Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307
Invest. educ. enferm vol.31 no.3 Medellín Sept./Dec. 2013
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Nursing actions in the perioperative period and in preparing prostatectomy patients for discharge
Acciones de enfermería en el perioperatorio y en la preparación para el alta hospitalaria del paciente prostatectomizado
Intervenções de enfermagem no perioperatório e no preparo para alta hospitalar do paciente prostatectomizado
Luciana Regina Ferreira da Mata1; Taciana Caldas Ferreira2; Emília Campos de Carvalho3
1RN, Ph.D. Professor Universidade Federal de São João del Rei - UFSJ-, São João Del Rei - MG, Brazil. email: lucianadamata@usp.br.
2Nursing undergraduate student. UFSJ, São João Del Rei - MG, Brazil. email: tacicaldas@yahoo.com.br.
3RN, Ph.D. Professor Escola de Enfermagem de Ribeirão Preto da Universidade de São Paulo EERP/USP, Ribeirão Preto - SP, Brazil. email: ecdcava@usp.br.
Receipt date: Oct 12, 2012. Approval date: Aug 20, 2013.
Article linked to research: Patients submitted to prostatectomy: clinical conditions and nursing care required in perioperative period and at hospital discharge.
Subventions: none.
Conflicts of interest: none.
How to cite this article: Mata LRF, Ferreira TC, Carvalho EC. Nursing actions in the perioperative period and in preparing prostatectomy patients for discharge. Invest Educ Enferm. 2013; 31(3): 406-413.
ABSTRACT
Objective. To identify nursing actions in the perioperative period and in preparing prostatectomy patients for discharge. Methodology. Cross-sectional, retrospective study. Data were collected from medical record of patients who underwent partial or total prostatectomy between August 2009 and August 2010 at hospitals in Divinopolis, Minas Gerais, Brazil. Results. A total of 121 patients were identified; the mean age was 67 years. The most frequent diagnosis was prostate cancer (70%). Main preoperative activities were measuring vital signs (55%), administering drugs (52%), educating patients about fasting (50%), and managing edema (45%). After surgery, the most frequent tasks were measuring vital signs (100%), measuring urine and emptying the urinary bag (100% for each), facilitating the healing of surgical wounds (77%), and evaluating Penrose drain discharge (48%). Among the 25 types of care observed, the activity that nurses performed most often for patients about to be discharged was providing education about urinary catheter manipulation (16%). Conclusion. This study identified weaknesses in care delivery for prostatectomy patients, particularly regarding home care education.
Key words: nursing care; prostatectomy; perioperative care; patient discharge.
RESUMEN
Objetivo. Identificar las acciones de enfermería en el perioperatorio y en la preparación para el alta hospitalaria del paciente prostatectomizado. Metodología. Estudio de corte transversal con toma de información retrospectiva. La recolección de los datos se hizo a partir de las historias clínicas de los pacientes sometidos a prostatectomía parcial o radical entre agosto de 2009 a agosto de 2010 en hospitales de Divinópolis, Minas Gerais, Brasil. Resultados. Se identificaron 121 pacientes, cuya edad promedio era de 67 años. El diagnóstico más frecuente fue el cáncer de próstata (70%). Los principales cuidados preoperatorio fueron: la medición de los signos vitales (55%), la administración de medicamentos (52%), la educación sobre el ayuno (50%) y la administración del enema (45%). En el postoperatorio, entre los que mayores porcentajes presentaron estuvieron: la toma de signos vitales (100%), la medición de la orina y el vaciado de la bolsa recolectora (100% cada uno), la curación de la herida quirúrgica (77%) y la evaluación de la secreción del drenaje de Penrose (48%). Para el alta hospitalaria, de 25 tipos de cuidados observados, el más realizado fue el de la educación sobre la manipulación del catéter urinario (16%). Conclusión. El estudio identificó debilidades en la atención del paciente prostatectomizado, especialmente en la educación para el cuidado en el hogar.
Palabras clave: atención de enfermería; prostatectomía; atención perioperativa; alta del paciente.
