Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307On-line version ISSN 2216-0280
Invest. educ. enferm vol.30 no.2 Medellín July/Dec. 2012
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Knowledge of the Andalusian legislation on dignified death and perception on the formation in attention to terminally ill patients of health sciences students at Universidad de Granada, Spain
Conocimiento sobre la ley andaluza de muerte digna y percepción sobre la formación en la atención a enfermos terminales del alumnado de ciencias de la salud de la Universidad de Granada, España
Conhecimento sobre a lei andaluza de morte digna e percepção sobre a formação no atendimento a enfermos terminais do corpo discente de ciências da saúde da Universidade de Granada, Espanha
Amalia María Morales-Martín1; Jacqueline Schmidt-Riovalle2; Inmaculada García-García3
1 RN, M.Sc. Andalusian Health Service, Spain. email: morales.amalia@gmail.com.
2 RN, PH.D. Professor, Faculty of Health Sciences, Universidad de Granada, Spain. email: jschmidt@ugr.es.
3 RN, PH.D. Professor, Faculty of Health Sciences, Universidad de Granada, Spain. email: igarcia@ugr.es.
Receipt date: August 4th 2011 Approval date: December 13rd 2011.
Subventions: none.
Conflicts of interest: none.
How to cite this article: Morales-Martín AM, Schmidt-Riovalle J, García-García I. Knowledge of the Andalusian legislation on dignified death and perception on the formation in attention to terminally ill patients of health sciences students at Universidad de Granada, Spain. Invest Educ Enferm. 2012;30(2): 215-223.
ABSTRACT
Objective. To determine the knowledge of the Andalusian ''Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process'' and perception of the formation on attention to terminally ill patients by students of health sciences at Universidad de Granada, Spain. Methodology. Cross-sectional descriptive study, conducted in 2010, with the participation of 572 students from the Nursing, Physical Therapy, and Occupational Therapy careers of the Faculty of Health Sciences at Universidad de Granada. A questionnaire including 19 variables was used. The data gathered was analyzed with the SPSS 15.0 program. Results. Half of the participants know of this Legislation. A total of 86.7% of the students did not know that the limitation of the therapeutic effort is a legal practice throughout Spain; 97.9% did not know either that the limitation of vital support measures is a legal practice. 64.2% of the students feel capable of addressing this issue with terminally ill patients and their families. 83.3% of those surveyed report not having sufficient knowledge to provide information about the ''Living testament''. Nursing students have greater knowledge of the Legislation studied; likewise, those who took the Palliative Care course obtained better results than students who did not. Conclusion. Students do not have adequate knowledge of the Andalusian legislation of dignified death. Although the participants do not feel prepared academically to deal with these types of patients, they do consider themselves capable of doing so.
Key words: palliative care; right to die; students, health occupations; legislation as topic.
RESUMEN
Objetivo. Determinar el conocimiento sobre ''Ley de Derechos y Garantías de la Dignidad de la Persona en el Proceso de la Muerte'' y percepción sobre la formación en la atención a enfermos terminales del alumnado de ciencias de la salud de la Universidad de Granada, España. Metodología. Estudio descriptivo de tipo transversal, realizado en 2010, en el que participaron 572 alumnos de las titulaciones de Enfermería, Fisioterapia y Terapia Ocupacional de la Facultad de Ciencias de la Salud de la Universidad de Granada. Se empleó un cuestionario que incluía 19 variables. Los datos recogidos se analizaron con el programa SPSS 15.0. Resultados. La mitad de los participantes tienen conocimiento de esta Ley. 86.7% del alumnado no sabía que la limitación del esfuerzo terapéutico es una práctica legal en toda España. 97.9% tampoco sabía que la limitación de medidas de soporte vital es una práctica legal. 64.2% de los estudiantes se siente capacitado para tratar este tema con el enfermo terminal y su familia. 83.3% de los encuestados reporta no tener el suficiente conocimiento para dar información sobre el ''Testamento Vital''. Los estudiantes de Enfermería tienen mayor conocimiento sobre la Ley en estudio; asimismo, aquellos que cursaron Cuidados Paliativos obtuvieron mejores resultados que quienes no lo hicieron. Conclusión. Gran parte de los alumnos no tiene un conocimiento adecuado de la Ley andaluza de muerte digna. Aunque los participantes no se sientan preparados académicamente para tratar con este tipo de pacientes, sí se consideran capaces para hacerlo desde la práctica.
Palabras clave: cuidados paliativos; derecho a morir; estudiantes del área de la salud; legislación como asunto.
