Introduction
According to figures from the World Health Organization published in 2012, preterm births represent 11.1% of all live births globally and large differences exist between countries according to their level of development, with Colombia reporting 8.8%.1 Prematurity brings along a high risk of early and late mortality and morbidity2 that demands specialized care within a neonatal unit. The continuity of care at home once the infant is discharged home is of great concern to the health staff, given that proper care is needed to ensure the wellbeing and adequate development of premature infants. It has been identified that after hospital discharge of premature children, a series of events take place in the home that can impact negatively on the child’s wellbeing.3-6 Therefore, discharge from the neonatal unit is an important process that involves, among other aspects, evaluation of the parents’ skills to care for their premature infant. It has been found that inexperience and lack of skills to care for premature child at home are related to a higher number of readmissions7 and to feeding difficulties, one of the most common problems in preterm infants after discharge.8) The hospital discharge of premature infants is thereby a critical event for the parents who requires close accompaniment, where participation from nursing professionals is highly relevant.9,10 The care skills of the parents must be assessed so that they can be guided at the time of discharge to strengthen their trust and security in their care of their infant once they get home.11
Although health care staff have previously identified barriers and facilitators which have provided better understanding of the needs of parents of premature infants upon discharge;11 it is necessary to also learn about the parents’ experiences to better understand their needs and how they can be best accompanied during the discharge process. This work seeks to contribute to the generation of strategies to enhance the discharge preparation process for parents of premature infants, to reduce their stress and enhance their sense of security and trust upon their infant’s discharge from the neonatal unit. Through knowledge of the parents’ experience upon discharge, we also hope to impact positively on the quality of care of preterm infants once home.
Methods
A qualitative descriptive study was conducted; information was gathered between September and December 2014 at a level III complexity neonatal unit in the city of Medellín. Data were collected through semi-structured interviews. Parents were interviewed close to the moment of their infant’s discharge. Once the parents were informed of the possibility of discharge or upon confirmed discharge, they were informed of the study and its purpose. After voluntary decision and signing of the informed consent, the interview was scheduled with the parents. For parents whose children were discharged on the day of the interview, the corresponding administrative procedures were guaranteed and prioritized. The interview was only conducted when the parents were calm, had sufficient time, and were emotionally ready. A comfortable and quiet place within the unit was sought for the parents, where they could be close to their infants and the health staff, and be available to respond quickly if they were needed.
The interview inquired about their lived experience regarding discharge from the neonatal unit. The interviews were audi-recorded by the researchers, transcribed textually by experienced research assistants and then validated by the researchers, and - finally - analyzed as of the references from founded theory.12 The number of interviews was determined by data saturation,13 that is when in the analysis of the interviews new data or relationships did not emerge among the categories. A total of 10 interviews were carried out, each lasting approximately one hour; only one interview was conducted with each parent (mother or father). The interviews were conducted by the researchers, who are nurses with diverse expertise in qualitative research and experience in neonatal care, who applied in full the ethical criteria required for the study.
Ethical principles corresponding to health research were adhered to. To that effect, the study was approved by the institutional ethics committees. Participants were asked to sign the written informed consent and were guaranteed confidentiality and anonymity. They were informed that they could withdraw from the study and stop the interview if they so desired without any prejudice against them or their infant An exploratory phase was carried out to allow refining of the interview guide, the approach to the study site, and rapport with the unit staff in order to enhance their collaboration and to better understand the dynamics and norms in the neonatal unit.
Data was analyzed with grounded theory12 as reference; open and axial coding was performed until the categories were arrive at: feelings experienced upon discharge and the experience of the discharge as a process. The methodological rigor of the research was based on criteria of confirmability, credibility, and auditability. Conversations were held with experts on the theme in other similar contexts. Likewise, the results were shared with the neonatal unit staff to validate them. Triangulation among the researchers was conducted throughout the analysis process, and was enriched by their diverse experiences; all have worked in different contexts and institutions, with different levels of experience in the area and from different schools of research.
Study participants were parents (mothers or fathers) who had a preterm infant hospitalized in the neonatal unit and who were near the time of discharge. The study excluded fathers and mothers with training in the health field. Nine mothers and one father participated in the study. Despite having only one father participant, his experience in relation to the aspects explored is congruent with the experiences of the mothers, hence, his data was included in the analysis. The youngest mother was 18 years of age at the moment of the interview and the eldest was 31 years old. Six of the participants had incomplete secondary studies, two had technical level education, and one was undertaking university studies. The most common occupation among the participants was domestic work; the participating father, who did not finish secondary education, worked as a field hand and/or construction and did not report formal employment. Three mothers were employees (drug store manager, executive secretary, industrial sewing machine operator), and one of them was a student. Only one of the participants did not report belonging to any religion; one was Christian, and the remaining participants were catholic.
