Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Investigación y Educación en Enfermería
Print version ISSN 0120-5307
Invest. educ. enferm vol.31 no.3 Medellín Sept./Dec. 2013
ARTÍCULO ORIGINAL / ORIGINAL ARTICLE/ ARTIGO ORIGINAL
Risk factors of foot ulceration in patients with Diabetes Mellitus type 2
Factores de riesgo de ulceración de pies en pacientes con Diabetes Mellitus tipo 2
Fatores de risco de ulceração de pés em pacientes com Diabetes Mellitus tipo 2
Patricia Bañuelos-Barrera1; Elva Dolores Arias-Merino2; Yolanda Banuelos-Barrera3
1RN, Ph.D. Professor Universidad Juárez del Estado de Durango -UJED-, Durango, México. email: pbanuelosb@hotmail.com.
2Gerontologist, Ph.D. Professor Universidad de Guadalajara, Jalisco, México. email: elvadolores@yahoo.com.
3RN, Ph.D. Professor UJED, Durango, México. email: yobanuelos@gmail.com.
Receipt date: Oct 13, 2012. Approval date: May 8, 2013.
Article linked to research: Intervención educativa conductual en personas con diabetes en riesgo de ulceración.
Subventions: Apoyo parcial del Consejo Nacional de Ciencia y Tecnología (No. 94670).
Conflicts of interest: none.
How to cite this article: Bañuelos-Barrera P, Arias-Merino ED, Bañuelos-Barrera Y. Risk factors of foot ulceration in patients with Diabetes Mellitus type 2. Invest Educ Enferm. 2013;31(3): 442-449.
ABSTRACT
Objective. Identify the risk factors for foot ulceration in patients with diabetes type 2 (DM2) who attended a primary care center in the city of Colima (Mexico). Methodology. This was a descriptive cross-sectional study conducted during 2012 with the participation of 87 patients with DM2 from both sexes and older than 30 years of age. Socio-demographic, anthropometric, clinical, and biochemical variables were measured. The study inquired about prior evaluation of the feet and prior education on diabetes by the healthcare team. Results. The mean age was 59 years and 70% were women. The average number of years since diagnosis was nine years; only 35% had good glycemia control; 66% engage in exercise; 51% wear open shoes; none had temperature differences in the feet; 82% had some type of dermatological abnormality; 50% had deformities in their feet. A total of 24% had been diagnosed with peripheral neuropathy and another 11% had peripheral vascular disease. Sixty percent of all the patients had risk of foot ulceration. Only 23% of the participants had had previous foot exams. One of every three diabetic patients had received education about the disease. Conclusion. An important proportion of the patients had risk of foot ulceration, contrary to the insufficient percentage of individuals with previous inspection and education about foot care. For nursing, it is an area of opportunity in this level of care to improve the inspection and education on diabetes, specifically on foot care, mainly in those patients with a prolonged evolution of the disease, deficient glycemia control, and risk of ulceration.
Key words: foot ulcer; Diabetes Mellitus type 2; patient education as topic.
RESUMEN
Objetivo. Identificar los factores de riesgo para la ulceración del pie en pacientes con diabetes tipo 2 (DM2) quienes asisten a un centro de primer nivel de atención en la ciudad de Colima (México). Metodología. Estudio descriptivo transversal realizado durante 2012 con la participación de 87 pacientes con DM2 de ambos sexos y mayores de 30 años. Se midieron variables socio-demográficas, antropométricas, clínicas y bioquímicas. Se indagó valoración previa de pies y educación previa en diabetes por parte del equipo de salud. Resultados. La edad promedio fue de 59 años; el 70%, mujeres. El promedio de años desde el diagnóstico fue 9; tan solo un 35% tenía buen control glucémico, el 66% realiza ejercicio, un 51% usa zapato abierto, ninguno tuvo diferencias de temperatura en los pies, un 82% tuvo algún tipo de anormalidad dermatológica, el 50% tenía deformidad en sus pies. Un 24% tenía diagnóstico de neuropatía periférica y otro 11% tenía enfermedad vascular periférica. El 60% de todos los pacientes tuvo riesgo de ulceración de los pies. A solo el 23% de los participantes se le había realizado revisión previa de pies. Uno de cada tres diabéticos había recibido educación sobre su enfermedad. Conclusión. Una proporción importante de los pacientes tuvo riesgo de ulceración de pies, en contradicción al porcentaje insuficiente de personas con revisión y educación previa sobre cuidado de pies. Para enfermería es una oportunidad trabajar en esta área y en este nivel de atención para mejorar la revisión y educación en diabetes, específicamente en el cuidado de pies, principalmente en aquellos pacientes con una larga evolución de la enfermedad, deficiente control glucémico y riesgo de ulceración.