RESUMO
Objetivo. Determinar o conhecimento sobre a lei andaluza da ''Lei de Direitos e Garantias da Dignidade da Pessoa no Processo da Morte'' e percepção sobre a formação no atendimento a enfermos terminais do corpo discente de ciências da saúde da Universidade de Granada, Espanha. Metodologia. Estudo descritivo de tipo transversal, realizado em 2010, no que participaram 572 alunos das titulações de Enfermaria, Fisioterapia e Terapia Ocupacional da Faculdade de Ciências da Saúde da Universidade de Granada. Empregou-se um questionário que incluía 19 variáveis. Os dados recolhidos se analisaram com o programa SPSS 15.0. Resultados. A metade dos participantes têm conhecimento desta Lei. 86.7% do corpo discente não sabia que a limitação do esforço terapêutico é uma prática legal em toda Espanha. 97.9% também não soube que a limitação de medidas de suporte vital é uma prática legal. 64.2% dos estudantes se sentem capacitados para tratar este tema com o enfermo terminal e sua família. 83.3% dos interrogados reportam não ter o suficiente conhecimento para dar informação sobre o ''Testamento Vital''. Os estudantes de Enfermagem têm maior conhecimento sobre a Lei em estudo; assim mesmo, aqueles que cursaram Cuidados Paliativos obtiveram melhores resultados que o corpo discente que não o fez. Conclusão. Nos alunos não é adequado o conhecimento da Lei andaluza de morte digna. Ainda que os participantes não se sentam preparados academicamente para tratar com este tipo de pacientes sim que se consideram capazes para fazê-lo.
Palavras chaves: cuidados paliativos; direito a morrer; estudantes de ciências da saúde; legislação como assunto.
INTRODUCTION
Legislation on Rights and Guarantees of the Dignity of Individuals during the Death Process,1 stems from the patients' right to decide during the process of their death. This Legislation also regulates the actions of healthcare personnel regarding limitations of therapeutic efforts and therapeutic obstinacy. This permits patients to select their treatment during the final stage of their lives. In the West, death is an inevitable fact that is still difficult to treat. Modern hospitals are not the appropriate scenario to let the person go; rather, they represent the theater of the struggle for life, where physicians determine when and how it is convenient to let the patient go through the interruption healthcare.2-4
In a democratic society in which respect for the individual's freedom and autonomy must be maintained during the illness and fully reach the death process,1 change of the healthcare offered during the death process should be facilitated, relegating the ethical principle of beneficence for that of the patient's autonomy. Although, currently, the relationship of the healthcare team with the infirmed individuals and their family members is more open and respectful of their dignity,5 most efforts for attention continue concentrating on improving the quality of life and not the quality of death. It is because of the aforementioned that many societies continue leaving no option for palliative care. An investigation conducted in 40 countries around the world found that too many people, including countries with excellent healthcare systems, endure poor quality of death, even when such arrives naturally.6 The authors of this study classify the nations analyzed in relation to the Quality of Death Index, which integrates different criteria (provision of palliative care, access to analgesic treatments, public policies and funds for the terminally ill, individual and community perceptions of death, among others). In this index, the United Kingdom, Australia, New Zealand, Ireland, and Belgium have been classified among the first five best places; while Mexico, China, Brazil, Uganda, and India hold the last five places.
The attitude of the European Council has been to protect the dignity of all human beings and the rights emanating from such. In its Resolution 613 of 1976,7 the Council declared its conviction that the terminally ill mainly want to die in peace and dignity, surrounded by their families and friends, if possible. It also considers that prolonging life should not be the exclusive purpose of the medical practice, but that it should also be concerned with relief of suffering.7
During June 1999, the Parliamentary Assembly of the European Council approved Recommendation 1418, which suggests to the Member States to act to protect citizens during the final stage of life. The text defends palliative care as a subjective right that should be provided during healthcare assistance. But it underscores that the desire to die did not generate a legal right of the patient or a judicial justification for a third party to practice euthanasia.8 In 2005, a proposal introduced to the European Council to legalize euthanasia in certain cases was rejected. It was a resolution project that set out to refine the posture opposed to euthanasia adopted in 1999. This project, according to the author of said proposal, did not declare itself in favor of admitting euthanasia and cooperation to suicide, but suggested diverse measures to guarantee the rights of the terminally ill.9,10 European nations have adopted different measures to guarantee these rights.11 The, previously mentioned, Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process,1 regulates the exercise of the rights of individuals during their death process, duties of healthcare personnel attending these patients, as well as the guarantees healthcare institutions are obligated to provide with respect to this process. For this, its purpose will be to protect the dignity of individuals during their death process, ensure the autonomy of patients, and respect their will in said process. Additionally, it includes the citizen's will previously manifested through the living testament.
