Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307On-line version ISSN 2216-0280
Invest. educ. enferm vol.30 no.2 Medellín July/Dec. 2012
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Puerperal women's satisfaction with their delivery
La satisfacción de las puérperas con su parto
A satisfação de puérperas com o seu parto
Ariane Garcia Cicuto1; Cíntia Rodrigues Leite Belisário2; Beatriz Barco Tavares3
1 RN. Professor, Faculdade de Medicina de São José do Rio Preto FAMERP, Brasil. email: ariane.cicuto@hotmail.com.
2 RN. FAMERP, Brasil.email: cintiafamerp@gmail.com.
3 RN, PHD. Professor, Nursing Department, FAMERP, Brasil. email: bbarco@famerp.br.
Receipt date: January 14th 2012. Approval date: March 23rd 2012.
Subventions: Bolsa de Iniciação Científica da FAMERP.
Conflicts of interest: none.
How to cite this article: Cicuto AG, Belisário CRL,Tavares BB. Puerperal women's satisfaction with their delivery. Invest Educ Enferm. 2012;30(2): 208-214.
ABSTRACT
Objective. To assess puerperal women's level of satisfaction with their delivery. Methodology. A descriptive study was developed at a teaching hospital in São José do Rio Preto (Brazil between July and December 2010. Participants were 200 puerperal women from the neonatal screening service, who completed the Delivery Experience and Satisfaction Questionnaire to measure their satisfaction level. Answer options for each question range between 1 and 10 (maximum satisfaction). Results. The puerperal women's mean age was 28 years; 96% had a partner; all women had participated in prenatal care; 82% were submitted to caesarean section. Satisfaction with pain management during labor ranged from 8.5 for caesarean section to 6 for normal birth. In comparison with the vaginal birth group, women subject to c-section showed greater satisfaction with postpartum pain intensity (8.7 versus 6.2) and less satisfaction with labor (6.0 versus 8.5) and delivery (7.1 versus 9.0). Conclusion. Without any difference per delivery type, women's satisfaction level with their delivery was high. Women who underwent caesarean section obtained higher satisfaction scores for postpartum pain management, while women who underwent vaginal birth manifested greater satisfaction with pain control during labor and delivery.
Key words: personal satisfaction; obstetrical nursing; parturition; obstetrics.
RESUMEN
Objetivo. Evaluar el nivel de satisfacción de las puérperas con sus partos. Metodología. Estudio descriptivo realizado en el hospital de enseñanza de São José do Rio Preto (Brasil), de juliodiciembre de 2010. Participaron 200 puérperas del servicio de tamizaje neonatal, que diligenciaron el instrumento Questionário de Experiência e Satisfação com o Parto para medir el nivel de satisfacción. Cada pregunta tiene opciones de respuesta entre 1 a 10 (máxima satisfacción). Resultados. El promedio de edad de las puérperas fue 28 años, el 96% tenía compañero, todas realizaron control prenatal, 82% fueron sometidas a cesárea. El nivel de satisfacción promedio fue de 9 en las mujeres con parto normal o por cesárea. La satisfacción con el manejo del dolor en el trabajo de parto fue de 8.5 para cesárea versus 6 en el parto normal. Comparadas con el grupo de parto vaginal, las cesariadas tuvieron una mayor satisfacción con la intensidad del dolor en el posparto (8.7 versus 6.2), y menor en el de trabajo de parto (6.0 versus 8.5) y parto (7.1 versus 9.0). Conclusión. Sin diferencia por tipo de parto, la satisfacción de las mujeres con su parto fue alta. Las cesariadas tuvieron mayor satisfacción con el manejo del dolor posparto, mientras que las de parto vaginal manifestaron mayor satisfacción en el control del dolor durante el trabajo de parto.
Palabras clave: satisfacción personal; enfermería obstétrica; parto; obstetricia.