RESUMO
Objetivo. Caracterizar o perfil de pacientes prostatectomizados em relação às variáveis sócio-demográficas e clínicas, e identificar ações de enfermagem realizadas no perioperatório e no preparo para alta hospitalar. Metodologia. Estudo transversal, retrospectivo. A coleta de dados foi realizada a partir de registros clínicos de pacientes submetidos a prostatectomia parcial ou radical entre agosto de 2009 a agosto de 2010 em hospitais de Divinópolis, Minas Gerais, Brasil. Resultados. Foram identificados 121 prontuários, cuja idade média foi de 67 anos. O diagnóstico mais frequente foi de câncer de próstata (70%). Os principais cuidados pré-operatórios foram: avaliação de sinais vitais (55%), administração de medicamentos (52%), ensino quanto ao jejum (50%) e lavagem intestinal (45%). No pós-operatório, os cuidados que apresentaram percentuais mais elevados foram: avaliação dos sinais vitais (100%), esvaziamento e mensuração de urina em bolsa coletora (100%), curativo de incisão cirúrgica (77%) e avaliação de secreção do dreno de penrose (48%). Para alta hospitalar, de 25 cuidados registrados, o mais realizado foi quanto o ensino sobre manuseio da sonda vesical (16%). Conclusão. O estudo identificou fragilidades no cuidado do paciente prostatectomizado, principalmente quanto ao ensino para o cuidado domiciliar.
Palavras chaves: cuidados de enfermagem; prostatectomia; assistência perioperatória; alta do paciente.
INTRODUCTION
Global efforts have been made to advance nursing practices in urology, which is recognized as a fundamental area to improve results with patients.1 Prostate cancer and benign prostatic hyperplasia (BPH) are mentioned as important problems among men.2 Prostate enlargement may lead to ureteral obstruction, with its attendant signs and symptoms, including differing degrees of urinary problems.3 This condition often develops after age 50 years. The enlargement could be benign or malignant. Surgical intervention may be required, which can entail removal of only the adenomatous part of the gland, in the case of BPH, or total removal of the prostate and seminal vesicles, in the case of malignancy.4 Erectile dysfunction, urethral stenosis, and urinary incontinence are complications that arise from surgery. Such complications might impair patients' well-being and quality of life and cause psychological symptoms because of embarrassment, loss of self-esteem, and social isolation.5
Nursing has a fundamental role for patients. The care activities that nurses provide at all stages of the perioperative period involve engagement with physical, psychological, social, cultural, or spiritual aspects of the human condition in order to improve patients' quality of life. These nursing activities range from preoperative evaluation of general health status and support, to reestablishing of optimal renal function, and to ensuring good postoperative recovery.3 Studies among patients who have undergone radical prostatectomy report that nursing care must include a focus on the problems that may occur, even temporarily - including psychological symptoms, changes in intestinal or urinary function,5,6 and sexual performance issues.7 Nurses' psychological preparation and development of education skills are recommended so that nurses become able to observe nonverbal signs and address concerns that patients do not directly report.7
In order to illuminate the complexity involved in understanding the specific needs of men undergoing prostatectomy and the relevance of nursing actions that may contribute to better postoperative recovery, this study aimed to characterize the sociodemographic characteristics of patients undergoing prostatectomy and variables and disease characteristics. We also identified nursing actions in the perioperative period and those related to preparation for hospital discharge.
METHODOLOGY
This cross-sectional, retrospective study involved review of the medical records from the Medical and Statistics Filing Service (SAME, acronym in Portuguese) of a large hospital where roughly 115 prostate surgeries are performed annually. Data were collected between February and April 2011 by consulting medical records of all patients who underwent partial or total prostatectomy between August 2009 and August 2010. Researchers developed an instrument to collect data, and three professors from the surgical nursing area reviewed relevance of these data. The instrument consisted of questions on sociodemographic and clinical data, such as date of birth, marital status, duration of hospital stay, medical diagnosis, surgery performed, presence or absence of drains, hospital discharge with or without permanent vesicle catheter (PVC), complications during hospital admission, medical guidance related to care, and nursing care delivery to patients before and after surgery and in preparation for discharge. We evaluated the data using simple descriptive statistical analysis (SPSS software, version 17.0; SPSS Inc., Chicago, Illinois).
The study was approved by the Hospital Ethical and Research Committee (number 30/2011). All guidelines and principles for research on human subjects were followed; privacy and confidentiality of information were preserved. Because only medical records were analyzed, the Ethical and Research Committee waived the need for informed consent.
