Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307
Invest. educ. enferm vol.31 no.2 Medellín May/Aug. 2013
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Characteristics of patients hospitalized at an intensive care unit due to drug abuse
Características de los pacientes internados en una unidad de terapia intensiva por abuso de drogas
Flávia Antunes1; Magda Lúcia Félix de Oliveira2
1RN, Master. Unidade de Terapia Intensiva Adulto do Hospital Universitário de Maringá, Maringá - PR, Brasil. email: flanti@bol.com.br.
2RN,Ph.D. Professor, Universidade Estadual de Maringá, Maringá - PR, Brasil. email: mlfoliveira@uem.br.
Receipt date: April 24, 2012. Approval date: May 8, 2013.
Article linked to research: Usuários de drogas de abuso que necessitaram internação em unidade de terapia intensiva - perfis sócio demográficos, características clínicas
Subventions: none.
Conflicts of interest: none.
How to cite this article: Flávia Antunes F, Oliveira MLF. Characteristics of patients hospitalized at an intensive care unit due to drug abuse. Invest Educ Enferm. 2013;31(2): 201-209.
ABSTRACT
Objective. To characterize the clinical and demographic profile of patients hospitalized due to drug intoxication at an intensive care unit (ICU) of a teaching hospital between 2004 and 2010. Methodology. In this descriptive study, information was collected from the hospitalized patients, as informed by a Toxicology Care Center (CAT) in Paraná (Brazil). The clinical files were checked and information was collected about age, gender, toxic agents and intoxication circumstances, comorbidities and clinical outcomes. Results. Sixty-two patients were included in the study, with a mean age of 58 years and 77% male. Alcohol was the substance related to most hospitalizations (77%), followed by psychoactive drugs (14%) and marihuana and crack (5% each). The main comorbidities were bronchopneumonia due to aspiration (37%), alcohol-related liver cirrhosis (24%) and traumatic brain injury (19%). The most frequent intoxication circumstances were chronic abuse (79%), attemptive suicide (19%) and acute abuse (4.9%). Thirty-nine percent of the patients died during hospitalization. Conclusion. The results show a concerning reality, as most of the patients are men of economically active age, who were intoxicated by a legal substance like alcohol, with a relevant number of deaths. Nurses need to pay particular attention to this health problem, in the context of which they play a fundamental role as educators with a view to the encouragement of healthy lifestyles.
Key words: intensive care units; drug users; hospitalization.
RESUMEN
Objetivo. Caracterizar el perfil clínico y demográfico de los pacientes hospitalizados por intoxicación por sustancias de abuso en unidad de cuidados intensivos (UCI) de un hospital universitario en los años de 2004 a 2010. Metodología. Estudio descriptivo en el que se recolectó información de los pacientes hospitalizados quienes fueron informados por un Centro de Asistencia Toxicológica (CAT) de Paraná (Brasil). Las historias clínicas fueron revisadas y se tomó información sobre edad y sexo, agentes tóxicos y circunstancias de la intoxicación, comorbilidades y resultados clínicos. Resultados. Se incluyeron en el estudio 62 pacientes, que tuvieron un promedio de edad de 58 años y de los cuales el 77% era de sexo masculino. El alcohol fue la sustancia relacionada con el mayor número de internaciones (77%), seguida por los medicamentos sicoativos (14%) y la marihuana y el crack (5%, cada uno). Las principales comorbilidades fueron la bronconeumonía por aspiración (37%), la cirrosis hepática de origen alcohólica (24%) y el traumatismo cráneo-encefálico (19%). Las circunstancias más frecuentes de la intoxicación fue el abuso crónico (79%), la tentativa de suicidio (19%) y el abuso agudo (4.9%). Un 39% de los pacientes falleció durante la internación. Conclusión. Los resultados muestran una preocupante realidad pues los pacientes en su mayoría son hombres en edad económicamente activa, quienes se intoxicaron con una sustancia lícita como es el alcohol, con un número relevante de muertes. El enfermero debe prestar especial atención a este problema de salud, dentro del cual tiene un papel fundamental como educador en el fomento de estilos de vida saludables.
Palabras clave: unidades de cuidados intensivos; consumidores de drogas; hospitalización.
