The introduction of penicillin changed the natural history of syphilis: The wide array of clinical manifestations reported in the pre-antibiotic era was limited to a few case reports thereafter. However, there has been a resurgence of previously uncommon clinical presentations owing to the HIV epidemic. Here, we compare the type of bone involvement in secondary and tertiary syphilis in two HIV-infected patients.
Case 1
A 27-year-old HIV-infected male on antiretroviral treatment (ARV) with a CD4 count of 297 cells/mm3 and an undetectable viral load (<20 copies/ml) presented to the emergency unit with a three-week history of progressive frontal headache without any response to analgesics. He was diagnosed with secondary syphilis three months before and underwent incomplete treatment due to a severe anaphylactic reaction to penicillin.
On the physical exam, a 3 x 3 cm non-painful nodular lesion on his forehead and erythematous macules in his palms were observed. The Rapid Plasma Regain test (RPR) (1:32 dilutions) and the confirmatory test (Fluorescent Treponemal Antibody Absorption - FTA-ABS) were positive. Cerebrospinal fluid (CSF) studies revealed a glucose of 45 mg/dl, 20 white blood cells/ml, 61 mg/ dl of protein and a positive VDRL (1:8 dilutions). Computed tomography (CT) of the head revealed a lytic lesion in the left frontal bone (figure 1A).
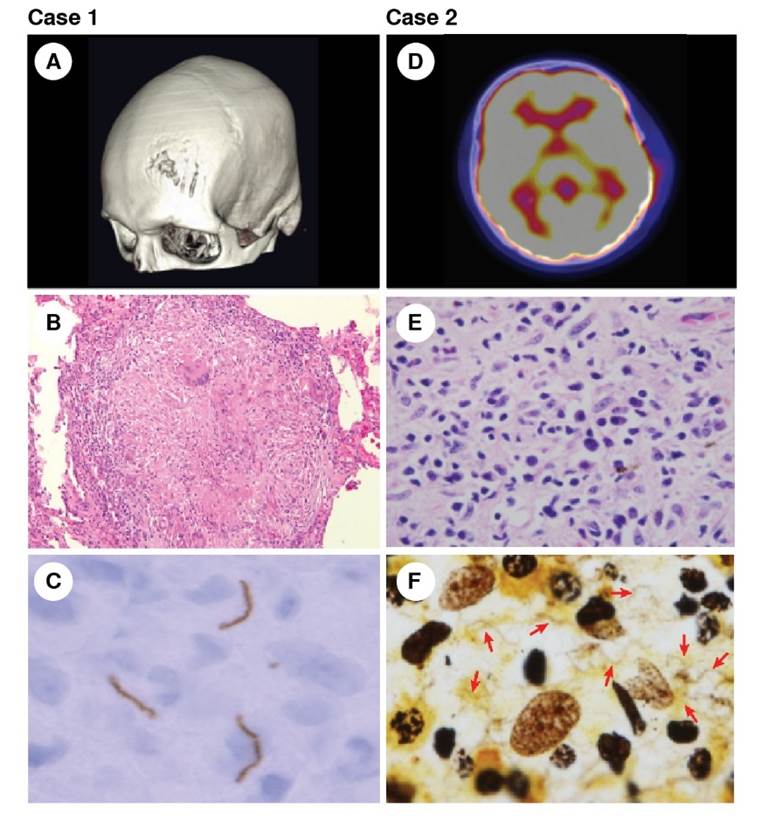
Figure 1 Left column: Case 1 - Tertiary syphilis. (A) Three-dimensional reconstruction of the skull computed tomography showing the bone lesion in the frontal bone. (B) Syphilitic gumma with chronic granulomatous infiltrate, hematoxylin eosin, 10X. (C) Immunochemistry of the lytic bone lesion showing spirochetes in the tissue. Right column: Case 2 - Secondary syphilis. (D) PET scan revealing lytic lesions with increased metabolism on the frontal and temporal bones. (E) Lymphoplasmocytic infiltrate in the bone biopsy, hematoxylin eosin, 100X. (F) Warthin-Starry stain revealing the presence of numerous spirochetes, 100X
The bone lesion biopsy revealed a chronic granulomatous process with no necrosis or perivascular lymphoplasmocytic infiltrate. Warthin Starry stain was negative, but immunohistochemical staining was positive for spirochetes (figure 1B). The lesion was cataloged as syphilitic gumma based on the chronic granulomatous infiltrate and the presence of spirochetes (figure 1C).