RESULTS
During the study period (August 2009 to August 2010), 121 medical records were analyzed. The mean patient age (± standard deviation) was 67.4±9.1 years. Most patients were either married (71.9%) or retired (35.6%); 12.4% were active workers. About 70.2% of patients who underwent prostatectomy had a medical diagnosis prostate cancer and 29.8% had a diagnosis of BPH. All patients with prostate cancer underwent total prostatectomy (removal of prostate and seminal vesicles). Surgical techniques identified were transurethral prostate resection (TPR) (26.5%), infraumbilical prostatectomy (70.2%) and transvesical prostatectomy (3.3%).
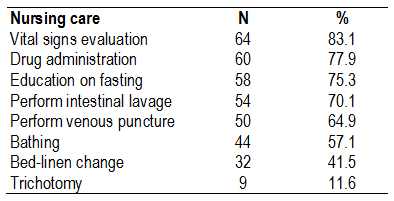
The mean duration of hospitalization for patients who had radical prostatectomy was 5±1.2 days (standard deviation) and 4±3.3 days for those who had partial prostatectomy. Other data analyzed were related to nursing care activities identified in the medical record right after the preoperative period Table 1). Among the main activities were evaluating vital signs (83.1%), administering drugs (77.9%), and providing education on fasting (75.3%). It is meaningful that 44 patients (36.4%) were admitted directly to the operating room on the day of the surgery. Therefore, Table 1 describes care delivery for 77 patients who were immediately assisted in preoperative.
Table 1. Nursing care during immediate preoperative period (n=77) in Divinopolis, Minas Gerais, Brazil, 2011
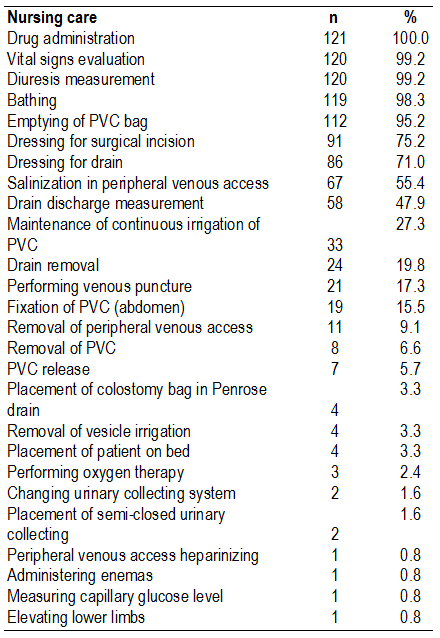
Nursing care activities frequently described in the postoperative period were administering drugs (100.0%), evaluating vital signs, and measuring urinary voiding (99.2% each) (Table 2).
Table 2. Nursing care for 121 patients during postoperative period in Divinopolis, Minas Gerais, Brazil, 2011
Eighty-nine patients who underwent infraumbilical and transvesical prostatectomy had a Penrose drain installed until the last day of hospitalization. The mean number of medicines prescribed for the 121 patients was 4.5±0.7 per patient. The principal drugs were analgesics (100.0%), antiemetics (99.2%), antibiotics (52.0%), and histamine antagonists (33.0%).
Only 24 records related to guidance for discharge were found, which led us to question whether the nurse team performed or recorded this step. Activities identified were management of PVC (n = 19, 15.7%), making appointments for medical follow-up (n = 3, 2.4%), infection prevention (n = 1, 0.8%), and management of surgical wound (n = 1, 0.8%).
