Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307On-line version ISSN 2216-0280
Invest. educ. enferm vol.30 no.2 Medellín July/Dec. 2012
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Improvement of self-care behaviors after a nursing educational intervention with patients with heart failure
Mejoramiento en los comportamientos de autocuidado después de una intervención educativa de enfermería con pacientes con falla cardíaca
Melhoramento nos comportamentos de autocuidado depois de uma intervenção educativa de enfermagem com pacientes com falha cardíaca
Edith Arredondo Holguín1; María de los Ángeles Rodríguez Gázquez2; Lina Marcela Higuita Urrego3
1 RN, M.Sc. Professor, Faculty of Nursing, Universidad de Antioquia, Colombia. email: tapua412@udea.edu.co.
2 RN, Ph.D. Professor, Faculty of Nursing, Universidad de Antioquia, Colombia. email:mariangelesrodriguezg@hotmail.com.
3 Nursing student. Faculty of Nursing, Universidad de Antioquia, Colombia. email: linamarcerla-17@hotmail.com.
Receipt date: December 19th 2011. Approval date: March 23rd 2012.
Subventions: Comité para el Desarrollo de la Investigación -CODI- de la Universidad de la Universidad de Antioquia.
Conflicts of interest: none.
How to cite this article: Arredondo -Holguín E, Rodríguez-Gázquez MA, Higuita-Urrego L. Improvement of self-care behaviors after a nursing educational intervention with patients with heart failure. Invest Educ Enferm. 2012;30(2): 188-197.
ABSTRACT
Objective. To evaluate the improvement in self-care behaviors after a nursing educational intervention in patients with heart failure. Methodology. The study had the participation of 29 patients over 30 years of age, who attended in 2010 the cardiovascular healthcare program of a hospital institution in Medellín (Colombia) and who signed the informed consent and received for nine months a nursing educational intervention consisting of group educational meetings, telenursing sessions, home visits, and support leaflet. The study applied Artinian's Self-care scale validated in the field, composed of 28 items distributed in four dimensions (request for help, adaptation to disease, and adherence to pharmacological and non-pharmacological treatments). To evaluate changes in these behaviors, the scale was applied at the beginning and end of the study. Results. Bearing in mind that the maximum possible score in the scale is 84, the patients had initial and final median scores of 40 and 53 (p < 0.05). The dimensions in which the most positive changes were observed were: request for help, adaptation to the disease, and adherence to the pharmacological treatment; regarding adherence to the non-pharmacological treatment, two behaviors did not obtain favorable changes (reduction in salt intake and measurement of the amount of urine eliminated). Conclusion. The nursing educational intervention conducted in our study had beneficial effects on most of the self-care behaviors assessed in individuals with HF.
Key words: heart failure; self-care; education, nursing.
RESUMEN
Objetivo. Evaluar el mejoramiento en los comportamientos de autocuidado después de una intervención educativa de enfermería en pacientes con Falla Cardiaca (FC). Metodología. Participaron 29 pacientes de 30 y más años quienes asistieron en 2010 al programa de salud cardiovascular de una institución hospitalaria de Medellín (Colombia). A su vez, firmaron el consentimiento informado y recibieron durante nueve meses una intervención educativa de enfermería consistente en encuentros educativos grupales, sesiones de teleenfermería, visitas domiciliarias y cartilla de apoyo. Se aplicó la Escala de autocuidado de Artinian validada en el medio, compuesta por 28 ítems distribuidos en cuatro dimensiones (solicitud de ayuda, adaptación a la enfermedad y adherencia a los tratamientos farmacológico y no farmacológico). Para la evaluación de los cambios en estos comportamientos, se aplicó al inicio y terminación del estudio. Resultados. Teniendo en cuenta que el puntaje máximo posible de obtener en la escala es de 84, los pacientes tuvieron una mediana en los puntajes inicial y final de 40 y 53 (p < 0.05). Las dimensiones en que más cambios positivos se observaron fueron: solicitud de ayuda, adaptación a la enfermedad y adherencia al tratamiento farmacológico; en cuanto a la adherencia al tratamiento no farmacológico hay dos comportamientos que no tuvieron cambios favorables: reducción en el consumo de sal y medir la cantidad de orina eliminada. Conclusión. La intervención educativa de enfermería realizada en nuestro estudio tuvo un efecto beneficioso en la mayoría de los comportamientos de autocuidado evaluados en las personas con FC.