After completing the desensitization protocol, the patient started treatment with 4 x 106 units of intravenous penicillin every four hours. The patient completed a 14-day course and at the 6-month follow-up, resolution of the headache and all lesions was documented.
Case 2
A healthy 40-year-old male presented to the emergency unit with a 20- day history of pain in the right side of his rib cage, more intense at night, and weight loss.
In the physical exam, a painful nodular lesion on the right sixth rib was detected. A chest computed tomography (CT) showed a lytic lesion on the sixth rib. A bone scan and positron emission tomography (PET) revealed additional lytic lesions with increased metabolism on the frontal and temporal bones (figure 1D). A bone biopsy was performed.
During his hospital stay, the patient reported a new-onset headache, pain in the nodular lesion in his forehead, and a diffuse erythematous maculopapular rash on his palms and soles.
The bone biopsy showed a lymphoplasmocytic infiltrate without necrosis or granuloma formation (figure 1E). The Warthin Starry stain revealed the presence of numerous spirochetes (figure 1F). With this result, treponemal and non-treponemal tests were ordered, both with positive results (Venereal Disease Research Laboratory - VDRL 1:128 dilutions). Cerebrospinal fluid (CSF) studies revealed glucose levels of 57 mg/dl, 19 WBC/ml, and 36 mg/dL of protein; the CSF VDRL was negative. The ophthalmologic evaluation found vitritis and optic neuritis in the left eye. The HIV test was positive with a viral load of 74,534 copies/mL, and the CD4 count was 476 cells/ml.
The patient’s diagnosis was secondary syphilis with cutaneous involvement and neurosyphilis with ocular involvement. The patient started treatment with 4 x 106 units of intravenous penicillin every four hours for 14 days and ARV. Three months later, the lesions were no longer painful or clinically appreciable, the headache had resolved, and the ocular lesions had disappeared. Serum VDRL was positive but only at a 1:2 dilution and CSF parameters were all normalized.
In a literature review from 1946 to 2022, we found 39 published cases of bone involvement in non-congenital syphilis (table 1). Most of these cases were reported as secondary syphilis (34 cases, 87%), only four cases were tertiary syphilis, and one was considered as late latent syphilis. The mean age at presentation was 34 years (20-60 years) and only 13% of patients were women; 30% (10) of cases were reported in HIV-infected patients with an average CD4 count of 367 cell/mm3 (130689 cell/mm3). The most frequent radiographic finding was lytic lesions, mainly in the frontal and parietal bones (18 cases, 47%), followed by the tibia (45.9%).
Table 1 Published cases of bone involvement in non-congenital syphilis and the two cases presented here
| Authors (Year) | Age sex | HIV status | Radiographic examination | Localization of lesions | Symptoms and signs | Stage of syphilis | Treatment | Length of treatment | Response |
|---|---|---|---|---|---|---|---|---|---|
| Lefkovits AM, et al. (1946) | 22/M | No | Nodular lesion and erosion of the outer layer | Skull | Headache, alopecia, generalized lymphadeno-pathy | Secondary | Procaine penicillin G | Two and a half weeks | Decreased in size at three months |
| Kellock IA, et al. (1956) | 47/M | No | Mixed lytic and sclerotic lesion | Skull, tibia, humerus, femur, elbow | Bone pain, weight loss, headache | Secondary | Benzathine penicillin G | Ten days | Improvement of images at five months |
| Bauer MF, et al. (1967) | 26/W | No | Osteolytic lesion in frontal bone | Frontal bone | Headache, maculopapular rash | Secondary | Procaine penicillin G | Ten days | Partial resolution at three months |
| Parker JDJ. (1972) | 35/M | No | Periosteal reaction | Tibias | Leg pain with paraesthesia of the ankles | Secondary | Cephalori-dine | Two weeks | Almost complete resolution of images at 11 months |