RESUMO
Objetivo. Avaliar o nível de satisfação das puérperas com seus partos. Metodologia. Estudo descritivo realizado no hospital de ensino de São José do Rio Preto (Brasil), de julho-dezembro de 2010. Participaram 200 puérperas do serviço de seleção neonatal, que preencheram o instrumento Questionário de Experiência e Satisfação com ou Parto para medir o nível de satisfação, cada pergunta tem opções de resposta entre 1 a 10 (máxima satisfação). Resultados. A média de idade das puérperas foi 28 anos, o 96% tinha parceiro, todas realizaram controle pré-natal, 82% foram submetidas a cesárea. O nível de satisfação média foi de 9 nas mulheres com parto normal ou por cesárea. A satisfação com o manejo da dor no trabalho de parto foi de 8.5 para cesárea contra 6 no parto normal. Comparadas com o grupo de parto vaginal, as cesariadas tiveram uma maior satisfação com a intensidade da dor no pós-parto (8.7 contra 6.2), e menor no de trabalho de parto (6.0 contra 8.5) e parto (7.1 contra 9.0). Conclusão. Sem diferença por tipo de parto, a satisfação das mulheres com seu parto foi alta. As que realizaram cesárias tiveram maior satisfação com o manejo da dor pós-parto, enquanto as de parto vaginal manifestaram maior satisfação no controle da dor durante o trabalho de parto e parto.
Palavras chaves: satisfação pessoal; enfermagem obstétrica; parto; obstetrícia.
INTRODUCTION
To inhibit women's morbidity and mortality in the pregnancy-puerperal cycle, Brazilian and international entities determine humanized and high-quality prenatal, delivery and puerperal care, making women and their families feel more satisfied. Among attitudes, women's attitudes as the primary actors during delivery stands out, participating in choices regarding their care.1 Parturient women's active participation should be stimulated, providing orientations about their health condition, delivery types, risks and benefits, guaranteeing a safe and effective delivery, with a view to enhancing their autonomy and respecting the right to choose what the birth of their child will be like.2 Orientation also avoids possible future complains, that is, good communication between health professionals and women in the pregnancy-puerperal cycle is essential.3
The birth process demands a private, welcoming and comfortable environment that guarantees the parturient women's safety, with a view to reducing anxiety and fear, which can interfere in pain perceptions and, consequently, in the evolution of labor.4 The fear of labor pain isa factor that stimulates women to request a c-section. To minimize this pain, the use of analgesic during labor increases, to the detriment of several alternative techniques, predisposing to higher incidence levels of instrumental births and caesarean sections. In the United States, no single conduct exists either, as the availability of anesthesia differs from state to state and even among cities in the same state, highlighting rural areas as the most problematic regions.5,6 This type of care entails longer hospitalization and postpartum recovery times, raising care costs. In the Unified Health System (SUS), the cost of a caesarean section (c-section) ranges between R$ 647 and R$ 1 012, against R$ 445 to R$638 for normal births.7
In Brazil, caesarean sections represent 43%, one of the highest rates in the world. In the Southeast, this delivery type represents 52%, which is the highest rate; in the North, on the other hand, percentages are lower with 35%. According to World Health Organization recommendations, however, these surgeries should only take place when the natural procedure represents risks for the infant and/or the mother, which is the case in between 15 and 20% of births.8 round the world, more than half a million maternal deaths take place due to pregnancy, birth and puerperal complications. These deaths could be avoided through preventive measures, using appropriate technology.9
The choice of the delivery type is linked with complication risks and receives countless influences, ranging from economic to cultural issues, which need to be minimized. In regions with high incidence levels of caesarean sections, this is considered the ''ideal'' delivery, a consumption good many pregnant women desire. In 2008, in São José do Rio Preto, São Paulo, Brazil, researchers identified that 43% of pregnant adolescents and 41% of pregnant adult women would like to submit to a c-section. In another region of the country, on the other hand, 75% of the women were expecting normal birth.10,11 The woman's relation with the health team is an essential component of her satisfaction with the delivery type, as it arouses good maternal experiences regarding the delivery type and care. Hence, if a team professional attends the woman badly during her delivery, her dissatisfaction rate with the delivery type will be higher, i.e. it will be negatively affected. If the parturient woman's relation with the team is good, on the other hand, her satisfaction rate will increase.12
Based on this panorama and with a view to improving women's health care in this life phase, the aim of this study is to: assess puerperal women's level of satisfaction with their delivery.