Palabras clave: úlcera del pie; Diabetes Mellitus tipo 2; educación del paciente como asunto.
RESUMO
Objetivo. Identificar os fatores de risco para a ulceração do pé em pacientes com diabetes tipo 2 (DM2) que assistem a um centro de primeiro nível de atendimento na cidade de Colima (México). Metodologia. Estudo descritivo transversal realizado durante 2012 com a participação de 87 pacientes com DM2 de ambos sexos e maiores de 30 anos. Mediram-se variáveis sócio-demográficas, antropométricas, clínicas e bioquímicas. Indagou-se valoração prévia de pés e educação prévia em diabete por parte da equipe de saúde. Resultados. A idade média foi 59 anos, o 70% foram mulheres. A média de anos desde o diagnóstico foi 9 anos, tão só um 35% tinham bom controle glicêmico, o 66% realiza exercício, um 51% usa sapato aberto, nenhum teve diferenças de temperatura nos pés, 82% tiveram algum tipo de anormalidade dermatológica, 50% tinha deformidade em seus pés. Um 24% tinha diagnóstico de neuropatia periférica e outro 11% tinha doença vascular periférica. O 60% de todos os pacientes tiveram risco de ulceração dos pés. A só o 23% dos participantes se lhe tinha realizado revisão prévia de pés. Um de cada três diabéticos tinha recebido educação sobre sua doença. Conclusão. Uma proporção importante dos pacientes tiveram risco de ulceração de pés, em contradição à percentagem insuficiente de pessoas com revisão e educação prévia sobre cuidado de pés. Para enfermaria é um área de oportunidade neste nível de atendimento o melhorar a revisão e educação em diabete, especificamente no cuidado de pés, principalmente naqueles pacientes com uma longa evolução da doença, deficiente controle glicêmico e risco de ulceração.
Palavras chaves: úlcera do pé; Diabetes Mellitus tipo 2; educação de pacientes como assunto.
INTRODUCTION
Foot ulceration (FU) is one of the chronic complications of Diabetes Mellitus type 2 (DM-2), which cause high healthcare costs,1 with prevalence among individuals with DM-2 of up to 10%,2 which precedes amputation in up to 85% of the cases.3 Because of this, it is important to have early recognition of the risk factors of ulceration in primary care, and categorize that risk by degrees of affectation that permit timely care in each specific case, to diminish it and - whenever possible - control it before its evolution to amputation. Among the main factors for foot ulceration, we find peripheral neuropathy, peripheral vascular disease, foot deformity, and penetrating trauma.4 Lack of education on DM-2 has also been considered a risk factor of ulceration.5 In this respect, the International Working Group on Diabetic Foot (IWGDF)6 recommends examining the feet of all patients at least once a year. In those presenting risk factors, the inspection should be at least every six months and, thus, assign them to a risk category that guides subsequent management to prevent ulceration, re-ulceration, and amputation.
In primary care, the demand from the consultation service is high and it is unlikely that care is offered exclusively to patients with diabetes, which limits early detection of lesions of the foot and establishment of educational programs for prevention. Nursing personnel should assume foot exams and education on diabetes to patients as part of their daily work. For this purpose, they could take advantage of their closeness with users to put into practice the international recommendations with respect to foot care.6,7 That would be translated into efficient detection of feet at risk of ulceration, contribute in diminishing the incidence of serious complications like amputation, and would reduce costs. Due to this, the purpose of this study was to identify the risk factors for foot ulceration in patients with DM-2 who attend to its control in a primary care center.
METHODOLOGY
This was a cross-sectional descriptive study. Sample size was 87 patients with DM-2 who attended general consultation in a primary care center during 2012. The investigation included patients from both sexes, older than 30 years of age, who had no physical limitations that would keep them from participating in the study.