| Tigh RR, et al. (1976) | 20/M | No | Multiple areas of increased uptakea | Skull, sternum, and clavicle | Headache, myalgia, maculo-papular rash, cervical lymphadenopathy | Secondary | Benzathine penicillin G | Ten days | Loss at follow-up |
| Longstreth P, et al. (1976) | 30/M | No | Bone resorption of the distal clavicle | Clavicle | Headache, shoulder pain, alopecia, splenomegaly | Secondary | Benzathine penicillin G | Three weeks | Recalcification at one month |
| Erlich R, et al. (1976) | 25/M | No | Multiple lytic lesions | Tibia, fibula, ulna, radius | Headache, myalgia, ankle pain, maculopapular rash | Secondary | Benzathine penicillin G | Two and a half weeks | Imaging resolution at three months |
| Dismukes WE, et al. (1976) | 32/M | No | Multiple osteolytic lesions | Clavicle, frontal and parietal bone | Headache, fever, weight loss, generalized lymphadenopathy, maculopapular rash | Secondary | Procaine penicillin G | Ten days | Asymptomatic |
| Shore RN, et al. (1977) | 37/M | No | Multiple lytic lesions | Tibia, fibula, radius, and ulna bilaterally | Pain in leg, ankles and arms, maculo-papular rash | Secondary | Procaine penicillin G | Ten days | -- |
| Graudal C, et al. (1981) | 42/M | No | Osteitis changesa | Tibia | Left leg pain, fever, sore throat, weight lost | Secondary | Benzathine penicillin G | Ten days | Imaging resolution after treatment |
| Petersen LR, et al. (1983) | 48/M | No | Diffuse increased activitya | Ribs, long bones, and spine | Leg and back pain, headache, papular rash | Secondary | Parenteral penicillin G | Ten days | Asymptomatic at two months |
| Hansen K, et al. (1984) | 31/M | No | Multiple areas of increased uptakea | Parietal, occipital, maxillary, mandibular, ribs, humerus, femur | Headache, fever | Secondary | Benzathine penicillin G | Five months | 50% reduction in activity at nine months |
| Veerapen K, et al. (1985) | 35/W | No | Increased uptakea | Frontal bone and tibia | Neck and leg pain | Secondary | Procaine penicillin G | Ten days | No changes in the images at six months |
| Meier JL, et al. (1986) | 37/M | No | Increased activitya | Tibias | Fever, leg pain, headache | Early syphilis | Penicillin | Ten days | Asymptomatic at one year |
| Rodriguez S, et al. (1988) | 39/M | No | Dense bony sclerosis | T10, L1 and L5 vertebral bodies | Weight loss | Tertiary | Procaine penicillin G | One month | Asymptomatic at three months |
| Ollé-Goig JE, et al. (1988) | 32/W | No | Multiple diffuse intracortical destructive lesions | Tibias, fibulas | Leg pain, weight loss, headache | Secondary | Procaine penicillin G | Ten days | Asymptomatic at six months |
| 21/M | No | Osteolytic lesión | Frontal and parietal bone | Asthenia, headache, generalized lymphadenopathy, maculopapular rash | Secondary | Benzathine penicillin G | Ten days | Asymptomatic at two months | |
| Middleton S, et al. (1990) | 31/M | No | Increased uptakea | Tibias, ulnas, and frontal bone | Leg and forearm pain | Secondary | Benetha- mine penicillin | Ten days | Imaging resolution at four months |
| Kastner RJ, et al. (1994) | 25/M | No | Increased uptakea | Ulna, skull, and radius | Maculo-papular rash, generalized lymphadenopathy | Secondary | Procaine penicillin G | Two weeks | Markedly diminished uptake at 30 days |
| Chung KY, et al. (1994) | 29/W | No | Round osteolytic lesions | Frontal, temporal, and parietal bones | Headache, maculopapular rash | Secondary | Benzathine penicillin G | Three weeks | |
| Rademacher | 27/W | No | Periosteal elevation | Tibias, calcaneus | Headache, fever, | Secondary | Intrave-nous | Two weeks | Lost at follow-up |
| SE, et al. (1996) | 34/M | Yes | with periostitis Cortical thickeninga | Tibias | ulcerative rash, and shin and heel pain Fever, chills, night sweats, weight loss, painful skin lesions | penicillin G Intrave-nous penicillin G then benzathine penicillin | One month | Asymptomatic at nine months | |
| Gurland IA, et al. (2001) | 20/M | Yes | Multiple lytic lesions | Skull | Painful nodules | Secondary | Procaine penicillin G | Three weeks | -- |