INTRODUCTION
The use of abused drugs almost always leads to harmful consequences for the individual and for society, as they produce disturbances which establish considerable harm to the users' physical and mental health, causing important impacts on their families,1 as well as entailing costs to public safety and justice.2 It may be observed that the number of people using drugs is growing, and, because these are substances which can cause mental and physical dependency, the effects of their chronic use are appearing early leading to associated health problems, long-term hospitalization and an increase in mortality.3
Various fields of scientific knowledge adopt definitions of the terms use, abuse, and drug dependency. The International Classification of Disease (ICD - 10) defines use as any consumption, irrespective of frequency and abuse, consumption associated with recurrent, adverse consequences, these however not characterizing dependency. Dependency is manifested when the use of a substance begins to characterize a dysfunctional state.4 The psychological changes depend on the type of abuse drug consumed. The abused drugs are divided in three groups, in accordance with the activities which they exercise on the Central Nervous System (CNS). The first group is made up of drugs which reduce brain activity, termed CNS depressants; the second group of drugs is made up of those which act increasing brain activity, termed CNS stimulators; and a third group is made up of those drugs which act by qualitatively modifying brain activity, being termed hallucinogens.5
Drug users become progressively tolerant to the intoxications/poisoning they produce and develop signs and symptoms of withdrawal when the toxic agent is removed. In parallel, abusive use causes strain on physical and mental health, which can affect the CNS, liver, heart, pancreas and immune system, making the individuals vulnerable to mental disturbances and illnesses associated with drug use or comorbidities.6 In addition to this, abused drugs are associated with an increase in episodes of violence, accidents and criminality related to drug trafficking, such as robbery, theft and homicides, intensifying the situation of morbimortality through these events and causing an important impact on families and society.1 In the intensive care units (ICU) it may be observed that patients who use abused drugs are mainly hospitalized because of clinical or traumatic complications, acute or acute chronic, usually related to the severity of the drug dependency,7 placing great costs on the Unified Health System (SUS).8 The ICUs are environments where the patients with compromised vital functions and more delicate prognoses are hospitalized and receive complex attention from the specialized health team, in particular from nursing.9 The principle characteristic of a patient hospitalized in ICU is the severity of his clinical status.10 Hospitalization in ICU is a factor which creates suffering for patients and family members, and especially in this population the nursing team must be able to understand and work with their illnesses and difficulties, without judgements or prejudice.
The role of the nurse in providing guidance is of extreme importance, in addition to the role which she takes on between the patient and his family in an environment which is stressful for both.11,12 Although it is important to characterize this populational subgroup for the construction of prevention and control strategies, few reports were found in the Brazilian literature on the hospitalization of patients in ICU from poisoning by abused drugs. For nursing, a profession heavily involved in prevention and care, to recognize the consumer of drugs, as well as his characteristics, health problems and needs, requires the seeking of new strategies for contacting and linking with them, such that it may be possible to design and implant programs of prevention, education, treatment and health promotion which are adapted to the different needs.13 For this reason, this study aimed to establish the clinical and demographic characterization of users of abused drugs hospitalized in an intensive care unit for adults as a result of the secondary effects of the use of the drugs.
METHODOLOGY
This is research with a descriptive and exploratory character, with a quantitative approach, of hospitalizations in an adult ICU in a teaching hospital, located in the North-west of the Brazilian state of Paraná. The hospital studied is accredited to the SUS, being characterized as a public institution prioritizing care, teaching and research activities. Its clientele covers the population of the cities in the North-west region, principally those of the 15th Health Region. The adult ICU has eight beds, and is a center of excellence for attending critically-ill patients in the region within the public health system. It attends clinical and surgical patients, of both sexes, and with a minimum age of 14.
The study population was made up of 62 patients in a critical condition, of both sexes, with a principal or secondary medical diagnosis of poisoning from abused drugs, hospitalized in the ICU in the period January 2004 - December 2010, and accessed via the archives of the Center for Control of Poisonings (CCI/HUM), a support service for toxicological emergencies, a 24-hour on-call service. The data sources were the Annual Hospitalized Patients Report, archived in the CCI/HUM, and the patients' medical records, archived in the Medical Records Service. The Hospitalized Patients Report is a printed list, in which all the patients notified to the Center and hospitalized in hospitals in the North-west of Paraná are recorded manually, after a minimum period of twelve hours of clinical observation.