DISCUSSION
Prostatic changes often affect men over 60 years old, particularly because aging is a risk factor for prostate enlargement. Approximately three fourths of malignant or benign hyperplasia cases occur ages 60 and 65 years,8 and more than 70% of prostate cancers affect men older than 65 years.9 The mean age found in our study, 67.5 years, corresponded to findings in the literature. Several types of surgical management are used to remove parts of the enlarged prostate or the total gland. Surgical method depends on gland size, obstruction severity, patient age, the patient's general clinical condition, and the presence of associated diseases.9 Radical prostatectomy, the removal of prostate and seminal vesicles, is the standard surgery for prostate cancer patients at potentially curable phase.10 On the other hand, partial prostatectomy is often indicated for treatment of BPH and consists of removing part of prostate, with preservation of the external portion that maintains communication between the bladder and ureter; this method thereby preserves urinary continence after surgery. Transvesical prostatectomy and the TPR are the most frequent surgical techniques to partially remove the prostate; the last one is considered the gold standard for surgical treatment of BPH.11
Concerning nursing care during the preoperative period, we found that checking vital signs, administering drugs, and educating patients about fasting were the activities most often recorded in the medical record. To evaluate vital signs is extremely important to measure patients' physiologic condition in all patients after admission for surgical intervention.12 Drug administration is a responsibility of the nursing team, and nurses must understand the effects of all medicines administered, how they are to be administered, and how to monitor patients' response to treatment.13 Educating patients about fasting is important, especially after surgery, in order to reduce risk for regurgitation of gastric contents.14 However, the benefits of fasting for six or eight hours to avoid risk of gastric aspiration during anesthesia has been questioned in the medical literature. Currently, shortening the preoperative fasting period has been discussed; authors have proposed that patients be offered a carbohydrate-rich drink up to two hours before the surgery as a way to reduce insulin resistance and surgical stress and to improve patients' well-being and satisfaction.15
During the preoperative period, patients undoubtedly have high stress levels and anxiety. These feelings can have negative effects on patients' health status and must be considered.12 Therefore, the nursing team should merge all technical care with educating patients, clarifying the nature and purpose of the procedure, addressing doubts related to the procedure, and providing emotional support. Although in this study nurses were not identified as educators in the preoperative phase, some authors report the importance of this type of intervention to prevent potential problems and to provide information concerning urinary incontinence and erectile dysfunction, which can help improve patient quality of life.16
The goal of nursing care during the preoperative period should be to guarantee a safe recovery and to prevent, identify, and respond to complications that may result from anesthesia.17 In this study, postoperative nursing care delivered to all patients involved drug administration; 100% of the sample received analgesics. Pain is a consequence of surgery and ranged from moderate to severe in 40% to 60% of patients. Pain control is essential for integral care for patient so that other complications are avoided.18 Pharmacologic pain management includes peripherally and centrally acting analgesics. Prescriptions should be administered regularly and follow a scheme according to pain level, thereby providing constant plasma levels, and should be offered for episodes of intense pain.19
For all prostatectomy types, management of PVC commonly involves diuresis measurement and evaluation, emptying of the collecting bag, release, and vesicle irrigation. We observed that most actions requested by medical staff concerned PVC maintenance. Among complications arising from use of PVC are physical and psychological discomfort, bladder stones, renal inflammations, and, more frequently, urinary tract infections, which represent at least 35% of all nosocomial infections.20
To reduce the risk for such complications, nurses can improve their scientific knowledge about PVC care and encourage patients to increase liquid ingestion. Another aspect of postoperative care often required in prostatectomies (except TPR) concerns the Penrose drain. The nursing team should cover all maintenance of the drain, which includes cleaning the drain incision with aseptic technique to eliminate infection risk, promoting traction or mobilization to help eliminate discharge and avoid formation of residual collections, and removing the drain at discharge. Penrose drain is removed in steps, with mobilization of a few centimeters achieved daily; through this process the trajectory of the drain from the deep surface of cavity is eliminated and formation of dead space is avoided upon complete removal.21
It is important to reinforce that radical prostatectomy is considered an aggressive surgery and that urinary continence and erectile function affect a large number of patients.16 As a result, early rehabilitation of urinary continence and sexual activity requires careful preoperative and postoperative evaluation and must be linked to an efficient teaching plan on correct homecare.16
However, hospital stay between admission and discharge of patients undergoing elective surgeries has been quite reduced; patients are admitted on the day of surgery and more closely to surgery time, and there is also a stimulus to early discharge.22 Our study observed this general tendency. Forty-four patients (36.4%) were admitted a short time before the surgery and were forwarded directly to the operating room; this could increase the patient's and family's anxiety about the procedure.