Four of the participants were primiparous; one gave birth to twins; three had a previous child, and one had three other children including a previous preterm infant. Two mothers had no support from the fathers of their infant and the rest reported having support. In all cases, the participants had support from at least one relative. In general, study participants had low socioeconomic level. The number of days of hospital stay of the newborns were variable, thus, the shortest hospital stay was three days and the longest was four months. Length of stay was directly related to weight at birth, with the lowest at 790 g and the highest at 2 440 g.
Results
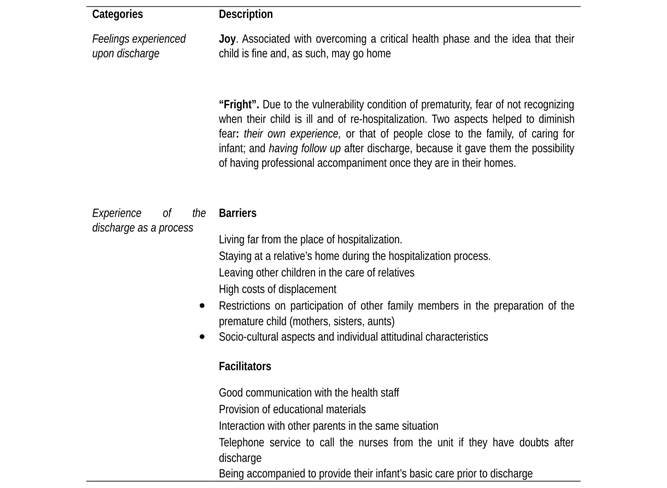
From analyzing the information obtained from each of the interviews, substantive codes were identified and grouped to form the following emerging categories: feelings experienced upon discharge, and experience of the discharge as a process; the latter category clearly identified barriers and facilitators.
Feelings experienced upon discharge
When asking the parents about their experience upon discharge, their feelings initially emerged as an aspect that influenced their experience. The feelings expressed by the participating parents were ambivalent, in general, denoting feelings of joy but in turn, some feelings of fear regarding the care and fragility of their infant. Joy mixed with the fear of caring for their premature child at home. The parents stated feeling “happy” and, in general, that was the feeling preceding the expression of other emotions. Feeling “happy” for the participants was related with relief and the joy that their child’s critical health stage had been overcome; going home was for them evidence that their child was well: it will be lots of joy because they give you your child in good health… (P4); because he was discharged, which means he is well… (P1).
In general, the participating parents experienced other feelings besides feeling happy, such as concern and fright, attributed to the fragility of the infants due to their condition of prematurity: Scared… too much responsibility, what if I drop him, they are like glass, oh no! What horror! They are very fragile (P2). “Fright”, understood in this context as an expression associated with fear, originated from the awareness parents have upon discharge that prematurity makes their children more vulnerable. The “fright” that parents say they felt upon discharge had to do with the possibility of their child getting sick, given that the prematurity increases health risks compared to other infants born at full term: “Scared… because he is preterm, because he might get sick” (P1). This possibility also scared them because it may imply returning to the hospital and a readmission for another hospital stay, a situation not desired by any of them.
Given the possibility of their infant getting ill, there was the added concern of not being able to recognize early signs and symptoms that may suggest illness. In contrast with the environment in the neonatal unit, where children are cared by the health staff and have clinical monitoring, the home confronts parents with the fear of not recognizing an illness in their child, given that they will not have equipment to monitor their infant or support from the health staff. One aspect that helped parents to minimize their fear is experience in caring for other children. The mother who had four children and prior experience caring for a preterm infant expressed tranquility at discharge: I am already used to dealing with my children, so nothing worries me... (P4). This expected, important role of experience was reinforced by participants who expressed that, even though they did not feel totally confident for care at home, once there they will receive support from others who have experience in caring for small children. This element helped minimize their fears: my uncle’s wife, she also has children, so that will help me a lot (P1).
Trust in one’s ability to provide basic infant care such as bathing, feeding, and changing diapers depended, to a large extent, on experience acquired through practice. Having previously performed these caregiving skills gave the parents greater security upon discharge. This point related to the participation in care that the nursing staff assigned to the parents during the hospitalization and their involvement with caring for their infant before returning home. In addition, upon discharge, the parents felt “relief” at the possibility of receiving follow-up care. The participants stated that they had been informed that their infant will be included in the “kangaroo plan”, which is a program which provides close and continuous follow-up of preterm infants. The families attend consultations within the plan; in this setting the infants are evaluated and the families are guided according to any identified needs. The participants, although unaware of this program untill discharge, saw in it a possibility of accompaniment, during which they can have issues solved, validate their care, and have specialists evaluate their infant’s state of health. In their experience as parents of preterm children, knowing that they will have access to monitoring programs after discharge gave them trust and security. This mitigated their fear, which was one of the principal feelings experienced by parents in the discharge process.