METODOLOGY
This quantitative and retrospective study was developed at the pediatric outpatient clinic of a teaching hospital (HB) with a capacity of more than 700 beds, 63 of which for obstetric care. The outpatient clinic received about 300 newborn infants per month for the heel lance procedure, a test to detect phenylketonuria, congenital hypothyroidism, hemoglobinopathies and cystic fibrosis.
A convenience sample was obtained from the population, comprising 200 puerperal women who brought their child for Neonatal Screening, as described above, between July and December 2010. For data collection, an individual interview was held, using a specific instrument that includes the following parts: identification data (age, marital status, education, family income, occupation), obstetric data for current birth (prenatal, delivery, postpartum) and data about satisfaction with the childbirth experience. To assess the satisfaction level, a scale from 1 to 10 was used, related to the level of personal satisfaction, with 1 indicating the worst and 10 the best satisfaction level, based on an instrument Costa et al.13 developed in 2004, the Delivery Experience and Satisfaction Questionnaire (QESP). A pilot test was performed to adapt and validate the proposed instrument.
The collected data were transcribed to a worksheet elaborated in Excel 2007, grouped according to specific characteristics. The data were analyzed and presented descriptively and in tables with absolute figures and percentages for the sake of a better visualization. To analyze the variables, a significance level of ?=0.05 was observed, but the analysis showed no statistical differences in satisfaction levels. Approval for the research project was obtained from the Research Ethics Committee at FAMERP, in compliance with National Health Council Resolution 196/96, under protocol No. 2786/2010.
RESULTS
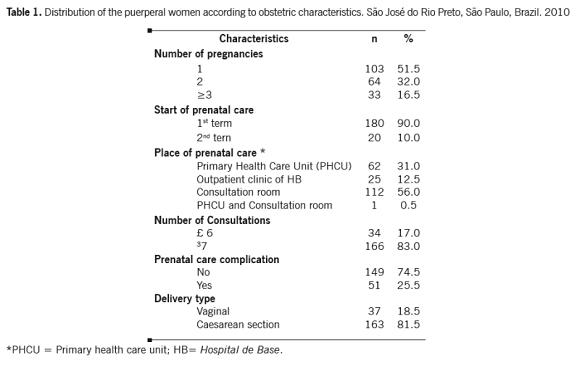
The puerperal women's mean age was 27.6 years, 50.0% were between 20 and 29 years old and 95.5% lived with a partner. As for the education level, 72.5% of the women had more than 11 years of study; 57.0% had a paid job, i.e. they contributed to the family income; 64.0% lived in their own home. Sixteen percent of the women survived on one minimum wage (MW), 46.0% on a family income of two to three MW, 24.5% four to five MW and 13.5% more than 5 MW. Table 1 displays the obstetric characteristics of the current birth. It is noteworthy that 100% of the women participated in antenatal care, 90% started in the first term, 83% took part in seven or more consultations, but 66% did not participate in educative groups for pregnant women. Nevertheless, 77.5% declared they had received some information about the delivery types. The Unified Health System -SUS- funded 42.5% of these deliveries, and the remaining 57.5% were self-funded, either through a health insurance plan or privately.
Out of 117 women who expected a c-section, 114 (97.4%) underwent this procedure. Out of 82 women who wanted vaginal birth, however, this only happened in 34 (41.4%) cases. This difference is statistically significant (X2 with Yates' correction = 45.6, p<0.001).
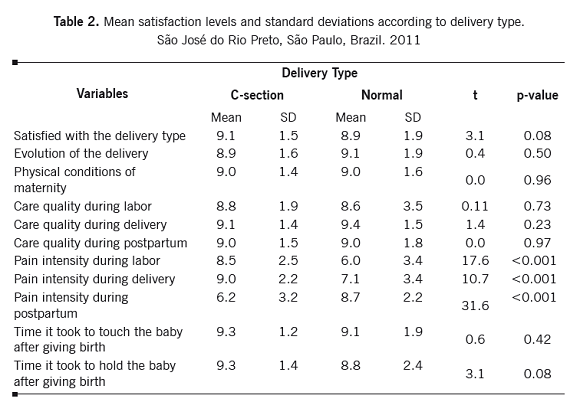
It is observed in Table 2 that the mean satisfaction level of women who underwent c-section and vaginal birth was the same (9.1 versus 8.9). Some statistically significant differences are found though. In comparison with the vaginal birth group, the c-section group showed higher satisfaction levels regarding postpartum pain intensity (8.7 versus 6.2) and lower satisfaction levels concerning labor (6.0 versus 8.5) and delivery (7.1 versus 9.0).