Information was collected about socio-demographic characteristics (age, sex, educational level, and marital status), antecedents of the disease, anthropometric measurements (weight, height, waist and hip circumference), and biochemical measurements (hemoglobin A1C, values of 7% or less were considered good glycemia control). To evaluate weight, height, circumferences, and body composition, the following were used: a TANITA scale (model BC-558 Segmental Body Composition Monitor), a fiberglass tape measure, and a retractable stadiometer (Seca). Regarding body composition,8 the male sex was considered overweight from 21 to 26% (obesity at 27% and more) in age groups from 18 to 39 years; from 22 to 27% (obesity at 28% and more) in the age group from 40 to 59 years; and from 25 to 29% (obesity at 29% and more) in the age group 60 years and more. In the female sex, the body fat values to be considered overweight were from 35 to 39% (obesity at 40% or more) in the age group from 18 to 39 years; from 36 to 40% (obesity at 41% and more) in the age group from 40 to 59 years; and from 37 to 41% (obesity at 42% and more) in the age group 60 years and more.
The clinical variables included evaluation of feet to assess the presence of peripheral neuropathy upon considering the lack of sensation in at least one of four sites9 with the Semmes-Weinstein monofilament, caliber 5.07 (Touch-Test Sensory Evaluators, North Coast Medical). Peripheral vascular disease was considered present when the patient showed ankle-brachial index values below 0.90,10 measured with Baumanometer number 11 or 12 (Welch Allyn) and with Doppler ultrasound carried out with an 8-MHz transducer (Huntleigh Health Care). Dermatology evaluation and musculoskeletal evaluation (presence of foot deformity) were conducted and neuropathic and vascular symptomatology was evaluated. Based on these, the risk of ulceration was assessed, which was categorized according to IWGDF6, thus: 0 = ''without risk'', when no peripheral neuropathy or foot deformity is present; 1 = ''slight risk'', when peripheral neuropathy and/or deformity is present; 2 = ''moderate risk'' if additionally peripheral vascular disease is present; 3 = ''high risk'', when antecedent is already present of ulcer or amputation.
Likewise, temperature of the feet was measured in six different sites of each foot: first segment (big toe), first, third, and fifth metatarsal heads, center of the mid-foot and heel.11 An increase above 2.2 °C in one foot in comparison to the other was considered a sign of inflammation11 and, hence, a foot at risk of ulceration. For this, a digital infrared thermometer was used (Temp Touch Xilas Medical, San Antonio, Texas). Additionally, inquiry was made about prior evaluation of the feet and previous education on diabetes; for this purpose, we identified patients with DM-2 attending consultation and with whom it was verified that they fulfilled the inclusion criteria. Thereafter, they were invited to participate in the study, explained the objective, and subjected to complete evaluation of the feet and anthropometric measurements. During a subsequent appointment blood samples were taken from the participants, with prior verification of at least 4-h fasting, after which they were given a snack to avoid hypoglycemia readings. The approximate time to gather data from each patient was 30 min. Data analysis was performed with the SPSS statistical package (version 17.0).
The study was carried out according to the principles of the Helsinki Declaration.12 Informed signed consent was obtained from the participants. The results of the evaluations were sent to each patient's home and a copy was attached to their clinical file. When the patient had any alteration, he or she was referred to a treating physician.
RESULTS
The socio-demographic characteristics of the 87 patients with DM-2 participating in this research were the following: mean age of 58.8±12.2 years, 70.1% were women, average educational level was 5.6 years, 54.0% had a partner, and 51.7% were dedicated to household work. Regarding involvement in physical exercise, 65.5% of the participants claimed they engaged in such systematically. The type of exercise was low impact (walking) in 96.8%, for which they invested an average of 17 minutes per session (median = 0), with an average weekly frequency of 2.5 days (median = 0).
As per anthropometric characteristics, an average Body Mass Index (BMI) was found of 29.3±5.6 kg/m2 in a range of 28.4 kg/m2. Based on this, 41.4% of the women and 5.8% of the men were obese (χ2=13.1, ρ=0.02). Waist circumference figures ranged between 72 and 130 cm; with relation to these, 65% of the women and 9.2% of the men had cardiovascular risk (χ2=37.9, ρ<0.001). With respect to body composition, from which body fat was considered, 50.6% of the women and 8% of the men were obese (χ2=19.2, ρ<0.001).
