Urinary tract infections affect people of all ages and are one of the most frequently treated pathologies in primary healthcare centers. Although urinary infections can be caused by several species in the Enterobacteriaceae, most cases (both community and hospital-acquired) are produced by E. coli1,2. Infection rates by extended-spectrum β-lactamases (ESBL)-producing E. coli have increased in the last 10 years in Latin America, with some regions showing prevalences of up to 32%. In addition, 11 to 25% of these ESBL-producing E. coli infections are now resistant to third generation cephalosporins including important rates of multidrug resistance, and only the antibiotics carbapenems, tigecycline and colistin are showing susceptibility rates >90% 3.
ESBL-producing strains are also often resistant to antibiotics of other classes (sulfonamides, aminoglycosides, quinolones) thus complicating treatment strategies. The screening of ESBL-producing bacteria by antibiotic susceptibility testing is challenging, hence detection of specific genes by PCR is commonly used for final confirmation. The most common ESBL are the SHV, TEM, and CTX-M types, and the association of these three types of enzymes with E. coli infections has been investigated in many studies. CTX-M-type enzymes have been shown to be the most prevalent ESBL 4 and have been associated with numerous outbreaks of infections both in hospitals and in the community, and particularly, along with the SHV and TEM types, in urinary E. coli strains isolated from nonhospital settings 5. This has resulted in a change in epidemiological patterns with ESBL-producing strains appearing outside the hospital environment, thus converting them into an emerging public health problem 2,6. The frequencies of ESBL found in South America rank amongst the highest in the world with CTX-M dominant possibly due to poorer social and economic situations, hospital overcrowding, lack of antimicrobial stewardship, excessive over-the-counter antibiotic usage, and under-supported infection control practices 6.
In Venezuela, there are several reports of infections by ESBL-producing Enterobacteriaceae species from Caracas 7, Cumaná 8, Ciudad Bolívar 9 and Mérida 10, and the reports from Ciudad Bolívar and Mérida also describe ESBL-producing isolates detected from communities. In this context and given the increasing probability of dissemination of ESBL-producing strains in the community, the aim of the present study was to characterize multidrug-resistant E. coli isolates causing community-acquired urinary tract infections and the risk factors associated with the presence of ESBL in Cumaná, Venezuela.
Materials and methods
Bacterial isolates and patients
We evaluated a total of 103 E. coli isolates from patients attending the urology outpatient consultation and the emergency unit from January 1st through June 30th, 2014, at the Hospital Universitario “Antonio Patricio de Alcalá” in Cumaná, Estado Sucre, Venezuela. Urine samples from patients from both genders (20 males and 83 females) and different ages (ranging from 12 to 70 years) who showed urinary tract infection symptoms and indications for urine culture were examined for isolates. All patients were diagnosed with community-acquired urinary tract infection defined as previously suggested 11 as having abundant bacteria and polymorphonuclear leukocytes in the urine sample and positive urine culture with bacterial counts equal to or greater than 103 CFU/ml of urine when E. coli was identified. The urinary tract infections were classified as complicated or uncomplicated according to the guidelines established by the Infectious Diseases Society of America 12.
A community-acquired infection was defined according to the criteria proposed by Friedman, et al. 13, differentiating it from healthcare-associated infections and hospital-acquired infections, like an infection present at the moment of the consultation and when patients had not received any of the following: intravenous therapy at home, wound care or specialized nursing care administered by a healthcare agency, close family or friends, and self-administered intravenous medical therapy in the 30 days before the infection as well as those patients that did not attend a hospital or hemodialysis clinic, or received intravenous chemotherapy in the previous 30 days, or had been hospitalized in an acute care hospital for two or more days in the previous 90 days, or resided in a nursing home or long-term care facility.
Microbial susceptibility tests and detection of ESBL
Antimicrobial susceptibility and interpretation were evaluated using the disk diffusion susceptibility test according to the Clinical Laboratory Standards Institute 14. The antimicrobials tested (Oxoid Ltd., UK) were ampicillin (10 μg), cefalotin (30 μg), cefoxitin (30 μg), cefotaxime (30 μg), ceftazidime (30 μg), cefepime (30 μg), aztreonam (30 μg), piperacillin-tazobactam (100/10 μg), imipenem (10 μg), meropenem (30 μg), ampiciliin-sulbactam (10/10 μg) amoxicillin-clavulanic acid (2:1) (30 μg), nalidixic acid (30 μg), ciprofloxacin (5 μg), amikacin (30 μg), tobramycin (10 μg) and trimethropim-sulfamethoxazole (25 μg).