Data from the Hospitalized Patients Report was noted related to the date of hospitalization - the year in which the case was notified - organized and presented in the periods 2004 - 2007 and 2008 - 2009; patient age - organized in the age ranges of 15 - 19 years old, 20 - 29, 30 -39, 40 - 49, 50 - 59, 60 - 69, and over 70 years of age, and presented by the average age of the population; patient's sex: organized as male or female, and presented as the frequency of the male sex; class of the toxic agent - alcohol, psycho-active medications, other abused drugs and alcohol in association with other drugs; circumstances of the poisoning - chronic use, acute use and use in a suicide attempt; and the case's clinical outcome - as discharge from hospital, or death. Later, the patients' medical records were audited, and records of co-morbidities were observed, with the following selected for the study: aspiration pneumonia, alcoholic liver cirrhosis and traumatic brain injury (TBI), which appear with the highest frequency.
A database was created using the Epi-info software version 3.5.1, in which the data was inputted, processed and analyzed using simple descriptive statistics, so as to present the variables, these being presented in terms of absolute and relative frequencies. The research project was submitted for appreciation by the Ethics Committee for Research Involving Human Beings of the State University of Maringá (COPEP/UEM), which approved it under decision number 184/2011.
RESULTS
In the period 2004 - 2010, the hospitalizations with medical diagnoses of secondary effects of abused drugs represented 3.8% of the total of hospitalizations in ICU in the period (62/1638). The proportion of hospitalizations involving patients who used abused drugs increased gradually: between the years 2004 - 2007 it was 2.2% (20/926) and between 2008 - 2010 was 5.9% (42/712), representing an increase of 110% compared to the previous period. The drug related to hospitalization most was alcohol, present in 80.6% of the medical diagnoses recorded. When not associated with another drug, alcohol was responsible for the hospitalization of 48 patients (77.4%). Nine hospitalized patients had used psycho-active medications (14.4%) and three had used other drugs, such as marijuana or crack (4.8%).
The patients' ages varied between 14 and 72 (with a median age of 58 years old) and were predominantly male (77.4%). The age ranges with the largest number of hospitalized patients were 50 - 59 years old (n=20, 32.3%), 40 to 49 years old (n=14, 25.5%) and 30 to 39 years old (n=11, 17.7%). The principle co-morbidities recorded were aspiration pneumonia, diagnosed in 23 (37.1%); cirrhosis of the liver arising from alcohol use, in 15 (24.1%), and traumatic brain injury (TBI), in 12 patients (19.3%). Other conditions such as chronic kidney disease and upper gastrointestinal bleeding were also diagnosed, in 7 (11.3%) and 5 (8.1%) of the hospitalized patients, respectively. Of these patients, who were hospitalized, 28 (45.2%) remained hospitalized in the ICU for a period of over 15 days: 15 (24.1%) remained hospitalized for between 16 and 30 days and 13 (20.9%) were hospitalized for over 30 days.
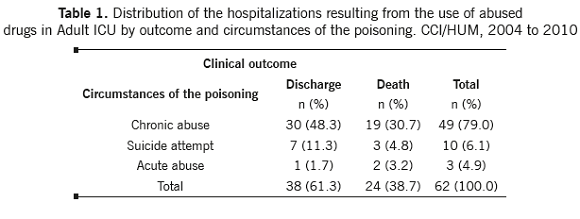
Chronic drug abuse was the circumstance of the poisoning most commonly associated with the etiology of the co-morbidities in the patients hospitalized in ICU (79%), generally because of chronic conditions in acute phases. For the majority of these, the outcome was to be discharged from hospital as â€improved' (48.3%), followed by a relevant number of deaths (30.7%) (Table 1). The majority of the cases of use of abused drugs for suicide attempts culminated in discharge from hospital (11.3%), all related to the use of psycho-active medications. Acute abuse was present in a smaller number of cases (4.9%), of whom two died, as shown in Table 1.