Palabras clave: insuficiencia cardíaca; autocuidado; educación en enfermería.
RESUMO
Objetivo. Avaliar o melhoramento nos comportamentos de autocuidado depois de uma intervenção educativa de enfermagem em pacientes com Falha Cardíaca (FC). Metodologia. Participaram 29 pacientes de 30 e mais anos que assistiram em 2010 ao programa de saúde cardiovascular de uma instituição hospitalar de Medellín (Colômbia) que assinaram o consentimento informado e receberam durante 9 meses uma intervenção educativa de enfermagem consistente em encontros educativos grupais, sessões de tele-enfermagem, visitas domiciliárias e cartilha de apoio. Aplicou-se a Escala de autocuidado de Artinian validada no meio, composta por 28 itens distribuídos em quatro dimensões (solicitação de ajuda, adaptação à doença e aderência aos tratamentos farmacológicos e não farmacológicos). Para a avaliação das mudanças nestes comportamentos se aplicou ao início e terminação do estudo. Resultados. Tendo em conta que a pontuação máximo possível de obter na escala é de 84, os pacientes tiveram uma média nas pontuações iniciais e finais de 40 e 53 (p < 0.05). As dimensões em que mais mudanças positivas se observaram foram os de solicitação de ajuda, adaptação à doença e aderência ao tratamento farmacológico; quanto à aderência ao tratamento não farmacológico há dois comportamentos que não tiveram mudanças favoráveis (redução no consumo de sal e medir a quantidade de urina eliminada). Conclusão. A intervenção educativa de enfermagem realizada em nosso estudo teve um efeito benéfico na maioria dos comportamentos de autocuidado avaliados nas pessoas com FC.
Palavras chaves: insuficiência cardíaca; autocuidado; educação em enfermagem.
INTRODUCTION
Worldwide, heart failure (HF) is considered a serious public health problem due to its high morbidity and mortality1 and because of the huge economic and social costs it generates for patients, their families, healthcare services providers, and society in general.2 The extreme fatigue these patients endure, given the low perfusion of body tissue, influences on the deterioration of the quality of life and on the personal and social roles, also leading to the progressive loss in the capacity for self care;3 thereby, one of the main challenges for nursing professionals who plan the care of individuals with HF is to improve their self-care. This is defined by Orem as the practice of behaviors individuals carry out on their own, consciously and permanently for maintenance of life, development, health, and welfare, which when done efficiently contribute specifically to the structural integrity, functioning and human development.4,5 Self-care is a key aspect in treating HF, which is why in most care programs prioritize these behaviors related to a better prognosis in the evolution of disease.6
It is known that the main risk factors of HF associated to behavior - cigarette smoking, dyslipemia, obesity, and sedentary lifestyle -7 are susceptible to intervention with the aid of educational programs, which results in the patient's improved functional status and reduction of the probability of readmission and premature death.8-11 Educational interventions with these individuals must include diverse pedagogical strategies that enhance knowledge and impact upon their self-management and management of their disease,12 while reducing the probability of readmission due to HF. 8,13 Regarding the type of personnel offering the educational intervention to individuals with HF, it has been noted that nursing professionals with knowledge of the disease, teaching, and evaluation of self-care behaviors determine the success of the program and the evolution of the patients.14
This study sought to evaluate improvement in self-care behaviors after a nursing educational intervention in patients with HF.
