombian Congresses of Tropical Medicine from 1987 to 2015) and repositories of theses from Colombian universities were searched.
The identification of parasites to the genus level, the geographical origin of the patient, and the vector or the infected reservoir were used as inclusion criteria.
Extraction and synthesis of information
For this review, all available scientific literature that met the inclusion criteria was taken into account; however, given the large number of documents, only published articles and gray literature with unique reports in the country were included.
Once the search results were compiled, the duplicate articles were identified and eliminated. Subsequently, those in which the title and summary were not related to the topic of interest were excluded. The full text of the articles, abstracts, and theses was reviewed to identify those that met the inclusion criteria.
During the review of each document, the following data were extracted: The geographical origin of the sample, the host (human, vector or reservoir), the clinical form of the disease, the typing method used, and the species or subgenus identified.
Results
There were 86 articles published between 1985 and 2017 in which the species of the Leishmania spp. and the geographical origin of the sample were indicated (Annex 1). Of these, 57 were scientific articles and 29 corresponded to gray literature, of which 26 were abstracts presented at national scientific events and 3 were undergraduate degree theses.
Geographical distribution
Studies of the geographical distribution of Leishmania spp. report, in order of their frequency, the circulation of Leishmania (Viannia) panamensis, L. (V.) braziliensis, L. (V.) guyanensis, L. (Leishmania) infantum, L. (L.) amazonensis, L. (L.) mexicana, L. (V.) colombiensis, L. (V.) lainsoni, and L. (V.) equatorensis; the last three with equal frequency 4-8.
According to the studies by Corredor, et al. 4, Ovalle, et al. 5, and Ramírez, et al. 6, in which the distribution of species by department is described, L. (V.) panamensis, L. (V.) braziliensis, L. (L.) mexicana and L. (L.) infantum are, in order, the species with the greatest geographical distribution and are present in 22, 19, 12 and 8 departments of the country, respectively. These studies provide an approximation of the distribution of Leishmania spp. in Colombia; however, they do not represent the entire country.
It is worth noting that some species grow better in cultures than others. Given this fact, when comparing L. (V.) panamensis and L. (V.) braziliensis frequencies, caution must be exercised in claiming that one species’ geographical distribution is greater or lesser than that of other species.
To determine the distribution of Leishmania spp. by department, we compiled information of the identified species and the geographical origin of the organism based on the 86 works that were found in the bibliographical review. Information on geographical origin was variable; some studies included detailed information, including the municipality, the county (vereda) or both, and others included less detailed information, such as department, natural region or river basins. The geographical scale depended primarily on the study coverage; studies of cases and outbreaks of leishmaniasis provided the most detailed information.
We also describe the geographical distribution of the Leishmania species reported in Colombia 4-42. However, given the small number of studies with detailed information on geographical origin, we decided to characterize the distribution by department (table 1 and figure 1).
Table 1 Leishmania species reported in Colombia for each department
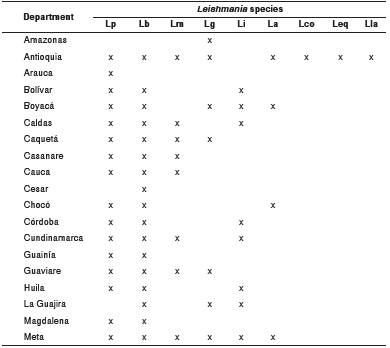
Lp: L. (V.) panamensis; Lb: L. (V.) braziliensis; Lm: L. (L.) mexicana; Lg: L. (V.) guyanensis; Li: L. (L.) infantum; La: L. (L.) amazonensis; Lco: L. (V.) colombiensis; Leq: (L. (V.) equatorensis; Lla: L. (V.) lainsoni
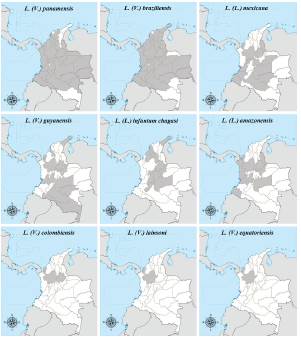
Figure 1 Geographical distribution by department of Leishmania species reported in Colombia, 1985-2017
Leishmania (V.) panamensis was identified in 39 of the 86 included studies. It was reported in 26 of the 32 Colombian departments. The departments with the highest number of reports of this species are, in order of frequency, Chocó (15/39), Antioquia (14/39), and Valle del Cauca (11/39), which are located in the western part of the country. According to the studies that included detailed information on the origin of the patients, L. (V.) panamensis was identified in 52 municipalities of 12 departments of Colombia. Of these municipalities, 28 belong to the department of Antioquia. There are no reports of this species in the departments of Amazonas, Atlántico, Cesar, La Guajira, and Quindío.