This new Andalusian legislation is pioneer in Spain in regulating the rights of patients and duties of healthcare professionals, both in public and private centers, and it has been a reference in other Spanish communities. The Foral Legislation 8/2011, of 24 March, on Rights and Guarantees of the Dignity of the Individual during the Death Process of Navarra,12 and the project of Legislation regulating the Rights of Individuals upon the Final Process of Life13 (whose draft has already been published), are examples of such.
The exercise of the right to dying with dignity has special importance in the multicultural and diverse Andalusian society in which distinct beliefs, values, y preferences coexist regarding death and how to confront it. This right is to be respected and guaranteed, as long as it does not violate that established in the legal order. The General Health Legislation 14/1986 of 24 April,14 along with Legislation 2/1998,15 of 15 June from Andalucía Health, have recognized and regulated the right of patients to individual autonomy with respect to their health status. This right was specifically regulated in Legislation 41/2002, of 14 November, called Basic Regulatory Legislation of the Patient's Autonomy and of the Rights and Obligations on Issues of Clinical Information and Documentation16. However, increasingly, complex situations emerge related to the capacity of individuals to decide about their own lives and on the application or not of certain treatments. This has motivated broad social debate, and the convenience of specifically approaching the regulation of the rights of individuals facing the death process.
The importance of palliative care has increased in recent years parallel to the concept of health, where medicine is no longer limited to merely curing the disease, but it is also involved in improving the quality of life and diminishing human suffering.
In Andalucía, the term ''palliative care'' did not appear legally until the 2007 Organic Law reforming the Statute of Autonomy for Andalucía,17 posterior to Legislation 5/2003 on Declaration of Anticipated Vital Will,18 which regulated the rights of individuals to decide on the health actions to which they could be subjected in the future.
In Spain, the curriculum in Nursing Schools has begun to include palliative care among its subject matter. The degree in Physical Therapy had already announced in its White Book (Libro Blanco)19 that one of its objectives would be to contribute to maintaining health, wellbeing, and quality of life of individuals, families, and the community. In Occupational Therapy the main core of its assignments are daily life activities to favor the autonomy of individuals.20 While it is true that these two last careers still do not include palliative care in their curriculum, it should be highlighted that both promote self-formation and knowledge of this subject, although the area of nursing began learning this beforehand.
This study sought to determine the knowledge of the Andalusian ''Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process'' and the perception of the formation on attention to terminally ill patients by health sciences students at Universidad de Granada, Spain.
METODOLOGY
This was a descriptive and cross-sectional study conducted with university students enrolled in the careers of Nursing, Physical Therapy, and Occupational Therapy of the Faculty of Health Sciences at Universidad de Granada in Spain. Data collection was carried out during June and July 2010. Attending, non-matriculated students were excluded, as were those who were only taking some courses as free configuration.
To gather the information, the students were concentrated in their classes. After explaining the purpose of the study, the students who voluntarily accepted to participate filled out a questionnaire with a maximum 30-minute time limit. Of the 943 students enrolled 572 were surveyed, corresponding to 61% coverage. The information collection instrument also included the variables of sex, age, career and course enrolled, 15 questions regarding all the legal issues contemplated by the Legislation, opinions about the professional exercise, and experience with patients during end-of-life processes. Once the instrument was elaborated, it was submitted to evaluation by three professors (two from Law and one from Ethics), who gave their expert opinion with respect to the clarity of the questions and if all the legal cases contemplated by the legislation were gathered. Their observations were incorporated in the final version of the 15-question survey, which was divided into three groups: 1st Evaluation of knowledge (6 items): All beginning with the heading ''From the legal point of view, it is a practice .'', your response options are: a) Legal throughout Spain, b) Criminal offense throughout Spain, c) Legal only in Andalucía through the Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process, and d) Crime only in Spain through the Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process; 2nd preparation on attention to terminally ill patients (6 items) with yes/no response options; 3rd support that should be provided to patients during the end of life (2 items) with response options of ''Totally disagree, Disagree, Neutral, Agree Totally agree, Does not know/Does not respond''; and 4th a question on whether the student Knows the mechanism to report on carrying out the Living testament, with yes/no response option.