METODOLOGY
This was an intervention study with before and after evaluation, with the participation of 29 patients over 30 years of age who attended in 2010 to the cardiovascular healthcare program of a hospital institution in Medellín (Colombia), with diagnosis of HF confirmed via echocardiography, clinical symptomatology, in functional class I to III from the New York Heart Association (NYHA), without alteration of conscience and who were not in terminal phase. The patients who accepted to participate in the research signed the informed consent and received the nursing educational intervention. This study assumed the definition of self-care behaviors by Orem as the intentional actions to accomplish a goal, aimed at sustaining, protecting, and promoting human functioning.4
The instruments used to gather information were: a) Survey of basic social and clinical conditioning, which contains information on: demographics (age, sex, marital status, occupation, and schooling); social support (family, friends, and healthcare institution); and clinical data (co-morbidity, functional class, ejection fraction, hospitalizations, and death). b) Self-care scale: to evaluate changes in self-care behaviors, Artinian's Heart Failure Self-Care Behavior Scale (HFSCBS)15 was used, which is derived from the self-care deficit theory by Dorothea Orem, which was validated for Colombia by Arredondo and Rodríguez,16 with Cronbach's alpha of 0.76 (men: 0.73 and women: 0.77). This scale comprises 28 items to measure the frequency of self-care behaviors, distributed into four dimensions (request for help, adaptation to living with the disease, adherence to the pharmacological treatment, and adherence to the non-pharmacological treatment). The response options are Likert-type responses and have four levels for the questions: 0 = never, 1 = a few times, 2 = almost always, and 3 = always. To score the scale, the score for each item is added; the higher the score, the higher the level of self-care, with 82 being the maximum score.
The researchers gathered the information. Data on the HFSCBS was self-reported by the patient and that related to clinical variables was obtained directly from the clinical history. The control mechanisms considered of the quality of information were the following: a) standardization of the nursing professionals participating in the investigation in tasks of enrolling the patients, application of the questionnaire, telenursing, home visits, and educational activity; b) pilot test with nine patients of the study's complete methodology; c) supervision by the main researchers of the activities carried out by the rest of the team, and d) detection of typing errors by comparing one of every ten records from the database to the information gathering instrument in which the data were filled in.
The educational activities that were part of the intervention were aimed at individuals with HF and their families. The five priority aspects for the educational intervention were: 1) knowledge of the disease, 2) adherence to the pharmacological and non-pharmacological treatment, 3) request for help during the disease, 4) adaptation to living with the disease and the effects of the medications, and 5) the self-concept as an element that permits empowering and motivating individuals for their care and their management of the resources for their process of adaptation to living with the disease.
The nursing educational program received by the patients lasted nine months in which these activities took place: a) group educational meetings during the 1st and 8th months, b) a telenursing session during the 2nd, 3rd, 4th, 5th, 6th, and 7th months, and: c) home visits during the 1st and 8th months, and group workshops with the topic of ''Developing self-care behaviors during HF'' on the 2nd and 9th months. To support the intervention activities, the educational leaflet ''Developing self-care behaviors: a way of facing HF'' was designed. Information from the HFSCBS was collected during the start of the study and before the final group meeting.
For the statistical analysis, the information gathered was analyzed with the SPSS program vr 19.00 (Chicago, USA). The analysis plan was carried out according to the objectives proposed. The general description of the study group was made with proportions for the qualitative variables and through the median and interquartile range for the quantitative variables. For the purpose of analyzing the difference of scores between the evaluations before and after the educational intervention, the Wilcoxon signed-rank test was used; assuming statistical significance if the probability value was less than 0.05.
This research was endorsed by the Research Technical Committee of the Faculty of Nursing at Universidad de Antioquia. The main ethical aspects considered were: signed informed consent and confidentiality of the information taken for the investigation. The ethical principle of beneficence was fulfilled with the education imparted during the home visits, the educational meetings, and the telenursing. Upon detecting patients' needs that had to be taken care of immediately health education was given and, whenever necessary, the patient was advised to attend to medical consultation. This study received code COL321 from the Latin American Registry of Clinical Trials in Course (LATINREC, for the term in Spanish) from the Iberian American Cochrane Network.