Another finding identified was the scarcity of records (n=24) concerning guidance provided by nursing team for discharge, raising the question of whether nurses performed or recorded this step in care. Nursing guidance involves communicating with patients, keeping them informed, and recognizing needs in different operative periods; nurses therefore use adaptive strategies that enable the individual to deal with possible surgical morbidities in the postoperative period.23 The decrease in hospital stay also reduces the time available for guidance and education of patients and time for addressing concerns. Important strategies for developing effective patient education concerning discharge involve providing written materials, using checklists on education applied in the hospital to guarantee consistency of patient education, and involving partners in education sessions.24
When patients are admitted to the hospital, discharge can be the moment most anticipated by patients and their family. Generally, the concern over the day of return to home becomes greater than the expectations for the surgical procedure itself.23 In most cases, the nurse has an important role in preparing prostatectomy patients for discharge, especially because these patients leave the hospital with doubts and expectations related to management of PVC, surgical incision, and function of the urinary and reproductive system.25 For this reason, educational interventions related to preparation for discharge must be a priority to increase patients' knowledge about their care needs and promote changes in behavior to stimulate self-care. 24
The telephone follow-up is another strategy mentioned in the literature to improve education for discharge, especially considering the trend toward short hospital stays. This method has been used mainly to follow up patients who have undergone surgery and are not considered to be at high risk; it enables them to have as normal a life as possible away from the hospital environment. This care strategy is considered better for the service because it reduces workload in the conventional system for outpatient unit follow-up.26 It may also result in reduced costs by avoiding readmissions. 27
The sociodemographic characteristics and mean age of our patients are similar to those reported in the national and international literature. Among clinical characteristics, the most common prostatic diagnosis was prostate cancer and the main intervention was surgery involving total removal of the prostate gland seminal vesicles. All postoperative interventions identified were physical, and some care activities were delivered more frequently than others. This finding shows differences in the routine of care delivery for prostatectomy patients. Checking vital signs, administering drugs, and educating patients about fasting were the preoperative care activities most frequently mentioned. In the postoperative period, analgesic drugs were administered to 100% of the sample. With regard to nursing interventions for discharge preparation, the scarcity of relevant records made the analysis harder and raised questions about whether nurses performed these activities. However, we could not determine whether this approach is being neglected or is simply not being reported by the nursing team.
This study is limited by collection of data from medical records; it is possible that certain care activities are being performed but are not being recorded. The study findings, including the weakness of records on guidance for homecare and psychosocial intervention, can be used to stimulate reflection on need for changes in nursing practice that could improve the quality of patient care.
REFERENCES
1. Thompson K, Marley J, Taylor J, Basketter V, O'Neill K, Parahoo K, et al. A baseline description of the research, clinical practice and development needs of urology nurses in the United Kingdom. J Urol Nurs. 2007; 1(1):36-46. [ Links ]
2. Napoleão AA, Caldato VG, Petrilli Filho JF. Diagnósticos de enfermagem para o planejamento da alta de homens prostatectomizados: um estudo preliminar. Rev Eletrônica Enferm. 2009;11(2):286-94. [ Links ]
3. Hunter KF, Moore KN, Cody DJ, Glazener CMA. Conservative management for postprostatectomy urinary incontinence (Cochrane Review). In: The Cochrane Library. Oxford: Update Software; 2007. [ Links ]