Leishmania (V.) braziliensis was reported in organisms from 26 departments. According to the 26 studies in which it was identified, the departments with the highest number of reports of this species are Meta (10/26), Cundinamarca (6/26) and Caquetá (6/26). At the municipality level, L. (V.) braziliensis was reported in 12 municipalities in the departments of Antioquia, Bolívar, Boyacá, Cauca, Nariño, Norte de Santander, Sucre, Tolima, and Valle del Cauca. The departments without reports of this species are Amazonas, Atlántico, Arauca, Guainía, Quindío, and San Andrés and Providencia.
According to the 8 studies in which L. (L.) mexicana was identified, the circulation of this species has been reported in 13 departments, of which Antioquia (4/8), Nariño (3/8), and Cundinamarca (2/8) have the greatest number of reports. There were only 3 studies with information at the municipality level; L. (L.) mexicana was reported in the municipalities of Gómez Plata in the department of Antioquia 12, Puerto López and Puerto Lleras in Meta 6, and Samaniego in Nariño 9.
Although L. (V.) guyanensis has a small geographical distribution (12 departments), this species has a greater number of circulation reports than L. (L.) mexicana. Leishmania (V.) guyanensis was identified in 20 of the 86 studies. The frequency of reports is higher in the departments of Caquetá (7/20), Tolima (5/20), and Putumayo (4/20), which are located in the southwestern part of the country. In total, there are 13 municipalities that reported the circulation of L. (V.) guyanensis, distributed in the departments of Amazonas, Caquetá, Meta, Putumayo, Sucre, Tolima, and Valle del Cauca.
Leishmania (L.) infantum was identified in 15 studies in organisms from 11 departments, including Córdoba (6/14), Cundinamarca (5/14), and Sucre (3/14), which have the highest number of reports of this species nationwide. The reports with detailed information of geographical origin come from 14 municipalities in 10 departments.
The 6 studies that report L. (L.) amazonensis indicate that the geographical distribution of this species is limited to the following 9 departments: Antioquia, Boyacá, Chocó, Meta, Nariño, Norte de Santander, Santander, Tolima, and Valle del Cauca. Of these, the department of Meta has the highest number of reports (4/6). In total, there are 12 municipalities in which L. (L.) amazonensis has been reported, distributed in the departments of Antioquia, Chocó, Meta, Nariño, Santander, Tolima, and Valle del Cauca.
To date, there are only two reports of L. (V.) colombiensis in the country 6,14. The samples came from patients from Río Grande and San Carlos municipalities of the department of Antioquia as well as from sand flies in the municipalities of El Carmen and San Vicente de Chucurí in Santander.
Leishmania (V.) lainsoni and L. (V.) equatorensis were recently reported by Ramirez, et al., both identified from patients from the region of Antioquia 6.
Studies with less detailed information on the origin of the patients report the circulation of L. (V.) braziliensis and L. (V.) panamensis in the Amazon, Andean, Pacific and Orinoquia regions and L. (V.) guyanensis in the Amazon and Andean regions 15. Likewise, the distributions of L. (V.) panamensis and L. (V.) braziliensis were reported in the Amazonas, Atrato, Cauca, Magdalena, Mira, Orinoco, Patía, and San Juan river basins, whereas L. (V.) guyanensis was reported in the Amazonas river basin 7,16.
Species typing techniques
To date, the parasites of Leishmania spp. in Colombia have been identified using different methods, including isoenzyme pattern analysis, monoclonal antibody typing, and other molecular biology techniques. Multi-Locus Enzyme Electrophoresis (MLEE) has been the most widely used technique for the identification of Leishmania spp. parasites in Colombia 4,17. MLEE is also used as a standard reference method for the confirmation of study findings 5,18.