Moving on to the clinical characteristics, the average time of evolution of DM-2 was 9.1±7.4 years, 85% had established pharmacological treatment (of which half had a combination of biguanide with sulfonylureas), 37.9% had had chronic complications, with the most frequent being high blood pressure (36.3%). Low prevalence of cigarette smoking (12.6%) and alcoholism (13.8%) were found. The figure of average glycated hemoglobin (A1C) in the participants was 8.3±2.2% within a range of 7.8%, a figure corresponding to poor glycemia control. A total of 42.5% of the participants had good glycemia control.
In relation to patients' feet, 2.4% had antecedents of previous ulcer or active ulcer, 48.3% had varicose veins and 9.2% had poor circulation; in the rest of the patients antecedents were not reported. Neuropathic symptomatology was present in 67.8% (59 patients) of the participants, of these 86.4% had it in both feet. Vascular symptomatology was present in 24.1% (21 patients) of the participants, of which 81% had it in both feet. The dermatology evaluation was abnormal in 81.6% (71) of the patients, mostly (93%) in both feet.
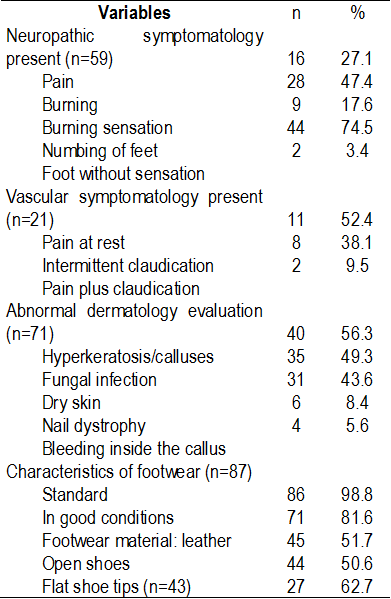
With respect to footwear characteristics, it was observed that nearly half of the participants (44) wore open footwear and had other characteristics that exposed them to foot trauma (Table 1). It must be highlighted that the temperature of the feet did not reveal differences above 2.2 °C from one foot to the other.
Table 1. Evaluation of feet and footwear of patients with DM-2
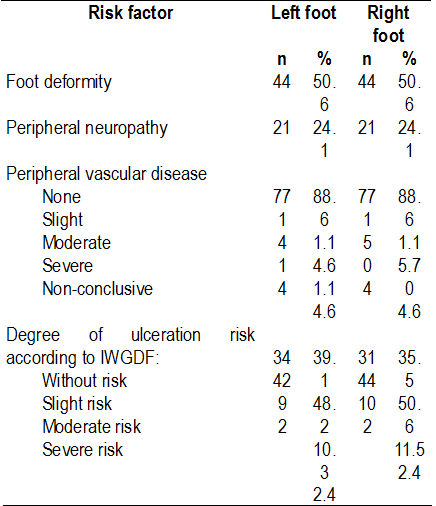
Regarding the degree of risk of foot ulceration of the participants according to the IWGDF categorization,6 it was found that more than 60% had some degree of risk, predominating slight risk; without statistically significant difference per foot (Table 2).
Table 2. Risk factors for ulceration found and degree of risk categorized in 87 patients with DM-2
Upon asking the participants about prior inspection of their feet by the healthcare team, 77.0% answered that their feet had never been inspected; while only 34.4% stated having received education on diabetes, without it being specific on foot care. Of these, 80.4% received group education, provided in 71.2% by a multidisciplinary team; those who received it individually, said they received it from their treating physician (14.9%).
DISCUSSION
Based on the results of the foot exams practiced on these patients, risk factors were found for ulceration, like foot deformity, peripheral neuropathy, and peripheral vascular disease. With relation to peripheral neuropathy data has been reported consistent with our findings,13,14 and other data differing with findings above 90%,4 a difference that can be because the population in that study was seen in a third tier healthcare institution, implying greater complexity of the patient's pathology.