ESBL phenotypes were confirmed using the combined disc method 14 using E. coli ATCC 25922 and K. pneumoniae ATCC 700603 as the control strains. Multidrug resistance was defined as those isolates that showed resistance to ≥1 agents in ≥3 antimicrobial categories according to the consensus of a group of international experts 15.
Detection of the genes coding for β-lactamases
DNA was isolated by extraction using the Wizard Genomic purification kit™ (Promega). Resistant genes were identified by means of a PCR assay for blaTEM, blaSHV and blaCTX-M using the primers described elsewhere 16-18. The PCR products were electrophoresed in 2% agarose gel and stained with GelRed Nucleic Acid Stain™ (Biotium). A 100 bp DNA ladder (Fermentas, Lithuania) was used as the molecular weight marker.
Transfer of resistance
Conjugation assays were done in a solid medium using E. coli j62- 2 (resistant to rifampicin, CVCM 131) as the recipient 7. The clinical and recipient strains were grown separately in Luria-Bertani broth (Hardy Diagnostics, Santa Maria, CA, USA) at 37°C for 18 hours, and then mixed in a ratio of 1:4 (clinical isolates: recipient). Transconjugants were selected on MacConkey agar containing 100 μg rifampicin and 2 μg cefalotin.
Differentiation of the CTX-M group by PCR-RFLP
Restriction enzyme digestion was carried out according to Mahboobeh 19.The members of the CTX-M group were identified according to the fragments generated by double digestion by the PstI and PvuII enzymes. E. coli 2944NR was used as an RFLP positive control since it contains aCTX-M-1 type β-lactamase while E. coli J62-2 was used as a negative control. The RFLP products were observed in a 2% agarose gel containing GelRedNucleic Acid Stain™ (Biotium).
Statistical analyses
The risk factors considered in this study were: Nasogastric tube use, Foley catheter use, chronic kidney disease, cerebral vascular accident, bedridden, immunosuppression treatment, pregnancy, presence of any functional or structural urinary abnormality, diagnosis of a urinary tract infection within one year, antimicrobial treatment within three months, hospitalization within the previous three months but not within the previous 30 days, diabetes, and age over 60.
The risk factors associated with infection by an ESBL-producing E. coli isolate were determined firstly by using a binary logistic regression for each variable followed by multivariate analysis for those variables showing best relevance, in which the variables were considered as predictors of ESBL.
The analysis was performed using a stepwise selection of variables, and the area under the ROC curve was calculated to determine the model’s predictive ability. The statistical analyses were carried out using the statistical package for the social sciences (SPSS™, version 18, IBM Corporation).
Ethical aspects
The patients gave their written consent after they were informed of the risks and benefits of participating in the study and had answered an epidemiological questionnaire.
The treatment of the patients, the analysis of the isolates, and the information generated were conducted according to the bioethical and biosafety guidelines set out by the Comisión de Ética, Bioética y Biodiversidad of the Instituto de Investigaciones en Biomedicina y Ciencias Aplicadas «Dra. Susan Tai” at the Universidad de Oriente.
Results
The E. coli isolates (n=103) evaluated in this study showed high rates of resistance for the antimicrobials frequently used to treat patients with urinary infections, such as ampicillin (96.1%), cefalotin (59.4%) and ampicillin-sulbactam (24.8%), amoxicillin-clavulanate (25.7%), trimethoprim-sulfamethoxazole (39.6%) and ciprofloxacin (29.7%).
The isolates from the uncomplicated urinary tract infections (30.1%) showed significantly lower resistance compared to those from complicated urinary tract infections (figure 1).