In recent years, techniques based on the amplification of DNA using PCR, such as Restriction Fragment Length Polymorphism (RFLP) 19, have been valuable in the identification of these parasites and in the analysis of nucleotide sequences 6,10,20. In studies that use PCR for identification, the power of discrimination between species varies according to the molecular target. In reports in which species are identified to the genus, subgenus or species complex level, specific primers directed to kDNA minicircles were used 21,22. Other molecular targets that allow the discrimination of Leishmania species are the hsp70 gene 18,19, the cytochrome b gene (Cyt b) 6,20, the 7SLRNA gene 10,23 and the internal transcribed spacer 1 (ITS1) 18, and 16S rRNA 24.
Clinical forms and their etiological agents
Leishmania species in Colombia have been identified primarily from parasites isolated from lesions of cutaneous leishmaniasis. In total, there are 36 studies that used samples from patients with this clinical form. The incidences predominated, according to the number of reports, in the departments of Antioquia (10/36), Nariño (9/36), Meta (8/36), Tolima (8/36), Chocó (7/36), and Valle del Cauca (7/36).
The typing of species in the cutaneous leishmaniasis cases resulted in the identification of L. (V.) panamensis as the most frequent causative agent of this clinical form. This was followed by L. (V.) braziliensis, L. (V.) guyanensis, L. (L.) mexicana, L. (L.) amazonensis and, with the same number of reports, L. (L.) infantum, L. (V.) colombiensis, L. (V.) lainsoni, and L. (V.) equatorensis.
Rodríguez, et al., in 1985, and Corredor, et al., in 1990, reported the identification of L. (L.) mexicana and L. (L.) amazonensis4,17 from patients with diffuse cutaneous leishmaniasis from the departments of Meta and Nariño.
To date, there are few studies that include the typing of Leishmania spp. from patients with mucosal leishmaniasis in Colombia 25-27. Cases of mucosal leishmaniasis were reported in the departments of Caquetá, Chocó, Cundinamarca, Meta, Nariño, Putumayo, and Valle del Cauca. Only L. (V.) braziliensis, L. (V.) panamensis, and L. (V.) guyanensis have been identified as etiological agents of mucosal leishmaniasis.
Similarly, reports of species identified from patients with visceral leishmaniasis are scarce. Two papers have been published; the first, by Corredor, et al., does not indicate the geographical origin of the patient 4. The second study, by Mestra, et al., reported the development of visceral leishmaniasis in a patient with renal transplantation in Medellín 28. The genotyping of Leishmania species in these studies resulted in the identification of L. (L.) infantum4 and L. (L.) mexicana28.
Natural infection of sand flies
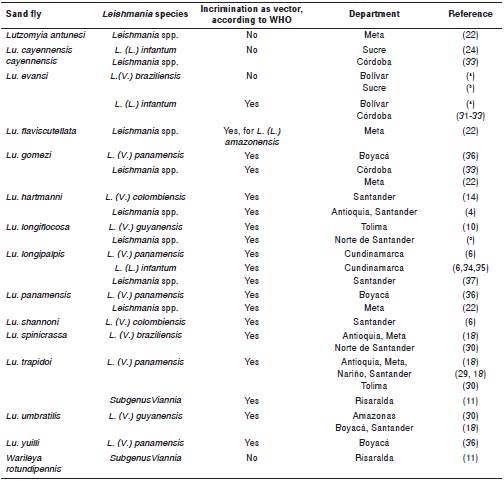
Twenty-three studies were published between 1987 and 2018 that reported the natural infection by Leishmania spp. in 15 species of sand flies from 13 departments (table 2). Lutzomyia evansi, Lu. longipalpis, Lu. spinicrassa and Lu. trapidoi were the most frequently reported species of sandflies. Of the 9 Leishmania species reported in the country, only L. (V.) panamensis, L. (V.) braziliensis, L. (V.) guyanensis, L. (L.) infantum, and L. (V.) colombiensis have been identified from sandflies (table 3).
Table 2 Reports of natural sand fly infection in Colombia
a Romero-Ricardo L, Pérez-Doria A, Rodríguez J, Vergara J, Montesino A, Martínez L, et al. Lutzomyia evansi como vector permisivo de Leishmania braziliensis y Leishmania infantum en el departamento de Bolívar, Colombia. Memorias, XVI Congreso Colombiano de Parasitología y Medicina Tropical. Biomédica. 2015;35(Supl.4):185.
b Pérez A, Romero L, Martínez L, Rivero M, Bejarano E. Aislamiento y tipificación de una cepa de Leishmania (Viannia) braziliensis a partir de Lutzomyia evansi en el municipio de Colosó, Sucre. Memorias, XVI Congreso Colombiano de Parasitología y Medicina Tropical. Biomédica.2 015;35(Supl.4):112-3.
c Cárdenas R, Gutiérrez R, Cabrera O, Santamaría E, Parada H, Mendoza F, et al. Lutzomyia longiflocosa (Psychodidae, Phlebotominae) infectado naturalmente con Leishmania spp. en una región endémica de leishmaniasis tegumentaria americana. Memorias, XX Congreso Latinoamericano de Parasitología. Biomédica. 2011;31:270.