With respect to peripheral vascular disease, our data were similar to those reported by Bustos and Prieto,15 but much lower than those estimated by Lavery et al.,4 at 29%, which could be due to differences in the process followed for its detection, given that ankle-brachial index values may be biased by the presence of calcification of blood vessels in diabetic patients,10 which makes it necessary to use other more complex evaluations like the evaluation of trans-cutaneous oxygen pressure, which along with angiography of lower limb arteries tend to be more precise and complementary to rule out or confirm the disease, given that on some occasions it is asymptomatic. Upon categorizing the risk of ulceration according to the IWGDF classification,6 a high percentage of participants were found at risk, which although the majority were at slight risk, this could increase with the evolution of the diabetes,16 which is why it is necessary to regularly evaluate these patients to monitor compliance with the recommendations for prevention of ulcers.6, 7
Although the IWGDF6 risk of ulceration classification is a simple evaluation, which provides guidelines of the type of necessary intervention according to the risk category proposed, few studies have used it, which hinders comparison of the results; although it is necessary to carry out a standardizing process due to the diversity of variables and categories proposed.17 Two studies in which this classification has been used18, 19 have found that three of every five of these patients have some degree of risk of ulceration, data consistent with this study; while Ndip et al.,20 reported that more than 90% of their patients with DM-2 has high risk of ulceration, probably because the population from that study also suffered chronic renal failure. This is important to consider, given that risk may increase when the patient has other microvascular complications, making early risk evaluation valuable from primary care, for the patient to be referred to a specialist and, thus, diminish or revert that risk.21 It is known that when patients are located in the low-risk category they have a 5% probability of ulcerating within three years and if the risk is high, the probability increases up to almost 60%.17
Of all the participants, only one patient had active ulcers at the moment of the physical exploration of the feet, which is a low frequency in relation to that reported elsewhere,2 which have shown ulceration prevalence ranging from 4 to 10%. This may be because the patients from that study were from a primary care institution and, hence, present fewer complications than those attending a second or third tier healthcare institution.
It is interesting to see the low percentage of patients who have had their feet examined previously, considering that the average of the evolution of the disease was almost 10 years. It is known that the foot inspection is carried out systematically on only 20% of the patients and that, generally, it is not carried out in high-risk patients in first and second tier healthcare.22,23
Recently, foot inspection has been reported as preventive care of ulceration in only 30% of the patients with DM-2 in an approximate 2-year period of time,24 data similar to that found in this study, which shows the scant participation of healthcare personnel regarding early detection of foot complications, perhaps due to lack of knowledge, time, or due to lack of interest, but which finally does not help diminish the existing ulceration and amputation rates. This is an area of opportunity for nursing, which can establish foot ulcer prevention programs in primary care, considering the foot exams, patient training, and timely referral to prevent complications.6,7 In this respect, it is worth highlighting that scant education on diabetes received by the participants, which was not specific for foot care, and was not provided by nurses, professionals whose potential could be used for said effect.
Lack of education on foot care has been verified by Lavery et al.,24 who during a 30-month follow up observed that only 1.3% of the patients at high risk of complications received this type of education. A possible explanation is that when patients with DM-2 also have other pathologies, for example chronic renal failure, care is prioritized on the complication, with little importance assigned to education on diabetes to prevent foot complications, and on other occasions, the healthcare personnel is not up to date with the international recommendations related to diminishing the problem of the feet.6,7 To learn this problem's real motive, we would require identifying the situation that prevails in each institution.
This study permitted identifying and categorizing the risk of foot ulceration in patients with DM-2, attending disease control at a primary care center in a Mexican province, emphasizing on the difficulty of poor education on foot ulcer prevention measures received by these individuals. The aforementioned is a development space for nursing professionals, given that they are in the capacity to evaluate and educate patients on aspects of prevention of diabetes complications, among them foot care.