CCI/HUM, 2004 to 2010
DISCUSSION
In the ICU studied, one may observe an important increase in the number of hospitalizations resulting from abused drugs, as 42 (67.7%) were recorded in the last three-year period (2008 to 2010), indicating the consequences of the consumption of abused drugs on the individual's health, which culminates in hospitalization and the overloading of the health services at all levels of care complexity.14 In relation to their use and distribution in society, the abused drugs are classified as licit and illicit. Those classified as licit are products containing psycho-active substances whose production, sale and use are not criminalized, while the illicit drugs are those which may not be sold freely, and whose production and use may be criminalized and repressed.15 Any substance containing alcohol, nicotine, caffeine, non-prescription medications, anorexic agents and anabolic agents may be considered licit.4
Note that alcohol, a licit drug, was responsible for the majority of the hospitalizations, with many of the patients remaining hospitalized for more than 30 days, which is characterized as a long hospitalization. Global consumption of alcohol in developing countries is growing, and this substance is responsible for 4% of deaths occurring in the world, besides being associated with serious social questions.16 Studies indicate that alcohol is the most-consumed drug in Brazil, and, according to the Brazilian Center for Information on Psychotropic Drugs (CEBRID), alcoholism affects from 5 to 10% of the adult Brazilian population.10,17,18
Regarding consequences for individual and collective health, the rates of prevalence of alcohol abuse in populations who seek medical assistance vary from 20% to 50%,17 and each year approximately eight thousand people die as victims of the abuse of licit and illicit drugs in Brazil,18 and, of the abused drugs, it was the abuse of alcohol that was reported most among patients hospitalized in a general hospital.10 The Brazilian population is among the heaviest consumers of alcoholic beverages and the rates of use continue to grow. In addition to this, the country has a tolerant attitude in relation to the consumption of this drug. Due to the ease with which alcohol can be purchased by those under 18 years old, its first use is taking place at ever-younger ages, leading to harmful use and dependence.19
Consumption per capita among consumers of alcohol in Brazil is higher than the average for the world population. This data is considered relevant, as the higher the average consumption in a population, the greater the prevalence of the harm related to this drug.20 It is important to note that alcohol enhances the effects of other drugs when they are used concomitantly, as it creates greater toxicity and prolongs the effects. Its use in association with drugs leads to greater difficulty in control of consumption and, consequently, to an increase in behaviors of risk and clinical situations of greater seriousness.19
The use of psycho-active medications - CNS depressants - is also present in the population studied, and can entail important consequences for the individual's health, related to an increase in morbi-mortality. The consequences of the wide use of these medications can have consequences for the patient's safety, due to impacts for the same in the clinical sphere, resulting in hospitalization.21 In relation to crack, although it is an emerging drug and with proven effects on its users' physical and mental health, it is responsible, along with other illicit drugs, for a small proportion of the deaths caused directly by their consumption. In contrast, alcohol is responsible for the majority of deaths related to drug use in Brazil, being responsible for 85% of these.18
In this study, the patients' ages varied from 14 to 72 years old, with a mean of 58 years old. One can see, therefore, that drug use encompasses a wide age range and that the users, irrespective of their ages, have access to them. In the population in the ICU studied, the researchers were able to see that, independently of age, drugs can be responsible for causing harm to an individual, resulting in a serious state of health for the same, from adolescents through to older adults. It was observed that many of the hospitalized individuals' ages were in the age ranges between 30 and 59 years old, showing a population which is predominantly of an economically-active age, leading one to suppose that the health problems and incapacities created by the problematic use of drugs are important, as identified in previous studies.7,22 In relation to the older individuals, these tend to consume more medications, including over-the-counter medications, including consumption of the medication on its own or with alcohol. The physiological changes which accompany age influence the concentrations of medications and their metabolization, such that the ingestion of various medications and the interaction with other drugs such as alcohol can influence functional capacity negatively, leading the individual to be ill more, as well as psycho-motor skills, which leads the individual to be more prone to accidents, which can result in hospitalization in intensive care, depending on the seriousness of the individual's clinical status.23