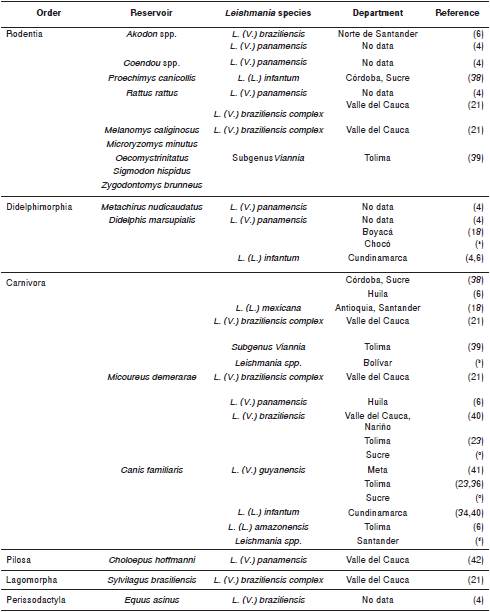
Table 3 Reports of natural infection of animal hosts in Colombia
a Carrillo-Bonilla L, Vélez I, Vélez-Mira A, Boite M, Cupolillo E. Estudio ecoepidemiológico de Didelphis marsupialis y Canis familiaris como posibles reservorios de Leishmania panamensis en un ciclo selvático y periurbano de Colombia. Memorias, XVI Congreso Colombiano de Parasitología y Medicina Tropical. Biomédica. 2015: 35(Supl.4):158-9.
b Zambrano P, Ayala M, Fuya P, Pérez J, Triana O, Cantillo-Barraza O. Estudios de reservorios silvestres en un brote de leishmaniasis visceral urbana en Cartagena, departamento de Bolívar. Memorias, XX Congreso Latinoamericano de Parasitología. Biomédica. 2011;31:297.
c Rivero M, Rodríguez J, Meza E, Pérez-Doria A, Bejarano E. Primer hallazgo de Leishmania guyanensis y Leishmania braziliensis en perros asintomáticos del foco urbano de leishmaniasis del municipio de Ovejas, Sucre. Memorias, XVI Congreso Colombiano de Parasitología y Medicina Tropical, Biomédica. 2015;35(Supl.4):113.
d Márquez LL, Luna KP, Ángulo VM. Detección de infección por L. chagasi en una población canina de un foco de leishmaniosis visceral en Santander. Biomédica. 2003;23:115.
Natural infection by L. (V.) panamensis, L. (V.) braziliensis, and L. (V.) guyanensis was detected primarily in Lu. trapidoi18,29,30, Lu. spinicrassa4,18,30, and Lu. umbratilis4,10,18,30, respectively, whereas reports of natural infection by L. (L.) infantum occurred primarily in Lu. evansi31-33 and Lu. longipalpis4,6,34,35. Infection with L. (V.) colombiensis in sand flies has only been reported in Lu. hartmani14 and Lu. shannoni6. Other species of sand flies in which a natural infection has been reported include Lu. longiflocosa by L. (V.) guyanensis10, Lu. cayennensis by L. (L.) infantum24, Warileya rotundipennis infected by parasites of the subgenus Viannia11, and Lu. antunesi, identified at the genus level 22.
Natural infection of animal hosts
Since 1988, there have been 19 studies involving the isolation and identification of Leishmania species in animal hosts in Colombia. The natural infection has been described in 16 mammalian species, among which rodents and marsupials predominate. Nine mammalian species have only a single report of natural infection, whereas others, such as Canis familiaris and Didelphis marsupialis, have several reports of infection. The typing of Leishmania spp. in these animals led to the identification of L. (V.) panamensis, L. (V.) braziliensis, L. (V.) guyanensis, L. (L.) infantum, L. (L.) mexicana, and L. (L.) amazonensis. Of these, L. (V.) panamensis has been identified in 7 of the 16 species of mammals, including D. marsupialis, C. familiaris, Choloepus hoffmanni, Rattus rattus, and species of the genera Akodon and Coendou (table 3).