REFERENCES
1. Cavanagh P, Attinger C, Abbas Z, Bal A, Rojas N, Xu Z. Cost of treating diabetic foot ulcers in five different countries. Diabetes Metab Res Rev. 2012; 28(Suppl 1):107-11. [ Links ]
2. Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ. Diabetic foot syndrome: Evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-hispanics whites from a diabetes disease management cohort. Diabetes Care. 2003; 26(5):1435-38. [ Links ]
3. International Working Group on the Diabetic Foot. Epidemiology of diabetic foot infections in a population based cohort. In: International Consensus on the Diabetic Foot; Noordwijkerhout, the Netherlands; May 22-24 2003. [ Links ]
4. Lavery LA, Peters EJG, Armstrong DG. What are the most effective interventions in preventing diabetic foot ulcers? Int Wound J. 2008; 5:425-33. [ Links ]
5. Reiber GE, Pecoraro RE, Koepsell TD. Risk factor for amputation in patient with diabetes mellitus: a case-control study. Ann Intern Med. 1992;117:97-105. [ Links ]
6. International Working Group on the Diabetic Foot. Consultative section of the International Diabetes Federation. Practical guidelines on the management and prevention of the diabetic foot based upon the International Consensus on the diabetic foot. Amsterdam: International Diabetes Federation & International Working Group on the Diabetic Foot; 2007. [ Links ]
7. American Diabetes Association. Executive Summary: Standards of medical care in diabetes 2013. Diabetes Care 2013; 36(S1):S4-S10. [ Links ]
8. Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgtroyd PR, Sakamoto, Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000; 72: 694-701. [ Links ]
9. Singh N, Armstrong D, Lipsky B. Preventing foot ulcers in patients with diabetes. JAMA 2005; 293(2):217-28. [ Links ]
10. Schaper NC, Andros G, Apelqvist J, Bakker K, Lammer J, Lepantalo M, et al. Specific guidelines for the diagnosis and treatment of peripheral arterial disease in a patient with diabetes and ulceration of the foot. Diabetes Metab Res Rev. 2012; 28(Suppl 1):236-37. [ Links ]
11. Lavery LA, Higgins KR, Lanctot DR, Constantinides GP, Zamorano RG, Armstrong DG, et al. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care. 2004; 17(11):2642-47. [ Links ]
12. World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. 2008 (cited 28 Jan 2010). Available from:http://www.wma.net/e/policy/b3.htm. [ Links ]
13. Aliss S, Cervantes R, Ibarra O, González B. Prevalencia de neuropatía periférica en diabetes mellitus. Acta Méd Grupo Ángeles. 2006; 4(1):13-7. [ Links ]
14. Bruce S, Young T. Prevalence and risk factors for neuropathy in a Canadian first nation community. Diabetes Care. 2008; 31:1837-41. [ Links ]
15. Bustos R, Prieto S. Factores de riesgo de ulceración de los pies en diabéticos tipo 2. Rev Med IMSS. 2009; 47(5):467-76. [ Links ]
16. Ahn YB. Risk factors for foot ulceration in diabetic patients. J Korean Diabetes. 2011; 12:76-9. [ Links ]
17. Monteiro-Soares M, Boyko EJ, Ribeiro J, Ribeiro I, Dinis-Ribeiro M. Risk stratification system for diabetic foot ulcers: A systematic review. Diabetologia. 2011; 54:1190-99. [ Links ]
18. Peters EJG, Lavery LA. Effectiveness of the diabetic foot risk classification system of the International Working Group on the Diabetic Foot. Diabetes Care. 2001; 24(8):1442-47. [ Links ]
19. Bower VM, Hobbs M. Validation of the basic foot screening checklist. A population screening tool for identifying foot ulcer risk in people with diabetes mellitus. J Am Podiatr Med Assoc. 2009; 99(4): 339-47. [ Links ]
20. Ndip A, Lavery LA, LaFontaine J, Rutter MK, Vardhan A, Vileikyte L , et al. High levels of foot ulceration and amputation risk in a multiracial cohort of diabetic patient on dialysis therapy. Diabetes Care. 2010; 33(4):878-80. [ Links ]
21. Leese GP, Freid F, Green V, Mcalpine R, Cunningham S, Emslie-Smith AM, et al. Stratification of foot ulcer risk in patient with diabetes: a population-based study. Int J Clin Pract. 2006; 60(5):541-45. [ Links ]
22. Wylie RJ, Walker EA, Shamoon H, Engel S, Basch C, Zybert P. Assessment of documented foot examinations for patients with diabetes in inner-city primary care clinics. Arch Fam Med. 1995; 4(1):46-50. [ Links ]
23. Edelson GW, Armstrong DG, Lavery LA, Caicco G. The acutely infected diabetic foot is not adequately evaluated in an inpatient setting. Arch Intern Med. 1996; 156(20): 2373-78. [ Links ]
24. Lavery LA, Hunt NA, LaFontaine J, Baxter CL, Ndip A, Boulton AJM. Diabetic foot prevention. A neglected opportunity in high-risk patients. Diabetes Care. 2010;33(7):1460-62. [ Links ]











 text in
text in