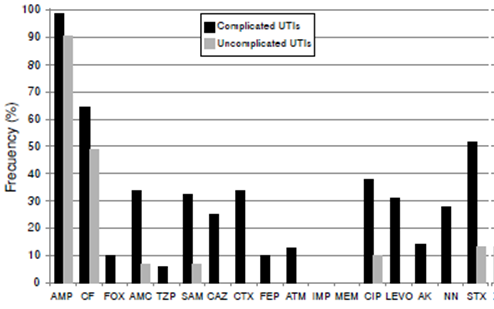
Figure 1 CF Frequency of resistant Escherichia coli isolates from patients with community-acquired urinary tract infections AMP: Ampicillin CF: Cefalotin; FOX: Cefoxitin; AMC: Amoxacillin-clavulanic acid; TZP: Piperacillin-tazobactam; SAM: Ampicillin-sulbactam; CAZ: Ceftazidime; CTX: Cefotaxime; FEP: Cefepime; ATM: Aztreonam; IMP: imipenem; MEM: meropenem; CIP: Ciprofloxacin; LEVO: Levofloxacin; AK: Amikacin; STX: Trimethoprim-sulfamethoxazole Note: Isolates with intermediate resistance were classified as resistant.
A total of 26 (25.2%) isolates were multidrug resistant (table 1), of which 21 (20.4%) showed production of ESBL. Of the 26 multidrug resistant isolates, 18 showed resistance to six or more antimicrobial categories, and the categories most associated with resistance were penicillins, cephalosporins, both with and without extended-spectrum, and folate pathway inhibitors (table 1). ESBL-producing isolates also showed a high frequency (66.7%) of simultaneous resistance to trimethoprim-sulphamethoxazole, fluoroquinolones and aminoglycosides compared to non-producing isolates (2.4%).
Table 1 Phenotypic and molecular characteristics of multidrug resistant Escherichia coli isolates. Here we show the DDST phenotypes of the bacterial isolates from patients with community-acquired urinary tract infections and their transconjugants, when appropriate, as well as the genes detected by PCR.
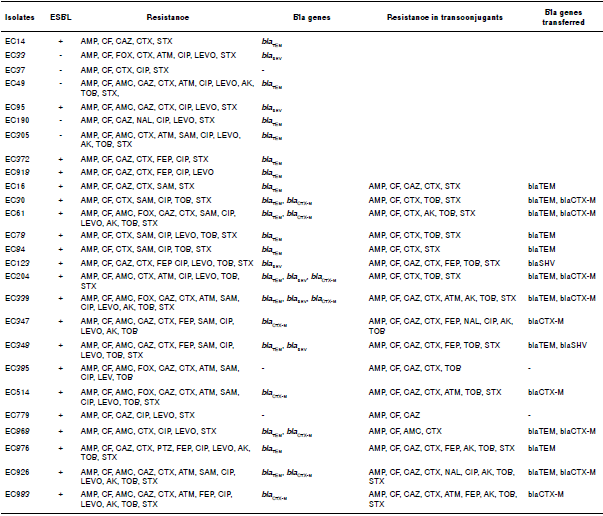
ESBL: Extended-spectrum β-lactamases; AMP: Ampicillin; CF: Cefalotin; AMC: Amoxacillin-clavulanic acid; FOX: Cefoxitin; CAZ: Ceftazidime; CTX: Cefotaxime; ATM: Aztreonam; SAM: Ampicillin-sulbactam; TZP: Piperacillin-tazobactam; FEP: Cefepime; CIP: Ciprofloxacin; LEVO: Levofloxacin; AK: Amikacin; TOB: Tobramycin; STX: Trimethoprim-sulfamethoxazole
The blaTEM gene was found in 17 isolates (65.4%) while blaCTX-M was detected in nine isolates (34.6%) and blaSHV in six isolates (23.1%). The blaTEM and blaSHV genes were found in E. coli isolates, ESBL-producing or not, while blaCTX-M was only found in ESBL-producing isolates. More than one gene was amplified in seven isolates: The most frequent combination was blaTEM + blaCTX-M (four isolates), and a three-gene combination was found in two ESBL producing isolates (table 1). The RFLP results revealed that five of the blaCTX-M genes were identified as belonging to the CTX-M-2 group and four to the CTX-M-1 group (figure 2).