RESULTS
This study had the participation of 29 individuals who were subjected to educational intervention in nursing and received the two evaluations of the self-care behaviors, before and after the intervention. The general characteristics for this group were the following: individuals with a mean age of 65 years; 55.2% were women; 51.7% were married, followed widows/widowers (20.7%); 14.2% were single, 6.9% lived with a partner, and 3.4% were separated. Regarding socio-economic level, 93.1% were in a socio-economic level of 3 or lower; 69.0% had elementary schooling or higher; 65.5% reported household chores as their main current activity, followed by paid work (6.9%) and recreational activities (3.4%); 31.0% did not engage in any activity; and 75.9% receive support mainly from the family, 41.4% from healthcare institutions, and 13.8% from friends.
With respect to clinical variables, most were patients in functional class NYHA 2 or 3 (41.4% each) and the rest were class 1 (17.2%); 34.3% had an ejection fraction below 50% and presented as main co-morbidities: hypertension (86.2%), congestive heart disease (37.9%), and diabetes mellitus (27.6%).
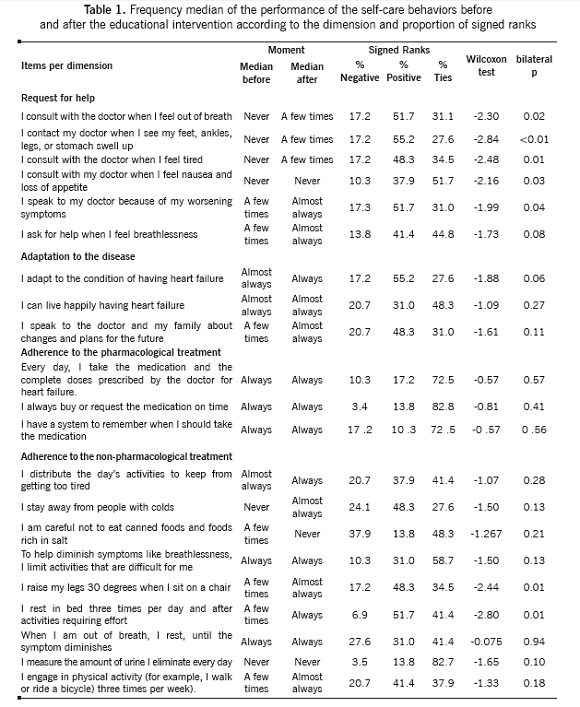
Analysis of repeated measures. In this study, 29 patients who were exposed to the educational intervention and who completed both of the self-care scale evaluations. The median value of the total score of the scale in the first evaluation was 40 points (interquartile rank: 34.5 - 43.0), while in the second evaluation it was 53 (interquartile rank: 45.0 and 60.0), said improvement of the score was statistically significant (z = -4.20, p < 0.001). The Wilcoxon signed-rank analysis showed that 86.2% of the patients (25 individuals) had positive changes that meant improvement in the scale score, 6.9% (2 individuals) presented negative changes, and an equal amount as the prior tied their score.
Table 1 shows the median values of the evaluation before and after the educational intervention and the proportion of positive, negative, and tied ranks of the items in the self-care scale. For the dimension of request for help, it may be noted that in five of the six items this difference is significant, with change in the frequency from never to a few times, in one of every two participants in the items having to do with consulting a physician when 'I feel out of breath', 'I see that my feet, ankles, legs, or stomach are swollen', and 'I feel tired'. The item 'I consult with my doctor when I feel nausea and loss of appetite' had a high proportion of ties, that is, no change was obtained, with the median value of never before and after intervention.