The data gathered were introduced for analysis in the SPSS program version 15.0. A descriptive analysis was performed by using frequencies and percentages for the qualitative variables. For the quantitative variables, the mean and standard deviation were calculated. In the bivariate analysis Pearson's Chi square test was used, statistical significance was assumed when the p value was < 0.05.
RESULTS
The responses obtained from 572 students were analyzed, 316 of which were from Nursing, 113 from Physical Therapy, and 143 from Occupational Therapy. Age ranged between 18 and 51 years, with a mean of 22.1±4.5 years. Of the total surveyed, 450 (78.7%) were women. Some 170 (29.7%) of the students were enrolled in the first course, 185 (32.3%) in the second, and 217 (37.9%) in the third.
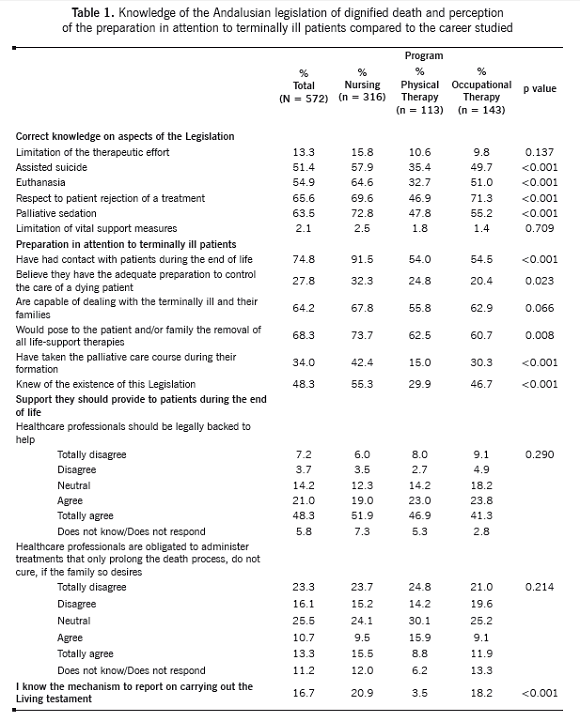
Table 1 show that in the questions on knowledge if from the legal point of view these are legal practices, the proportion of correct responses was greater in ''respect to patient rejection of a treatment'' (65.6%) and in the ''palliative sedation'' (63.5%), with the lowest correct responses for ''limitation in the therapeutic effort'' (13.3%) and ''limitation of vital support measures'' (2.1%). In all the questions in this group, Nursing had greater proportions of correct responses than those presented in the other groups, with statistical significance in four of the six items.
When comparing each of these questions through the condition of having taken or not the assignment of Palliative Care, a statistically significant difference was only found in the item of the practice of palliative sedation, where 72.7% of those who had taken the assignment versus 58.9% of those who had not taken it had correct knowledge (p = 0.001). It may also be observed in Table 1 that, although at the moment of the survey 74.8% of the students surveyed had had contact with patients during end-of-life processes, only 48.3% knew of the existence of the Legislation on dignified death and 34.0% had taken the palliative care course. Even though 64.2% feels capable of dealing with terminally ill patients and their families and 68.3% would pose to them the removal of all life-support therapies, merely 27.8% believe they have adequate preparation to control the care of a dying patient. Within all this group of questions the proportions were also greater in the Nursing career, with the question ''are you capable of dealing with terminally ill patients and their families'' as the only one in which no statistically significant difference was found.
When asked about the support that should be provided by healthcare professionals, seven of every ten surveyed, without distinction by career, agree that they should be legally backed to be able to help patients during the end-of-life process and four of every ten did not agree with the statement that they are obligated to administer treatments that only prolong the death process, do not cure, if the family so desires.
It is a cause for concern that only 16.7% of the participants reported knowing of the mechanism to report on carrying out the living testament. In this question, Nursing and Occupational Therapy had higher percentages than that found in Physical Therapy, with said difference being significant.
DISCUSSION
Approximately half of the participants in this study know of the existence of the ''Legislation of Rights and Guarantees of the Dignity of Individuals during Death processes''.1 The data from our study reveal that most of the students do not know that the limitation of the therapeutic effort is a legal practice in Spain, from the legal point of view. Additionally, a vast majority acknowledged not knowing that, from the legal point of view, the limitation of vital support measures is a legal practice only in Andalucía. This may be due, in part, to such Legislation being published in the BOJA bulletin (Boletín Oficial de la Junta de Andalucía) on 19 March 2010 and the surveys of the students were conducted between June and July of the same year. However, upon analyzing the results in function of the career, we find that nursing students have greater general knowledge of the legislation, while it is only known by one third of those in Occupational Therapy.