The present study confirms men's tendency to greater exposure and, consequently, to the serious effects of drug use on the organism. This tendency of consumption is not different from other regions of Brazil, where the prevalence of deaths and of users who are dependent on abused drugs, in particular alcohol, is prevalent in the male population.10,18 Also in the population studied, many patients were diagnosed with aspiration pneumonia as a co-morbidity. This may be attributed to episodes of nausea, which are quite frequent in patients who ingest substances which depress the central nervous system. Vomiting can occur in people with a reduced level of consciousness, increasing the chances of pulmonary aspiration of gastric contents, potentially causing pneumonia, which further worsens their clinical status.24 Chronic exposure to alcohol can entail a level of toxicity which directly or indirectly affects important organs or body systems, consequently giving rise to diseases such as liver cirrhosis, a disease commonly found in this population.20 In the case of acute poisoning from abused drugs, studies20-25 show their direct relation to accidents and violent episodes, leading to hospitalization due to these events' serious consequences. The high rate of TBI observed in the present study, arising from falls, traffic accidents and fights, indicates this tendency. The use of abused drugs is increasingly frequent in the population and consequently the number of hospitalizations resulting from these substances is also rising. The detrimental effects on the organism resulting from the use and abuse of these drugs often require specialized care due to the seriousness of the cases, which increases the number of hospitalizations of these patients in ICU, causing an even more worrying public health problem. When the abuse of alcohol or other drugs entails hospitalization in intensive care, it is because the problem has taken on even more worrying dimensions, and ends up affecting the entire family structure.26 In the population studied, the patients were in a situation of great seriousness, showing the detrimental effects of consumption of a drug, whether acute or chronic, genuinely capable of ending the individual's life. This consumption can also cause permanent physical and/or emotional sequelae which extend to other people within the patient's social network.2
The authors cannot cease emphasizing that there is sub-notification by the teams in the health services in regard to the attendances and hospitalizations in cases where the patient uses abused drugs. This surveillance is deficient in hospitals in general, principally in those where there are no toxicology centers, there being a significant shortage of data which can be compared with the seriousness of the patients' conditions. What was observed in the population studied is a reflection of global consumption of these substances which is increasingly sizeable and uncontrolled. In Brazil, in 1996 - 2007, there was an increase of 5% in the coefficient of mortality from non-transmissible chronic diseases, including health problems and diseases associated with the harmful use of alcohol; mortality, adjusted for age, from diseases associated with the use of this substance, increased from 4.3 to 5.2 people per 100 thousand persons.27 Although this study was undertaken with a specific population - critically-ill drug users - the characteristics found in this population point to a worrying reality: an increase in the proportion of hospitalizations in ICU over the years; health problems in men, of an economically-active age; a licit drug, alcohol, as the principal abuse drug; the most frequent co-morbidities were aspiration pneumonia, cirrhosis of the liver resulting from alcohol use and TBI; a long period of hospitalization; the majority were chronic drug users; and a high number of deaths, even by the parameters of ICU. In the face of this, it is essential that the nurse trains her team, through continuous education activities, such that all the health professionals involved in the care, directly or indirectly, carry out care which is more humane and of high quality, and which is less stigmatizing to users of abused drugs. The functioning of the nurse at all levels of care, from primary care through to specialized care, with preventive activities, monitoring and guidance, is also essential.
Because this is a subject of current importance, but scarce in nursing studies, there is a need for further discussion and research on this population, so as to investigate its needs and promote better care for this clientele, such that they may face the period of illness, hospitalization and post-hospitalization in a more efficient and dignified way.