In the dimension adaptation to the disease, comprised of three items, it was found that, although without reaching statistical significance, positive changes were obtained in half of the individuals: in 'I adapt to the condition of having HF' (from almost always to always) and in 'I talk to the doctor and my family about changes and plans for the future' (from a few times to almost always); while in the item 'I can live happily having HF' half of the participants did not change frequency of the behavior, which was almost always.
The three items of the dimension adherence to the pharmacological treatment ('Every day, I take the medication prescribed by the doctor for HF', 'I buy or request the medication on time', and 'I have a system to remember when I should take the medication') had a median in the frequency of always in the self-care behaviors, in both the initial and final measurements.
In the dimension adherence to the non-pharmacological treatment, the items 'to help diminish symptoms like breathlessness, I limit difficult activities' and 'when I am out of breath, I rest until the symptom diminishes' did not change in frequency of performance, with always before and after the intervention. In this dimension only two items had positive changes with statistical significance in the frequency of self-care behaviors during the pre- and post-intervention evaluations: 'I raise my legs 30 degrees when I sit on a chair' (from never to almost always) and 'I rest in bed three times per day after activities requiring effort' (from never to always).
Although without statistically significant difference, improvement was also made in the frequency of the behaviors 'I distribute the day's activities to keep from getting too tired', 'I keep away from people with colds', and 'I engage in physical activity three to four times per week'. Two behaviors in this dimension deserve attention: the first has to do with reducing the intake of foods rich in salt in which a regression was noted in the median frequency from a few times to never, and the second in measuring on a daily basis the amount of urine eliminated, behavior in which almost nine of every ten participants did not change, with the median frequency of never before and after intervention.
DISCUSSION
This study, which evaluated the effectiveness of a nursing educational program to improve the self-care of patients with HF, found that participants increased the frequency of their behaviors from the first to the second evaluation with the educational intervention, which agrees with that reported in other similar studies.3,12
Regarding the self-care dimensions posed by the HFSCBS, for the Request for help similar results were found to those described by Artinian et al.,15 in which the self-care behaviors that improved most are those related to seeking medical help upon the evidence of symptoms and signs of HF decompensation; with this behavior being one of the most important goals in self-care educational programs.17 Another aspect related to requesting help is associated to recognizing the symptoms and the need for consultation before the symptoms worsen;18 these topics are aspects that are frequently dealt with in educational programs and those in which the patients and their caretakers pay greater attention to chest pain and to the sense of breathlessness; perceived by patients as evident risk of dying and for which they frequently consult.19
Among the most important strategies that allow patients to request help, there are the mechanisms of psychological adaptation to stress learnt during changes in their health status;20 however, Buetow21 states that healthcare professionals describe that patients with HF also use mental strategies like evasion, rejection, negation, and forgetfulness to encounter the disease; through these, they seek for hope to construct a positive life amid adversity, which can lead to suppression of angst upon learning of the diagnosis to negation of the reality of knowing they have HF.18
In the dimension of adaptation to the disease, positive changes were found of patients for their new condition. Some studies have concluded that patients with HF have seen their diagnosis as a positive experience22, given that it has helped them to reassess their existence23 and carry out plans in changing their life styles, which helps them to live with the disease;24 during this study, the participants manifested during the group meetings and home visits that they felt happier than before the disease. Another important situation related to this dimension is that patients with HF find it easier to follow the treatment and live with the symptoms if they have adapted to the disease.25
In adherence to the pharmacological treatment, during our investigation a good frequency was found of self-care behaviors of the participants during measurements before and after the educational intervention. Several studies state that because the pharmacological treatment in patients with HF is complex and for life, changes in behaviors related to said treatment are indispensable to reduce complications and deaths.26-30 It has been found that support from family and friends plays a fundamental role in pharmacological adherence, given that frequently these individuals share the responsibility of caretakers, a fact also observed in this investigation.26
During this study, in the dimension adherence to the non-pharmacological treatment, improvement was obtained in several self-care behaviors to diminish symptoms like sensation of breathlessness, edema, and fatigue; by planning their daily activities better to satisfy basic and leisure necessities; raising their legs when seated and resting in bed three times per day. As in the study by González et al.,31 our research found that one of the hardest behaviors to improve was the decrease of salt intake, which has been related to the patient's inadequate knowledge on managing this behavior,32,33, the cultural association the patient makes of salt with good flavor of food and with the interference of monitoring this type of diet with the patient's socialization needs, manifested as a conflict when other members of the family consume foods high in sodium;34 other studies have proposed that educational programs on the issue of restricting sodium intake35,36 should include, besides the patients, their family and close friends, as well as the food production industry.