Leishmania (V.) braziliensis and L. (V.) guyanensis have been primarily isolated from C. familiaris. Of the species of subgenus Leishmania, L. (L.) infantum has the highest number of reports of natural infection in animal hosts, including D. marsupialis, C. familiaris and Proechimys canicollis (table 3).
Discussion
In this review, the 86 reports of Leishmania species in Colombia were compiled (Annex 1). Our goal was to characterize the geographical distribution of the species causing the different clinical forms and to map the natural infection of sand flies and other animal hosts. This information is valuable to health authorities because it allows the determination of transmission foci so that proper prevention measures may be established. Additionally, it provides information for the development of new research related to the Leishmania species in Colombia.
In addition, this review enabled us to describe the geographical distribution of the nine species circulating in 29 of the 32 departments of the country, expanding the area described by Ramírez, et al., which included information only from 23 departments 6.
One limitation of this work is that in most of the studies included the geographical origin of the samples analyzed was not specified in detail, which is why the described distribution is limited to the department. Thus, it is not possible to relate the location of the species to the geographical and climatological variations of the country. If future reports provide the exact location of the samples, such as village (vereda) and municipality, the precise geographical distribution of the parasite species could be updated.
The circulation of nine species of Leishmania makes Colombia one of the countries harboring the highest number of species. According to the established geographical distribution, the departments of Antioquia, Santander, and Meta have the highest number of circulating species and the highest number of species identification reports. These three departments accounted for 28.8% of the cases of leishmaniasis reported to the Instituto Nacional de Salud during the year 2016, of which Antioquia reported the second highest number of cases of cutaneous leishmaniasis, and Meta reported the highest number of cases of mucosal leishmaniasis 2.
Among the species identified as causing cutaneous leishmaniasis in the country, reports of L. (L.) infantum occurred in patients from the departments of Boyacá, Caldas, Cundinamarca, La Guajira, Meta, and Santander 6. This article does not describe the clinical characteristics of the cases and indicates only that the patients included had cutaneous leishmaniasis. Despite the close relationship between L. (L.) infantum and visceral leishmaniasis, cases of cutaneous leishmaniasis by this species have been previously reported in countries in Latin America, including Brazil 43 and Nicaragua 44.
Twenty-seven percent of the species identification reports were derived from sand fly studies. Natural infection was detected in 15 species, of which 11 are listed by WHO as confirmed vectors of leishmaniasis in Colombia 45. Among these, Lu. evansi and Lu. longipalpis are confirmed vectors of L. (L.) infantum and Lu. trapidoi¸ Lu. spinicrassa and Lu. umbratilis are confirmed vectors of L. (V.) panamensis, L. (V.) braziliensis, and L. (V.) guyanensis, respectively 45. It is important to highlight the variety of sand fly species (Lu. trapidoi, Lu. gomezi, Lu. panamensis, Lu. yuilli and Lu. longipalpis) in which a natural infection by L. (V.) panamensis was detected, as this may be related to its wide distribution in the country.
The characterization of Leishmania spp. in mammals has been the least explored in the country. Of the animal species with reports of natural infection, many species of Leishmania have been identified in C. familiaris (table 3), which is listed as the main reservoir of L. (L.) infantum. Although there is evidence that this host plays a role in the transmission of parasites that cause cutaneous leishmaniasis, it is unknown whether C. familiaris acts as a reservoir or if it is an incidental host. Several species of mammals infected by Leishmania parasites have been reported in Colombia (table 3). Of the nine species of Leishmania circulating in Colombia, infection by L. (V.) colombiensis, L. (V.) lainsoni, and L. (V.) equatorensis have not been reported in animal hosts. As in Colombia, there are few reports of natural infection by these species in other Latin American countries.
This report gathered published information regarding the distribution of Leishmania spp. in Colombia from 1985 to 2017 and reveals that the available information is limited. Therefore, it is necessary to propose studies to identify the circulating species in endemic sites throughout the country that have not yet been reported and thus contribute to the control of the disease.
A possible strategy to update the species distribution map of Leishmania spp. in Colombia is to compile information on species typing and distribution in the country and thus create a consolidated map of available information. This would allow the areas in which there is no information on circulating species to be identified. It would be valuable to compare the distribution of the parasite species and the distribution of its vectors in the country 46.