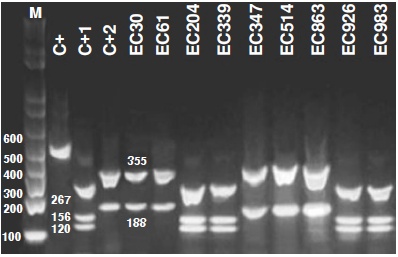
Figure 2 Digestion profile of the blaCTX-M gene detected in Escherichia coli isolated from patients with community-acquired urinary infections M: Molecular weight marker (1 kb Invitrogen); C+: Undigested blaCTX-M-2 fragment; C+1: Control blaCTX-M-1, strain 2944NR; C+2: Control blaCTX-M-2 Kp 22; lines 5-13: Isolates of Escherichia coli containing the blaCTX-M gene
Of the 26 multidrug resistant isolates resistant to third generation cephalosporins and subjected to in vitro bacterial conjugation, only 17 were able to transfer plasmids with resistance genes at a mean transfer rate of 10-7clinical isolates-transconjugant. Phenotypic analysis of the transconjugants demonstrated that part of the resistance pattern present in the clinical isolates was also observed in the transconjugants (table 1). All of the blaCTX-M genes were transferred to the transconjugant strain from the clinical isolates while only 64.7% (11/17) of the blaTEMgene and 33.3% (2/6) of the blaSHV were transferred (table 1). In the transconjugants of the two clinical isolates containing the three genes (204 and 339), the blaSHV gene was not transferred. These results demonstrate the transmissibility of bla genes to other E. coli strains.
When analyzing the risk factors for ESBL-producing E. coli, we found that an age over 60 years, complicated urinary tract infection, and urinary catheterization (more than 30 days previous to the infection) predisposed patients to an infection by a multidrug resistant/ESBL-producing E. coli strain (table 2) with relative risks (RR) 3.1 (95% CI: 1.5-6.4), 4.1 (95% CI: 1.1- 16.5),and 3.3 (95% CI: 1.6-6.8) times higher, respectively, for patients with those conditions compared to those without them.
Table 2 Epidemiological and clinical variables associated with ESBL-producing Escherichia coli
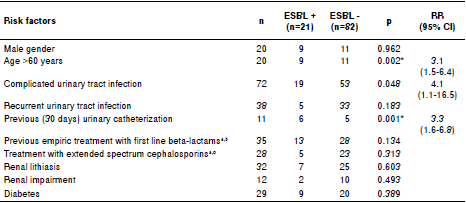
ESBL: Extended spectrum β-lactamases; RR: Relative risk; CI: Confidence interval
* Statistically significant
a Within three months
b First line β-lactams: AMP, SAM, and CF
c Extended spectrum cephalosporins: 3rd and 4th generation cephalosporins and monobactams (ATM)
Other risk factors, such as nasogastric tube use, cerebral vascular accident, bedridden patients, immunosuppression treatment, pregnancy, the presence of a structural urinary abnormality, and hospitalization within the previous three months were not analyzed since no ESBL-producing isolate was found in any of the patients showing these conditions.
Of the 20 male patients with complicated urinary tract infections, seven were aged over 60 with functional problems due to their prostate or kidneys and frequently attended the urology consultation for their control. All seven patients had urinary tract infections caused by ESBL-producing isolates. Of the 83 female patients with urinary tract infections, 53 were classified as complicated due to any of the abovementioned factors but with recurrent urinary tract infections within a year being the most frequent condition.
Discussion
The resistance of E. coli isolates from complicated urinary tract infections to many of the antimicrobials tested here indicates that treatment should only be given after susceptibility testing. High resistant rates to third-generation cephalosporins and aztreonam of clinical isolates of another bacteria, K. pneumoniae, have also been found in a previous study undertaken in Cumaná 12. The relatively high frequency of multidrug resistant E. coli found in the community and the high proportion of isolates showing resistance to ≥6 antimicrobials indicates the need to revise the treatment guidelines for urinary tract infections in Venezuela. A significant increase in the prevalence of multidrug resistant E. coli has also been reported in the US with rates raising from 9.1% in 2001 to 17.0% in 2010 20 and resistance to three, four or five antimicrobial agents. In the same study, widespread resistance was observed for trimethoprim-sulfamethoxazole (62.6%, 88.6%, and 97.9%, respectively) and ciprofloxacin (48.9%, 84.3%, and 98.2%, respectively).
Uncomplicated community-acquired urinary tract infections are normally treated empirically without undertaking a urine culture or an antibiogram unless they recur repeatedly 21. Our findings, however, demonstrate the importance of monitoring this empirical use of antimicrobials at a community level as recommended by the Infectious Diseases Society of America in order to select an appropriate empirical treatment 22.