It was also noted in this study that patients improved in the behavior of staying away from people with colds, which is indispensable to reduce the risk of respiratory infection that could be a cause of cardiac decompensation.36,37 Another important behavior improving in our study after the educational intervention was engagement in prescribed physical activity. Patients who did not manage to improve this behavior adduce to motives like the loneliness in which they live, conditions of insecurity where they live, lack of recreational centers for adults, and steep conditions of the neighborhoods where they have their homes; this is related to what is also posed by Artinian et al.,15 pointing out that the social conditions of the patients influence on how they carry out self-care activities.
The self-care behavior that did not obtain changes during the initial and final evaluations was that of the daily measurements of the amount of urine eliminated; during the home visits and the telenursing sessions, researchers found that patients do not measure their urine, given that they find no relationship between this practice and HF, they have no knowledge of how to measure their urine, their treating physician did not prescribe it, and they do not have equipment to perform this measurement task. However, this behavior is essential inasmuch as it relates to heart and kidney functions, the effect of diuretics, and control of liquid intake; hence, control of liquids through self-monitoring is fundamental to control complications in HF,38 which is why healthcare institutions must consider this aspect and include it in healthcare programs for these patients.
Bearing in mind that educational programs in nursing not only seek to improve awareness, but also the behaviors influencing upon the disease,39,40 the patients attending these programs perceive that changes in the behavior bear a beneficial impact on their health and will be more receptive to performing them.41,42 We cannot ignore the effect these programs have on improving physiological patterns (stabilization of blood volume, ejection fraction, kidney care) and the patient's physical and emotional capacities.43
Aware of the physical and emotional needs of patients with HF and of their families, along with the complexity of treating the disease and the social shortcomings and lack of access to healthcare services; it is a challenge for the nursing professional to promote educational programs with pedagogical strategies and inter-sector resources that manage to shed a glimpse of hope for individuals with HF against the possibilities of better quality of life even with the disease, by committing to care for themselves and to seek aid when they are incapable of self care.
Conclusion. The results of this research suggest that the nursing educational intervention conducted in our study had beneficial effects on most of the self-care behaviors assessed in individuals with HF. The educational intervention should be reinforced in the aspects where improvement was not noted.
Limitations of the study. Because the study simultaneously evaluated several educational strategies within the same intervention, it is not possible to indicate which was the most efficient, which makes it necessary to carry out further research to compare groups of patients with distinct strategies.
Another limitation is that, although the questionnaire to gather information was self-filled, some patients needed help from research aides to complete the evaluation, which could influence on possible information bias. Furthermore, the data gathered are the expression of the perception patients have of their own actions, which could be against their actual behaviors. It is suggested that in other investigations along the same line, information on bio-indicators should be completed, so that these can be related to the self-reported behaviors.
Acknowledgments: We thank our patients and their families for having shared their care experiences with us.