| Coyne K, et al. (2006) | 36/M | Yes | Periostitis | Humerus, femur, tibia, fibula, and skull | Headache, fever, and sweats, maculopapular rash | Secondary | Benzathine penicillin G | Two weeks | Imaging resolution at three months |
| Huang I, et al. (2007) | 40/M | Yes | Multiple lytic lesions, “worm eaten” appearance | Frontal and parietal bone | Headache | Secondary | Penicillin | One and a half months | Asymptomatic resolution at 1.5 months |
| Kandelaki G, et al. (2007) | 20/M | Yes | Destructive lesion | Sternal bone | Painful lump on chest and maculo-papular rash | Secondary | Procaine penicillin G | Two weeks | Imaging resolution at six weeks |
| Denes E. (2009) | 37/M | Yes | Increased uptakea | Tibia, radius, and skull | Leg pain, loss of appetite and weight, skin ulcerations | Secondary | Benzathine penicillin G | Six weeks | Asymptomatic at two months |
| Naraghi AM, et al. (2010) | 64/M | Yes | Hetero-geneous activitya | Tibias, fibula, femur, skull, orbit | Leg pain | Early syphilis | Benzhatine penicillin G | Three weeks | Imaging resolution at three years |
| Samarkos M, et al. (2011) | 25/M | Yes | Increased uptakea | Skull, ribs | Headache, maculopapular rash | Secondary | Intrave-nous penicillin G | - | Imaging resolution at three months |
| Liu Z-Y, et al. (2011) | 62/M | No | Focal osteolytic lesions and onionlike periosteal reaction | Tibia and fibula | Leg pain | Late latent syphilis | Penicillin G | One and a half months | Imaging resolution at 1.5 months |
| Egan KM, et al. (2012) | 41/M | No | Increased enhancementa | Skull | Headache and papular rash | Secondary | Procaine penicillin G | Two weeks | Asymptomatic at three months |
| Boix V, et al. (2013) | 40/M | Yes | Osteolytic lesions and increased uptakea | Skull, humerus, and ulna | Fever, headache, weight loss, generalized lymphadenopathy | Secondary | Doxycy-cline and azithromycin | Four months | Imaging resolution at four months |
| Alraddadi B, et al. (2013) | 32/M | - | Osteolytic lesion | Skull | Headache | Secondary | Intrave-nous penicillin G | Two weeks | Asymptomatic at two weeks |
| Park KH, et al. (2014) | 41/M | No | Bone destruction and extra-skeletal soft tissue formation | Multiple ribs and L5 vertebra | Weight loss, maculopapular rash, and generalized lymphadenopathy | Secondary | Benzathine penicillin | Three weeks | Decreased uptake at six months |
| Bezaley S, et al. (2014) | 20/M | No | Multiple osteolytic and sclerotic lesions with periosteal reaction | Tibia, 11th rib, parietal bone, acromioclavicular joint, and sacroiliac joint | Weight loss, leg, shoulder and rib pain, headache, maculopapular rash | Secondary | Penicillin | - | Asymptomatic at one month |
| Manríquez J, et al. (2014) | 50/M | No | Increased uptakea | Tibia | Leg pain, maculopapular rash, generalized lymphadenopathy | Secondary | Benzathine penicillin G | Three weeks | - |
| Bai Y, et al. (2017) | 44/M | No | Osteolytic lesion and new bone formation | Bodies of L4 and L5 vertebras | Low back pain, numbness below the knees, and inability to walk | Tertiary | Benzathine penicillin G | Three weeks | Imaging resolution at 12 months |
| Kamegai K, et al. (2022) | 30/M | Yes | Osteolytic lesion | Sternum and ribs | Chest pain | Tertiary | Ceftriax-one | 13 weeks | Magnetic resonance imaging (MRI) showed abnormal signals |
| Jankowska L, et al. (2022) | 20/W | Osteolytic lesion | Clavicule | Skin lesions, uveitis, bone pain | Tertiary | Penicillin | 14 weeks | Reduced tumor was observed |
a Bone scintigraphy
Twenty patients presented headache (51%), bone pain (48%) and maculopapular rash (17 patients, 43%). Among the five patients with tertiary or late latent syphilis, bone pain was the most frequent symptom (4/5 patients). Of the 39 patients, 35 (89%) were treated with intravenous penicillin, 17 (43%) with intramuscular procaine penicillin, and 14 (35%) with benzathine penicillin. The mean treatment duration was 24.6 days (10-150 days). No treatment failures were reported.