DISCUSSION
All women participated in prenatal care, but less than half participated in educative groups for pregnant women. In the same sense, researchers describe that a lack of information creates insecurity to have a normal birth and makes society define caesarean section as a low-risk procedure.14 This also confirms expectations regarding the delivery type and the actual delivery, entailing high c-section rates. Women's insufficient preparation for labor and delivery causes unrealistic expectations, mainly related to pain, leaving care decisions up to the health professionals. Adequate prenatal care aims to minimize this expectation, preparing them for what can happen and thus limiting this gap between expectation and experience.15
In addition, maternal morbidity and mortality rates are higher among women submitted to caesarean section, women with repeated c-sections and those of advanced maternal age. It is important to advise pregnant women on the risks and benefits of each delivery type though, so that they choose the delivery type consciously, and for health professionals to respect their autonomy and decision, always discussing with the women what procedures will be performed during the birth process.14
It is noteworthy that satisfaction levels with the delivery type were the same between the groups. Studies demonstrate that this satisfaction rate receives different influences, from variables like the evolution of the delivery, the maternity's physical conditions and labor and delivery care, which were similar in our study.16 Higher satisfaction levels are described among women after normal delivery though.16
The higher satisfaction rate among women who underwent normal delivery may be related to the woman's active participation in the birth process, the encouragement of vaginal delivery, breastfeeding in the immediate postpartum period, and the stay at the rooming-in unit, i.e. mother and infant stay together from birth until hospital discharge. These promote affective bonds between mother and child since the first hours of life and, consequently, greater satisfaction with the delivery type and care received.13,17
Satisfaction with pain before the delivery was higher among women who underwent caesarean section, as labor did not even start for many of them. Studies have described that the use of non-pharmacological strategies relieves pain during labor, mainly in the active phase, and health professionals need to heed these practices with a view to using appropriate technology in care delivery, enhancing the parturient women's satisfaction.18 The women describe labor pain as a negative but necessary factor to experience this unique moment of a child's birth, which is compensated for by the happiness of holding the child in their arms, and facilitated by the presence of a companion they trust, enhancing their relaxation.19-21
With regard to postpartum pain assessment, women submitted to c-section reported higher pain intensity, lowering their satisfaction level in comparison with women with underwent normal birth. In line with this result, researchers found higher morbidity levels among women who gave birth through caesarean section, and the pain was characterized as very intense.22 Concerning care at the rooming-in unit, the puerperal women after normal birth felt more satisfied.22
Conclusion. Independently of the delivery type, women in this study showed the same satisfaction level. Differences were found in labor, delivery and postpartum pain intensity, with higher satisfaction levels during labor and lower rates during the postpartum, as opposed to women after vaginal birth. Care delivery to pregnant and parturient women and to mothers and infants needs to further conditions for women to be fully active, instead of moments of unnecessary interventions, enhancing humanized care. Thus, the delivery type is chosen consciously, increasing satisfaction levels.