When delving on the specific contents of the Legislation, we noted that the participants adequately knew those contained in prior legislations like those related to euthanasia and assisted suicide. But new aspects like limitation of the therapeutic effort and limitations of vital support measures are unknown. In their study, Torres et al.21 described similar results to ours.
The contents learnt in the Palliative Care course implied higher percentages of correct responses in diverse questions made; without any statistically significant differences - except for the question related to palliative sedation, an aspect dealt with specifically in the course. Rodríguez-Morera A and Villegas JM22 in their study on the opinion of students from a graduate program in Occupational Therapy on Palliative Care provided data where most of the therapists posed the need for a greater extension of the course and their main interest was to broaden their knowledge on the topic.
A vast majority of those surveyed recognized not having the proper preparation to control the care of a dying patient. In this sense, Benbunan-Bentata et al.,23 state that helping people die confronts us with our own limits and fears. To solve this problem, they propose teaching strategies that aid in the confrontation and abilities of emotional self-control. Many of the students manifested feeling capable of dealing with terminally ill patients and their families. These statements contrast with the fact that most state not being prepared; this datum coincides with the findings by Cruz et al.,24 and with those by Cantídio et al. 25 What we interpret from this is that the students believe they are capable of dealing with these patients and their families, but when they have to confront real situations, through clinical practices, is when they prove that they do not have the proper preparation to control the care needed by a terminally ill patient.
One fourth of the students surveyed do not have clear understanding if they are obligated to administer treatment that only prolongs the patient's death process in case the family requests it. García-Caro et al.,26 refer to this fact in a study carried out with physicians and nursing professionals. Emotions play a determinant role on how professionals should behave and on their decision making. Likewise, a vast majority of those surveyed recognize not knowing how to report on carrying out the Living testament. This response may be due not so much to ignorance of the Living testament, but to the difficulty in delivering that information to patients and their families, perhaps because of the lack of communication skills. We notice statistically significant difference with respect to the careers; in that most of the Physical Therapy students ignore the reporting mechanism. In general, we can state that students who have taken the Palliative Care course know the legislation best, although it does not seem to be a determinant factor; rather, it is in the concrete formation of the Nursing career where these contents are transversally addressed.
In conclusion, it may be pointed out that Nursing students have more knowledge on the ''Legislation of Rights and Guarantees of the Dignity of Individuals during the Death Process'', followed by those from Occupational Therapy and Physical Therapy. Likewise, those who took the Palliative Care course obtained better results than students who did not take it. Although students do not feel prepared academically to deal with these types of patients, they do consider themselves capable of doing so.
Limitations of the study. This was a preliminary study, with the purpose of defining shortcomings in attention to patients and families of the students of health sciences to guide the development of the Degrees started. The research shows knowledge, opinions, and beliefs of students; we have not evaluated the skills and abilities that would permit students to work with patients during end-of-life processes.
REFERENCES
1. Ley 2/2010, de Derechos y Garantías de la Dignidad de las Personas en el Proceso de la Muerte. BOJA, número 54, de 19-03-2010. [ Links ]
2. Pla L. Aproximaciones a la muerte en Occidente. Aquelarre Rev Centro Cul Univ. 2005;4(7):81-98. [ Links ]
3. Caycedo M. La muerte en la cultura occidental: antropología de la muerte. Rev Col Psiquiatr. 2007;36(2):332-9. [ Links ]