REFERENCES
1. Albert N. Evidence-based nursing care for patients with heart failure. AACN Adv Crit Care. 2006;17(2):170-83. [ Links ]
2. Achury D. Adherencia al tratamiento en el paciente con falla cardiaca. In: Rincón F, Díaz E, editors. Enfermería cardiovascular. Bogotá: Sociedad Colombiana de Cardiología; 2008. p. 342-68. [ Links ]
3. Scott L, Setter-Kliner K, Britton A. The effects of nursing interventions to enhance mental health and quality of life among individuals with heart failure. Appl Nurs Res. 2004;17(4):248-56. [ Links ]
4. Orem DE, Taylor SG, McLaughlin K, editors. Nursing: Concepts of Practice. St Louis, MO: Mosby; 2001. [ Links ]
5. Renpenning K, Taylor S. Self-care t theory of nursing: Selected Papers of Dorothea Orem. New York: Springer Pub Co; 2003. [ Links ]
6. Deaton C. Outcome measurement. J Cardiovasc Nurs. 2000;14(1):116-8. [ Links ]
7. Jiang HE, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton P. Risk factors for congestive heart failure in US men and women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med. 2001;161(7):996-1002. [ Links ]
8. Evangelista L, Doering L, Dracup K, Hamilton M. Compliance behaviors of elderly patients with advanced heart failure. J Cardiovasc Nurs. 2003;18(3):197-206. [ Links ]
9. Gheorghiade M, Zannad F. Modern management of acute heart failure syndrome. Eur Heart J. 2005;7(suppl B:):B7. [ Links ]
10. Chui M, Deer MBS, Tu W, Oury S, Brater D, Murray M. Association between adherence to diuretic therapy and health care utilization in patients with heart failure. Pharmacother. 2003;23(3):326-32. [ Links ]
11. Benatar D, Bondmass M, Ghitelman J, Avitall B. Outcomes of chronic heart failure. Arch Intern Med. 2003;163(3):347-52. [ Links ]
12. Baker DW, Asch SM, Keesey JW, Brown JA, Chan KS, Joyce G, et al. Differences in education, knowledge, self-management activities, and health outcomes for patients with heart failure cared for under the chronic disease model: the improving chronic illness care evaluation. J Card Fail. 2005;11(6):405-13. [ Links ]
13. Blue L, Lang E, McMurray J. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ. 2001;323(7315):715-8. [ Links ]
14. McAlister F, S. S, Ferrua S, 2004 MJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission. A systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810-9. [ Links ]
15. Artinian N, Morris M, Sloan M, Lange P. Self-care behaviors among patients with heart failure. Issues in Cardiovascular Nursing. Heart Lung. 2002;31(3):161-72. [ Links ]
16. Arredondo-Holguin E, Rodríguez-Gázquez M. Validez y confiabilidad de una escala de valoración de comportamientos de autocuidado en personas con falla cardiaca. Aquichan. 2012;12(1):23-31 [ Links ]
17. Jovicic A, Holroyd-Leduc J, Straus S. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. [ Links ]
18. Leslie WS, Urie A, Hooper J, Morrison CE. Delay in calling for help during myocardial infarction: reasons for the delay and subsequent pattern of accessing care. Heart. 2000;84(2):137-41. [ Links ]
19. Penny WJ. Patient delay in calling for help: the weakest link in the chain of survival? Heart. 20011;85(2):121-2. [ Links ]
20. An K, De Jong M, Riegel B, McKinley S, Garvin B. A cross-sectional examination of changes in anxiety early after acute myocardial infarction Heart Lung. 2004;33(2):75-82. [ Links ]
21. Buetow S, Goodyear F, Coster G. Coping strategies in the self-management of chronic hearth failure. Fam Pract. 2001;18:117-22. [ Links ]
22. Mahoney JS. An ethnographic approach to understanding the illness experiences of patients with congestive heart failure and their family members. Heart Lung. 2001;30(6):429-36. [ Links ]