REFERENCES
1. Chalub M, Telles LEB. Àol, drogas e crime. Rev Bras Psiquiatr. 2006; 28(Supl II):69-73. [ Links ]
2. Oliveira MLF, Arnauts I. Intoxicação alcoólica em crianças a adolescentes: dados de um centro de assistência toxicológica. Esc Anna Nery. 2011; 15(1):83-9. [ Links ]
3. Pechansky F, Szabot CM, Scivolleto S. Uso de álcool entre adolescentes: conceitos, características epidemiológicas e fatores etiopatogênicos. Rev Bras Psiquiatr. 2004; 26(1):14-7. [ Links ]
4. Souza DPO, Areco KN, Silveira Filho DX. Àol e alcoolismo entre adolescentes da rede estadual de ensino de Cuiabá, Mato Grosso. Rev Saúde Pública. 2005; 39(4):585-92. [ Links ]
5. CEBRID, Centro Brasileiro de Informações sobre Drogas Psicotrópicas. Departamento de Psicobiologia. Universidade Federal de São Paulo - UNIFESP. Drogas Psicotrópicas. São Paulo; 2003. [ Links ]
6. Bau, CHD. Estado atual e perspectivas da genética e epidemiologia do alcoolismo. Ciênc Saúde Coletiva. 2002; 7(1):183-90. [ Links ]
7. Sousa FSP, Oliveira EN. Caracterização das internações de dependentes químicos em Unidade de Internação Psiquiátrica do Hospital Geral. Ciênc Saúde Coletiva. 2010; 15(3):671-7. [ Links ]
8. Gallassi AD, Alvarenga PG, Andrade AG, Couttolenc BF. Custos dos problemas causados pelo abuso do álcool. Rev Psiquiatria Clínica. 2008; 35(1):25-30. [ Links ]
9. Rosa CMR, Fontana RT. A percepção de técnicos em enfermagem de uma unidade de terapia intensiva sobre a humanização no seu trabalho. Rev Ciênc Cuid e Saúde. 2010; 9(4):752-9. [ Links ]
10. Elias ACGP, Tiemi M, Cardoso LTQ, Grion CMC. Aplicação do sistema de pontuação de intervenções terapêuticas (TISS 28) em unidade de terapia intensiva para avaliação da gravidade do paciente. Rev Latino Am Enfermagem. 2006; 14(3): 324-9. [ Links ]
11. Gois CFL, Aguillar OM, Santos V, Rodríguez EOL. Stress factors for patients undergoing cardiac surgery. Invest Educ Enferm. 2012; 30(3):312-9. [ Links ]
12. Silva ND, Contrin L.M. Orientações do enfermeiro dirigidas aos familiares dos pacientes internados na UTI no momento da visita. Rev Arq Ciênc Saúde. 2007; 14(3):148-52. [ Links ]
13. Ministério da Saúde (BR), Secretaria de Atenção à Saúde. A política do Ministério da Saúde para atenção a usuários de álcool e outras drogas. 2nd ed. Brasília (DF): MS; 2004. [ Links ]
14. Ballani TSL, Oliveira MLF. Uso de drogas de abuso e evento sentinela: construindo uma proposta para avaliação de políticas públicas. Texto Contexto Enferm, Florianópolis, 2007; jul-set; 16(3): 488-94. [ Links ]
15. Marques F. Caminhos da prevenção: estudos de CEBRID ajudam a distinguir mito e realidade no panorama do uso de drogas no Brasil. [Internet]. São Paulo: FAPESP; julho 2005 (cited 2011 Apr 15). Available from: http://www.antidrogas.com.br/mostraartigo.php?c=416. [ Links ]
16.World Health Organization. Global Status Report on Alcohol and Health. Geneva: WHO; 2011. (cited 2013 Feb 1). Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/index.html. [ Links ]
17. Pillon SC, Luis MAV. Modelos explicativos para o uso de álcool e drogas e a prática da enfermagem. Rev Latino Am Enfermagem. 2004; 12(4):676-82. [ Links ]
18. Gonçalves A. àlcool é a droga que mais mata [Internet]. Maringá: Gazeta de Maringá; 2012 Feb 5. [cited 2012 Feb 20]. Available from: http://www.gazetadopovo.com.br/vidaecidadania/conteudo.phtml?tl=1id=1220239tit=lcool-e-a-droga-que-mais-mata. [ Links ]
19. Scheffer M, Pasa GG, Almeida RMM. Dependência de álcool, cocaína e crack e transtornos psiquiátricos. Psic: Teor e Pesq. 2010; 26(3):533-41. [ Links ]
20. Duailibi S, Laranjeira R. Políticas públicas relacionadas à s bebidas alcoólicas. Rev Saúde Pública. 2007; 41(5): 839-48. [ Links ]
21. Secoli SR. Polifarmácia: interações e reações adversas no uso de medicamentos por idosos. Rev Bras Enferm. 2010; 63(1):136-40. [ Links ]
22. Alves HNP, Surjan JC, Nogueira-Martins LA, Marques ACPR, Ramos SP, Laranjeira RR. Perfil clínico e demográfico de médicos com dependência química. Rev Assoc Med Bras. 2005; 51(3):139-43. [ Links ]
23. Hulse GK. àlcool, drogas e muito mais entre os idosos. Rev Bras Psiquiatr. 2002; 24(1):34-41. [ Links ]
24. Amaral RA, Malbergier A, Andrade AG. Manejo do paciente com transtornos relacionados ao uso de substância psicoativa na emergência psiquiátrica. Rev Bras Psiquiatr. 2010; 32(2): S104-11. [ Links ]
25. Babor TF, Caetano R. Evidence-based alcohol policy in the Americas: strengths, weaknesses, and future challenges. Rev Panam Salud Publica. 2005; 18(4-5):327-37. [ Links ]
26. Galperim B, Tovo CV, Volpato R, Rodrigues C, Almeida PRL, Stein A, et al. Análise dos escores de gravidade como preditores na mortalidade em cirróticos hospitalizados. Rev Assoc Med Rio Grande Do Sul, Porto Alegre. 2009; 53(3): 221-5. [ Links ]
27. Schmidt MI, Bartholow B, Gulnar G, Menezes AM, Monteiro CA, Barreto SM, et al. Chronic non-communicable diseases in Brazil: burden and current challenges. The Lancet. 2011; 377(9781):1949-61. [ Links ]











 text in
text in