4. García R. Antropología de la muerte: entre lo intercultural y lo universal, en Cuidados Paliativos. San Sebastián: Ed. Sociedad Vasca de Cuidados Paliativos; 2003. p. 305-22. [ Links ]
5. Gorrita R. La relación médico paciente en la sociedad actual: autonomía, integridad y consentimiento informado. Rev Cienc Med la Habana. 2008;14(1). Disponible en: http://www.cpicmha.sld.cu/hab/Vol14_1_08/hab04108.htm [ Links ]
6. Economist Intelligence Unit. The quality of death: Ranking end-of-life care across the world. Ed. Lien Foundation; 2010. Disponible en: www.eiu.com/sponsor/lienfoundation/qualityofdeath [ Links ]
7. García I, Cantón MA. Voluntad vital anticipada, cuidados paliativos y eutanasia. Edita El Observatorio de Salud en Europa EASP. Consejería de Salud. Junta de Andalucía. Septiembre 2005. Disponible en: http://www.easp.es/web/documentos/InformesOSE/00009951documento.pdf [ Links ]
8. Asamblea Parlamentaria del Consejo de Europa. Recomendación 1418. Protección de los derechos humanos y la dignidad de los enfermos terminales y moribundos. Consejo de Europa. 24a Sesión. 1999. [ Links ]
9. Asamblea Parlamentaria del Consejo de Europa. Assistance to patients at end of life. Doc. 10455. Febrero 2005. Disponible en: http://www.assembly.coe.int/Mainf.asp?link=/Documents/WorkingDocs/Doc05/EDOC10455.htm [ Links ]
10. Asamblea Parlamentaria del Consejo de Europa. Assistance to patients at end of life. Doc. 10495. Abril 2005. Disponible en: http://www.assembly.coe.int/Mainf.asp?link=/Documents/WorkingDocs/Doc05/EDOC10495.htm [ Links ]
11. De Miguel C, López A. Eutanasia y suicidio asistido: conceptos generales, situación legal en Europa, Oregón y Australia (I). Med Pal. 2006; 13(4): 207-15. [ Links ]
12. Ley Foral 8/2011, de Derechos y Garantías de la Dignidad de la Persona en el Proceso de la Muerte. (BOE, número 88, de 24-03-2011). [ Links ]
13. Proyecto de ley reguladora de los Derechos de la Persona ante el Proceso Final de la Vida. (Boletín Oficial de las Cortes Generales. Serie A, proyectos de Ley, número 132(1), 17-06-2011). [ Links ]
14. Ley 14/1986 de 25 de Abril, General de Sanidad. BOE, número 102, de 29-04-1986 [ Links ]
15. Ley 2/1998 de 15 de junio, de Salud de Andalucía. (BOE, número 185, de 4-08-1998). [ Links ]
16. Ley 41/2002, de 14 de noviembre, Básica Reguladora de la Autonomía del Paciente y de Derechos y Obligaciones en Materia de Información y Documentación Clínica. (BOE, número 274, de 15-11-2002) [ Links ]
17. Ley Orgánica 2/2007, de 19 de Marzo, de reforma del Estatuto de Autonomía para Andalucía. BOE, número 68, de 20-03-2007) [ Links ]
18. Ley 5/2003, de 9 de Octubre, de Declaración de Voluntad Vital Anticipada. (BOJA, número 210, de 9-10-2003) [ Links ]
19. Libro Blanco Agencia Nacional de Evaluación de la Calidad y Acreditación (ANECA). Título de Grado en Fisioterapia. 2009. [ Links ]
20. Libro Blanco Agencia Nacional de Evaluación de la Calidad y Acreditación (ANECA). Título de Grado en Terapia Ocupacional.2009. [ Links ]
21. Torres LM, Schmidt-RioValle J, Garcia-Garcia I. Preparación del personal sanitario sobre el proceso asistencial de la muerte. [Trabajo Fin de Máster]. Universidad de Granada. 2010. [ Links ]
22. Rodríguez-Morera A y Villegas JM. Formación de Terapia Ocupacional en cuidados paliativos. Opinión de los terapeutas participantes en un curso de postgrado. Med Pal, 2010; 17(1): 9-12. [ Links ]
23. Benbunan-Bentata B, Cruz-Quintana F, Roa-Venegas JM, Villaverde-Gutiérrez C, Benbunan-Bentata BR. Afrontamiento del dolor y la muerte en estudiantes de Enfermería: una propuesta de intervención. Int J Clin Health Psychol. 2007;7(1):197-205. [ Links ]
24. Cruz-Quintana F, García- Caro MP, Schmidt- RioValle J, Navarro-Rivera MC, Prados-Peña D. Enfermería, familia y paciente terminal. Rev ROL Enferm. 2001;24(10):8-12. [ Links ]
25. Cantídio FS, Vieira MA, Sena RR. Significado da morte e de morrer para os alunos de enfermagem. Invest Educ Enferm. 2011;29(3):407-18. [ Links ]
26. Garcia-Caro MP, Cruz-Quintana F, Schmidt-RioValle J, Muñoz-Vinuesa A, Montoya-Juarez R, Prados-Peña D et al. Influencia de las emociones en el juicio clínico de los profesionales de la salud a propósito del diagnóstico de enfermedad terminal. Int J Clin Health Psychol. 2010;10(1):57-73. [ Links ]