23. Pattenden JF, Roberts H, Lewin RJ. Living with heart failure; patient and carer perspectives. Eur J Cardiovasc Nurs. 2007;6(4):273-9. [ Links ]
24. Costello JA, Boblin S. What is the experience of men and women with congestive heart failure? Can J Cardiovasc Nurs. 2004;14(3):9-20. [ Links ]
25. Welstand J, Carson A, Rutherford PJ. Living with heart failure: an integrative review. Int Nurs Stud. 2009;46(10):1374-85. [ Links ]
26. Strömberg A, Mårtensson J, Fridlund B, Levin LA, Karlsson JE. Dahlström, U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective randomised trial. Eur Heart J. 2003;24:1014-23. [ Links ]
27. González B, Lupón J, Herreros J, Urrutia A, Altimir S, Coll R, et al. Patient's education by nurse: what we really do achieve? Eur J Cardiovasc Nurs. 2005;4(2):107-11. [ Links ]
28. Clark AP, Stuifbergen A, Gottlieb NH, Voelmeck W, Darby D, Delville C. Health promotion in heart failure--a paradigm shift. Holist Nurs Pract. 2006;20(2):73-9. [ Links ]
29. Barrera L, Galvis C, Moreno M, Pinto N, Pinzón M, Romero E, et al. La habilidad de cuidado de los cuidadores familiares de personas con enfermedad crónica. Un estudio comparativo de tres unidades académicas de enfermería. Invest Educ Enferm. 2006;24(1):36-46. [ Links ]
30. Hearth Failure Society of America. Comprehensive heart failure practice guideline. J Card Failure. 2010;16:e1-e194. [ Links ]
31. González B, Lupón J, Herreros J, Urrutia A, Altimir S, Coll R, et al. Patient's education by nurse: what we really do achieve? Eur J Cardiovasc Nurs 2005;4(2):107-11. [ Links ]
32. Martje HL, Van der Wal M, Jaarsma T, Moser D, Veeger N, van Gilst W, et al. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006;27(4):434-40. [ Links ]
33. Colín E, Castillo L, Orea A, Montaño P, Dorantes J. Impacto de una dieta con restricción de sodio y líquidos sobre el estado clínico de pacientes con insuficiente cardiaca. Rev Chil Nutr. 2010;37(4):427-37. [ Links ]
34. Bentley B, De Jong MJ, Moser DK, Peden AR. Factors related to nonadherence to low sodium diet recommendations in heart failure patients. Eur J Cardiovasc Nurs. 2005;4(4):331-6. [ Links ]
35. Ajzan I. Attitudes, personality and behavior New York: Open University Press; 2005. [ Links ]
36. Achury D. Contexto clínico de la falla cardiaca. En: Adherencia al tratamiento en el paciente con falla cardiaca. Bogotá: Editorial Universidad Nacional; 2007. [ Links ]
37. Rich MW. Heart failure in the elderly: strategies to optimize outpatient control and reduce hospitalizations. Am J Geriatr Cardiol. 2003;12(1):19-24. [ Links ]
38. Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179-85. [ Links ]
39. Rankin S, Stallings K. Patient education, principles and practice. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2001. [ Links ]
40. Gattis W, Hasselblad V, Whellan D, O'Connor C. Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Arch Intern Med. 1999;159(16):1939-45. [ Links ]
41. Holst M, Willenheimer R, Martenson J, Lindholm M, Strömberg ATf-uos-cbaasseopwhfiphc. Telephone follow-up of self-care behaviour alter a single sesión education of patients with heart failure in primary health care. Eur J Cardiovasc Nurs. 2007;6(2):153-9. [ Links ]
42. López M, Rus C, Martínez MM, Cortez GA, Delgado M. Aplicación de un plan de cuidados de enfermería en un programa de insuficiencia cardiaca. Enferm Cardiol. 2007;14(41):25-32. [ Links ]
43. Whellan DJ, Gaulden L, Gattis WA, Granger B, Russell SD, Blazing MA, et al. The benefit of implementing a heart failure disease management program. Arch Intern Med. 2001;161(18):2223-8. [ Links ]