REFERENCES
1. Serruya SJ, Cecatti JG, Lago T di G. O Programa de Humanização no Pré-natal e Nascimento do Ministério da Saúde no Brasil: resultados iniciais. Cad Saúde Pública. 2004;20(5):1281-9. [ Links ]
2. Barcellos LG, Souza AOR, Machado CAF. Cesariana: uma visão bioética. Rev Bioética. 2009;17(3):497-510. [ Links ]
3. Uzcátegui UO, Cabrera C. Aspectos bioéticos de la cesárea y consentimiento informado. Rev Obstet Ginecol Venez. 2010;70(1):47-52. [ Links ]
4. Ministério da Saúde. O modelo de atenção obstétrica no setor de Saúde Suplementar no Brasil: cenários e perspectivas [Internet]. Rio de Janeiro: Ministério da Saúde; 2008 [cited 2010 January 16]. Available in: http://bvsms.saude.gov.br/bvs/publicacoes/livro_parto_web.pdf [ Links ]
5. Velasco LA, Barroso MTS, Segura MH, Martínez ER, Perales S, González-Acosta V, et al. Influencia de la analgesia epidural en el parto [Internet]. [cited 2010 April 16]. Available in: http://dialnet.unirioja.es/servlet/articulo?codigo=3147815 [ Links ]
6. Birnbach DJ, Bucklin BA, Dexter F. Impact of anesthesiologists on the incidence of vaginal birth after cesarean in the United States: role of anesthesia availability, productivity, guidelines, and patient safety. Semin Perinatol. 2010;34(5):318-24. [ Links ]
7. Ministério da Saúde. Saúde incentiva parto normal [Internet]. Brasília: Ministério da Saúde [cited 2010 March 29]. Available in: http://portal.saude.gov.br/portal/saude/visualizar_texto.cfm?idtxt=33908 [ Links ]
8. Ministério da Saúde. Campanha incentivo ao parto normal [Internet]. Brasília: Ministério da Saúde [cited 2010 January 20]. Available in: http://portal.saude.gov.br/portal/aplicacoes/campanhas_publicitarias/campanha_detalhes.cfm?co_seq_campanha=1765 [ Links ]
9. Faneite P, Rivas M. Mortalidad materna: tragedia prevenible? Hemos avanzado? Rev Obstet Ginecol Venez. 2010;70(1):24-30. [ Links ]
10. Bruzadeli, DS, Tavares BB. Expectativa quanto ao parto e conhecimento do motivo da cesárea: entre puérperas adolescentes e adultas. Rev Eletr Enf. 2010;12(1):150-7. [ Links ]
11. Melchiori LE, Maia ACB, Bredariolli RN, Hory RI. Preferência de gestantes pelo parto normal ou cesariano. Interação Psicol. 2009;13(1):13-23. [ Links ]
12. Domingues RMSM, Santos EM, Leal MC. Aspectos da satisfação das mulheres com a assistência ao parto: contribuição para o debate. Cad Saúde Pública. 2010;20(Suppl 1):S52-S62. [ Links ]
13. Costa R, Figueiredo B, Pacheco A, Marques A, Pais A. Questionário de experiência e satisfação com o parto (QESP). Psicol Saúde Doenças. 2004;5(2):159-87. [ Links ]
14. Salim R, Shalev E. Health implications resulting from the timing of elective cesarean delivery. Reprod Biol Endocrinol. 2010;8:68. [ Links ]
15. Lally JE, Murtagh MJ, Macphail S,Thomson R. More in hope than expectation: a systematic review of women's expectations and experience of pain relief in labour. BMC Med. 2008;6: 7:7. [ Links ]
16. Silva, AC de S. Vivências da maternidade:expectativas e satisfação das mães no parto. [Dissertation] Coimbra: Faculdade de Psicologia e de Ciências da Educação, Universidade de Coimbra; 2010. [ Links ]
17. Davim RMB, Torres GV, Dantas JC. Efetividade de estratégias não farmacológicas no alívio da dor de parturientes no trabalho de parto. Rev Esc Enferm USP. 2009;4(2):438-45. [ Links ]
18. Lopes CV, Meincke SMK, Carraro TE, Soares MC, Reis SP, Heck RM. Experiências vivenciadas pela mulher no momento do parto e nascimento de seu filho. Cogitare Enferm. 2009;14(3):484-90. [ Links ]
19. Oliveira ASS, Rodrigues DP, Guedes MVC, Felipe GF. Percepção de mulheres sobre a vivência do trabalho de parto e parto. Rev Rene. 2010;11(Esp):32-41. [ Links ]
20. Oliveira ASS, Rodrigues DP, Guedes MVC, Felipe GF, Galiza FT, Monteiro LC. O acompanhante no momento do trabalho de parto e parto: percepção de puérperas. Cogitare Enferm. 2011;16(2):247-53. [ Links ]
21. Cardoso PO, Alberti LR, Petroianu A. Morbidade neonatal e maternas relacionada ao tipo de parto. Ciênc Saúde Coletiva. 2010;15(2):427-35 . [ Links ]
22. Odinino NG, Guirardello EB. Satisfação da puérpera com os cuidados de enfermagem recebidos em um alojamento conjunto. Texto Contexto Enferm. 2010;19(4):682-90. [ Links ]