According to Resolution 8430 of 1993 of the Colombian Ministerio de Salud, the present report implied no risk: it used retrospective documentary research methods and information from medical records. The patients gave their informed consent, and it had the approval of the institutional ethics committee. There was no intervention or intentional modification of the patients’ biological, physiological, psychological, or social variables, and their dignity, well-being, and confidentiality were respected. Our research follows the bioethical principles of beneficence, non-maleficence, respect, autonomy, and justice.
Discussion
The differential diagnosis of bone lesions in adult HIV-infected patients varies according to the age of the patient, the number, and the characteristics of the lesions. Non-infectious etiologies for patients under the age of 40 include primary bone tumors such as enchondromas, giant cell tumors, osteoblastoma, and osteosarcoma, among others; in those older than 40, non-infectious etiologies include hyperparathyroidism, enchondromatosis, Langerhans cell histiocytosis, multiple myeloma, and metastatic lesions.
In contrast, infectious etiologies vary according to the severity of imm3unosuppression. In patients with CD4 counts of less than 200 cells/ mm , infectious etiologies such as bacillary angiomatosis and disseminated Mycobacterium haemophilum infection could be considered. Tuberculosis, syphilis, and lesions due to bacterial osteomyelitis can appear independently of the patient's CD4 count 1,2.
Since the advent of highly active antiretroviral therapy, cases of syphilis have been increasing due to changes in sexual behavior 3. This growing incidence, coupled with more aggressive and atypical presentations in HIV- infected patients, explains why more exotic forms of the disease are being reported again 4,5.
Although syphilitic spirochetes have a significant affinity for bone 6, bone involvement is an infrequent clinical manifestation representing only up to 8.7% of the lesions, actively looked for with X-rays in patients with secondary syphilis 7. Treponemes can cause bone involvement during all disease stages. During spirochetemia, treponemes can disseminate through Haversian canals in the bone marrow until they reach the periosteum and produce periostitis. This initial lesion can progress and produce a lytic or blastic one. Depending on the degree of cortical destruction, these changes will manifest according to time as osteitis, osteomyelitis, or gumma 8.
The most affected bones are the long bones, the cranium, and the ribs; within the cranium, the frontal and parietal bones are most involved 9. Characteristically, lesions are painful and often represent the only clinical sign 10. A maculopapular rash may be seen concomitantly in 60% of patients during secondary syphilis. However, during tertiary syphilis, associated clinical findings are rare 11.
Differentiating bony lesions of secondary versus tertiary syphilis is not possible on clinical or radiologic grounds alone. The presence of cutaneous lesions does not help to differentiate the stage of bony lesions, as these can recur in patients with tertiary syphilis, as happened in the first case reported herein. Only histologic findings can help clarify the stage of the lesion. Chronic granulomatous inflammation with or without necrosis characterizes gummatous lesions, whereas lesions in secondary syphilis classically display perivascular lymphoplasmocytic infiltrate. Spirochetes are only visualized in 36% of bone lesions during secondary syphilis and are seen even less frequently during tertiary syphilis 11. The two cases we present here displayed typical histologic findings for the respective stage of the disease, and the presence of spirochetes in bone tissue was confirmed in both.
Although it is not clear whether bone lesions should be treated as another bacterial osteomyelitis or according to the stage of syphilis, all reported cases were treated with penicillin for two or more weeks as authors expressed concerns about beta-lactam penetration to bone 11. The treatment for early disease stages of syphilis is 2,4 x 106 units of benzathine penicillin, but there are no clinical studies to guide the treatment for bone compromise during these early stages 12. Although follow-up time and type (clinical or radiological) vary according to the case, no treatment failures were reported 11. In contrast, the guide for treating syphilitic gumma as any other tertiary syphilis manifestation is clear: 2,4 x 106 units of benzathine penicillin weekly for three weeks. Given the lack of data regarding bone lesion-specific treatment and response, it is important to determine the type of bone compromise regardless of the symptoms to rule out neurosyphilis in tertiary syphilis 12.
Here we presented the cases of two HIV-infected patients with different stages of bone involvement in syphilis. Although the clinical presentation of both cases was typical, syphilis-related with bone involvement was not initially suspected since clinicians are not used to with this type of compromise. As secondary versus tertiary syphilis bone lesions cannot be differentiated based on clinical or radiologic findings alone, clinicians should consider syphilis in the differential diagnosis of blastic or lytic bone lesions, especially in HIV- infected patients.