The experience of the discharge as a process
Although the hospital discharge for the participating parents was a special moment giving rise to emotions and feelings, parents recognized it as a process as they stated that they have been preparing for the discharge. Within the preparation process, they identified the need to learn a series of tasks in order to care for their premature child at home. During the discharge preparation process, the parents indicated that the staff taught them aspects related to caring for their children, highlighting basic care skills, like breastfeeding, changing diapers, and bathing their child. I have been taught to feed him, bathe him, and change him, and also that the child must be supported… (P3). In regards to how they were taught, the mothers and the father stated that they were first shown how to do things and then they had to perform the task while being evaluated on how they were doing things: yes, they have you bathe and change the infant (P4), I watched them bathe two babies and then I bathed mine, the nurse watched me do it (P7).
This category confirms that parental bonding was promoted through supervised direct care within the unit, as a strategy to prepare for care at home. The experience of providing direct care was identified by the parents as a helpful element to obtain greater trust and diminish fears upon discharge. With respect to who taught them how to care for their children once home, the participants viewed nursing assistants as the first line of preparation, however, they unified the nursing staff by not distinguishing nurses with different level of training or functions. Those who distinguished between levels of nursing viewed the primary work of professional nurses to be communication: they also kept each other informed, even when one arrives in the morning, they reported on what had occurred, or what tests had been run and for what reason (P6). The role of the medical staff was to provide information with respect to more critical health issues, and to ask whether parents have received adequate training prior to the discharge. Yesterday, the physician who was here spoke to me, he asked me about caring for my child… I told him that I’ve had babies with low birth weight, and he said, then there is no problem I will discharge the child tomorrow if you already know about that (P4).
At this point, it is possible to establish that the parents identified the participation of all members of the health care team in their process of preparing to care for their children at home, with different team members playing interrelated and complementary functions. In addition, the parents described barriers and facilitators to the process of preparing to care for their children at home.
Barriers
Socioeconomic difficulties were described as barriers to the preparation process for hospital discharge. Coming from far away, staying with relatives, being away from their familiar surroundings, having to leave their other children in the care of relatives or others, places a high emotional burden on the mothers and diverts their attention: … I cried practically day and night thinking of my children back home. It wasn’t so much for my baby, but for the others I had back home (P4). The economic difficulties of the parents was an obstacle to continuous accompaniment of their infants in the NICU and, hence, the teaching opportunities for care at home were limited. The economic support from close friends or relatives became a factor that facilitated the preparation for hospital discharge: So, you get collaboration from some people to get money for travel expenses or to get something to eat because sometimes you go hungry here all day and having even if it is only something to drink, thank God my family has helped me (P1).
The parents expressed that is was easier for maternal participation, as fathers had limited presence and little participation in the discharge process because of work, as they were the economic providers for the families . …my husband did come on weekends, on Saturdays when he left work early, and Sundays were sacred for him to come and kangaroo her (P6). The one father who participated in the study was able to be present during the whole hospitalization process and upon discharge because he was unemployed at the moment of the child’s hospital admission and had economic support from his family.
All the participants also identified as a barrier to the hospital discharge preparation process, restriction from participation of other significant members of the family who would support home care: For example, in my case, my mom will continue caring for my baby, she should have been aware of the care the baby needs. I would have liked that, now I have to talk to her about the education I received (P6). Other difficulties expressed by some of the mothers were associated with personal and attitudinal factors, which limited their interaction and the asking of questions: I am shy, I haven’t asked! Yes, I haven’t asked either because I imagine that if I ask obviously they will answer, sometimes one is somewhat shy (P1). This finding demonstrates that attitudinal, personal, and cultural characteristics interfere in the process and must be considered upon discharge in order know the parents’ reality and ensure understanding of the guidance given for care at home. Likewise, empathy and an atmosphere of trust are fundamental for parents to openly express their fears.
Facilitators
The mothers and the father who participated in the study, expressed good communications with the staff as a facilitator of the discharge preparation process. …I felt it was all fine, they were very nice and everything, very kind to deal with, they are not bad tempered. They are very patient, they take care of you and everyone (P3). Another facilitator for the mothers and the father interviewed was the educational material distributed, mainly that having to do with warning signs and written information on caring for their children at home: …they gave me a booklet that had to do with the warning signs and those for which we shouldn’t be worried, so clearly, when you read this you understand more about the child (P4). Regarding support groups, the mothers and the father interviewed described that space for interaction with other parents helped give them perspective on their own situation and allowed them to talk about their lives, which was positive for them: we would talk a lot, most of all about our families, about the families and their issues, about my issues. I got along well with those mothers. Super well (P8).