4. Nagle GM. Cirurgia genitourinária In: Meeker MH, Rothrock JC. Alexander Cuidados de enfermagem ao paciente cirúrgico. 13rd Ed. Rio de Janeiro: Guanabara Koogan; 2007. [ Links ]
5. Steineck G, Helgesen F, Adolfsson J, Dickman PW, Johansson J, Norlén BJ, et al. Quality of life after radical prostatectomy or watchful waiting. N Engl J Med. 2002; 347(11):790-6. [ Links ]
6. Palmer MH. Using epidemiology in patient education for post-prostatectomy urinary incontinence. Ostomy Wound Manage. 2001; 47(12):20-5. [ Links ]
7. Chambers SK, Schover L, Halford K, Clutton S, Ferguson M, Gordon L, et al. ProsCan for Couples: randomised controlled trial of a couples-based sexuality intervention for men with localisedprostate cancer who receive radical prostatectomy. BMC Cancer. 2008; 8:226. [ Links ]
8. Humphreys MR, Fernandes KA, Sridhar SS. Impact of Age at Diagnosis on Outcomes in Men with Castrate-Resistant Prostate Cancer (CRPC). J Cancer. 2013; 4(4): 304-14. [ Links ]
9. Rigdon JL. Robotic-assisted laparoscopic radical prostatectomy. AORN J. 2006; 84(5):760-70. [ Links ]
10. Sfoungaristos S, Perimenis P. Clinical and pathological parameters predicting extracapsular disease in patients undergoing a radical prostatectomy for clinically localized prostate cancer. Prague Med Rep. 2012; 113(1):5-15. [ Links ]
11. Ribeiro JC, Carvalho AP, Santos AR. Terapeutica actual da Hipertrofia Benigna da Prostata. Acta Urol. 2006; 23(1):93-9. [ Links ]
12. Christóforo BEB, Carvalho DS. Cuidados de Enfermagem realizados ao paciente cirúrgico no período pré-operatório. Rev Esc Enferm USP. 2009; 43(1):14-22. [ Links ]
13. Silva DO, Grou CR, Miasso AI, Cassiani SHDB. Preparo e administração de medicamentos: análise de questionamentos e informações da equipe de enfermagem. Rev Lat Am Enfermagem. 2007; 15(5):1010-7. [ Links ]
14. Moro ET. Prevenção da aspiração pulmonar do conteúdo gástrico. Rev Bras Anestesiol. 2004; 54(2):261-75. [ Links ]
15. Aguilar-Nascimento JE, Perrone F, Prado LIA. Jejum pré-operatório de 8 horas ou de 2 horas: o que revela a evidência? Rev Col Bras Cir. 2009; 36(4):350-2. [ Links ]
16. Carvalho JMS, Cristão ASM. El valor de los cuidados de enfermería: la consulta de enfermería del hombre sometido a prostatectomía radical. Rev Enf Ref. 2012; serIII(7): 103-12. [ Links ]
17. Rossi LA, Torrati FG, de Carvalho EC, Manfrim A, da Silva DF. Diagnósticos de enfermagem do paciente no período pós-operatório imediato. Rev Esc Enferm USP. 2000; 34(2):154-64. [ Links ]
18. Secoli SR, Padilha KG, Litvoc J. Análise custo-efetividade da terapia analgésica utilizada na dor pósoperatória. Rev Lat Am Enfermagem. 2008; 16(1):42-6. [ Links ]
19. Chaves LD, Pimenta CAM. Controle da dor pós-operatória: comparação entre métodos analgésicos. Rev Lat Am Enfermagem. 2003; 11(2):215-9. [ Links ]
20. Bernard MS, Hunter KF, Moore KN.A review of strategies to decrease the duration of indwelling urethral catheters and potentially reduce the incidence of catheter-associated urinary tract infections. Urol Nurs. 2012; 32(1):29-37. [ Links ]
21. Cesaretti IUR, Saad SS. Drenos laminares e tubulares em cirurgia abdominal: fundamentos básicos e assistência de enfermagem. Acta Paul Enferm. 2002; 15(3):97-106. [ Links ]
22. Silva LGDM, Lacerda RA. Problemas de usuários cirúrgicos após a alta hospitalar e a atuação de enfermagem. Online Braz J Nurs [Internet]. 2006 (cited 2009 Sep 25); 5(2). Available from: http://www.uff.br/objnursing/index.php/nursing/article/view/330/74 [ Links ]
23. Carvalho ARS, Matsuda LM, Stuchi RAG, Coimbra JAH. Investigando as orientações oferecidas ao paciente em pós-operatório de revascularização miocárdica. Rev Eletrônica Enferm. 2008;10(2):504-12 [ Links ]
24. Fredericks S, Guruge S, Sidani S, Wan T. Post-operative patient education: A systematic review. Clinical Nursing Research: An Int J. 2010;19 (2):144-64. [ Links ]
25. Mata LRF, Napoleão AA. Intervenções de enfermagem para alta de paciente prostatectomizado: revisão integrativa. Acta Paul Enferm. 2010;23(4):574-9. [ Links ]
26. Anderson B. The benefits to nurse-led telephone follow-up for prostate cancer. Br J Nurs. 2010;19(17):1085-90. [ Links ]
27. Naffe A. Postdischarge follow up phone call. Heart lung. 2012;41(99):102. [ Links ]