β-lactam antibiotics are commonly the first choice of treatment against many microorganisms including uropathogens. Nevertheless, in recent years there has been a progressive increase in the frequency of E. coli strains from outpatients that characteristically show reduced susceptibility to penicillins and third generation cephalosporins due to the production of ESBL 23. This is now considered an emergent problem at the community level especially as changes in epidemiological patterns have been observed: While SHV and TEM have been shown to be the most prevalent enzymes in nosocomial strains, CTX-M is reported as predominant in community-acquired strains 24.
In this study, phenotypic characterization revealed that an important fraction of the isolates studied produced ESBLs. Here, the blaTEM gene was the most prevalent ESBL gene indicating the possible circulation of TEM-type ESBLs in strains from the community that have not been detected in nosocomial strains from the Hospital General de Cumaná12. We also found variations in the antibiotic resistance of isolates containing only blaTEM, which may suggest the presence of clavulanic-acid inhibited ESBLs not characterized in this study, or the presence of other blaTEM type genes. The non-ESBL-producing isolates that did contain the blaTEM gene are probably TEM-1 that confers resistance to penicillins and first-generation cephalosporins. Resistance to third-generation cephalosporins could then be due to other resistance mechanisms, for example, OXA-type enzymes which have been identified from some E. coli strains isolated from patients with community-acquired urinary tract infections in India 25. The blaSHV gene has been found to be less frequent in community-based strains than blaTEM and blaCTX-M 26.
The identification of the specific CTX-M enzyme type from the susceptibility pattern proved to be difficult due to the overlapping of the ceftazidime and cefotaxime phenotypes and the fact that several genes were present. The wide dissemination of CTX-Ms around the world has been referred to as the “CTX-M pandemic” since this enzyme is the most common β-lactamase carried by the Enterobacteriaceae that cause community onset urinary tract infections as shown in reports from different continents 2,24,27-31.
In Venezuela, there have been very few reports that identify the type of bla genes found in bacterial strains causing urinary infections. The CTX-M-32 enzyme (CTX-M-1) was identified in an E. coli strain isolated from a patient with diabetes from the Mérida state who was also suffering from a community-acquired urinary tract infection, which is the first report of this variant in South America 32.
It is important to note that some CTX-M enzymes are associated with specific countries: CTX-M-9 in Spain; CTX-M-1 in Italy and the United Kingdom, and CTX-M-2 in Israel, Japan, and most South American countries 24,33. In contrast, variants such as CTX-M-15 (CTX-M-1), which originated from the Asp240Gly substitution in CTX-M-3 and CTX-M-14 have been detected all over the world 24,34. The seasonal appearance and spread of these enzymes in different habitats may partially explain their epidemiology. The use of antimicrobials and other risk factors in different regions, as well as the characteristics of different geographical compartments, may have contributed to the current situation surrounding CTX-M.
The in vitro bacterial conjugation assays demonstrated that the genes coding for ESBL are localized in transferable plasmids which also carry other resistance determinants affecting antimicrobials, such as aminoglycosides, trimethoprim-sulfamethoxazole, and quinolones. Furthermore, the transfer of resistance to ciprofloxacin and nalidixic acid indicates that these strains contain a resistance mechanism against this group of antimicrobials that can disseminate horizontally as well as vertically. In India, 94% of the CTX-M-producing isolates were able to transfer their genes by conjugation with plasmids ranging in size from 120 to 272 kbp and half of these plasmids also carried the TEM-1 gene 25. This dissemination of ESBL in conjugative plasmids increases the possibility of an accelerated rate of proliferation 2.
Few studies have evaluated risk factors for community-onset ESBL infections and some of the studies previously undertaken in the U.S.A. were conducted prior to the emergence of community-wide multidrug-resistant E. coli (35). Here we identified age over 60 years, complicated urinary tract infections, and urinary catheterization as risk factors for infection with ESBL-producing E. coli strains. Other studies have also shown older age 35-40, urinary catheterization 36,37,39 and complicated urinary tract infections 40 as factors that increase the risk of acquiring a urinary tract infection by multidrug resistant bacteria.
In conclusion, our results reveal the presence of multidrug resistant isolates that cause community-acquired urinary infections. This is of great epidemiological importance and requires the intervention of the health authorities in the region to prevent further dissemination of these types of strains.