Another aspect identified as a facilitator for discharge preparation was the opportunity for telephone contacts with the unit nurses after discharge, which offered the mothers and the father interviewed the possibility of receiving reassurance for their doubts when needed. That placed them at ease when leaving the unit, becoming a form of support for them when faced with caring for their children in their homes: she told me: if anything, call us right away, they gave me the phone number in case something came up I could call them to get explanations, so I felt more secure, I felt I could call them for them to explain things about the baby (P1). Table 1 presents a summary of the categories that account for the experiences lived by the parents participating in the study:
Discussion
Parents experience a series of emotions and feelings during the discharge of their preterm children. The first category that emerged in the study had to do with feelings at the time of discharge. Participants expressed feelings of joy, given that they were waiting for the moment when they would go home with their child; yet all commonly felt fear due to the vulnerability associated with their child’s prematurity. This finding is consistent with other studies12,15,16 which also report that parents perceive a preterm child has having a higher risk of being ill and thus require special care, generating fear upon discharge. Parents distinguish between caring for a full-term versus and a preterm infant and express that prematurity makes them fragile and dependent on special and different care, a finding also described in other studies with similar populations and purposes.17
Clarification and understanding of this perceived greater vulnerability associated with prematurity can guide the nursing staff and the health team in charge of caring and preparing parents for discharge, as this can lead the parents to more effective care. Other aspects that must be considered during the hospital discharge process, according to the study participants, relate to the parents’ attitudinal and cultural factors, which can limit communication and understanding of the guidelines for care of their infants at home. It is necessary to assess the personality and specific needs of the parents.11,18 Regarding fathers, the participants expressed a scarce presence during the hospitalization of the preterm infant due to work responsibilities, as father have the role of economic provider and family support. These results are consistent with previous studies in which the fathers are attributed with the traditional function of supporting the family, which limits their participation in the discharge preparation process and leads health professionals to focus on the mothers.18,19 In addition, it reinforces the mother’s role as principal caregiver that prevails in our culture.
A main point of interest in this study is the role of experience and practice. According to the parents, caring for their infant prior to the discharge increases the level of sufficiency or competence for care at home. Parents understand that the more they provide direct care for their infant in the neonatal unit and have greater contact with them, the more confidence they will have to care for the infant at home. The value of practice or experience for effective care of preterm children at home has been described in similar studies.20,21 Through their experiences, parents describe the discharge as a process, characterized by education from the health staff on a series of necessary skills to care for their infant at home. This finding establishes that for parents the hospital discharge is a process and not a single moment isolated from the hospitalization experience. In this sense, participants identified some barriers and facilitators related to the discharge process. The following were considered barriers: living far away from the hospital; having to live with relatives during their infant’s hospitalization; having to leave their other children in the care of family in order to care for their hospitalized infant; the high costs of displacement; restrictions on the participation of other family members in the preparation of the premature child (mothers, sisters, aunts); and socio-cultural aspects and individual attitudinal characteristics.
On the other hand, family accompaniment, the option of calling the staff at the unit in case of doubts, and having a follow-up service such as the kangaroo plan were highlighted as facilitators. These, according to participants, gave them confidence that they will receive support once they leave the neonatal unit. This type of accompaniment offered to the parents, once they leave the hospital, is an element of great importance for parents of preterm children.22
The findings reinforce the importance of establishing institutional monitoring programs that facilitate the transition to home. It has been found in the literature that these types of programs impact positively on the number of readmissions and on parent satisfaction.23) Similarly, it is important to make efforts to involve family members and other potential caretakers at home, such as grandmothers and aunts. in the discharge preparation process,24,25 thereby enhancing quality of care at home by other caretakers. The results obtained provide direction for strengthening the preparation process for caring of preterm infants at home, which impacts upon the experiences of parents upon discharge, upon their emotions and feelings, as well as on their trust and security in caring for their children. In conclusion, participants experience during discharge from the neonatal unit a moment that blends feelings of joy and fear associated with their children’s condition of prematurity. From the parents’ experiences, participation in caring for their children while in the unit allowed them to feel better prepared for care at home, which is why it is quite important to promote participation by parents in caring for their children from the start of the hospitalization process and once the preterm infant’s health condition permits. Lastly, the hospital discharge is a process with barriers and facilitators that the nursing staff and health care team must value and recognize within the framework of the diverse social and cultural contexts from which the parents and families come.











 text in
text in