Introduction
Nosocomial Infections (NIs) are considered as one of the most important problems of health centers around the world, especially in developing countries. They have been associated with consequences such as increased length of hospitalization and increased health care costs(1) and are considered a threat as they increase the spread of infection in the community.(2) A reduction in NIs incidence can help retrieve patient health and improve economic efficiency.(3) These infections are a major cause of mortality and increased complications among hospitalized patients. Reports show two million NIs resulting in 19 000 deaths among patients and each year.(4) According to the World Health Organization, 7.1 million cases of NIs occur annually and 1 out of every 20 people is infected in hospital leading to the death of 99 thousand people and imposing about 32-26 million dollars on societies.(5) Studies in the East Mediterranean and Southeast Asian regions showed that 11.8 percent of hospitalized patients were affected by NIs.(6) The main objective is to reduce the risk of acquiring NIs by patients, hospital staff, and patients’ companions, and preventing transmission of infection by hospital staff and the patients' companions. Nurses play a crucial role in the control and prevention of NIs because they have the highest contribution to the treatment and care of the patient.(7)
Nurses can take appropriate measures in this regard such as disinfecting the skin, wearing gloves and masks, changing infusion sets, using caution measures, separating patients, using standard precautions, observing hand hygiene, preventing inadvertent contact with the needle sticks, avoiding exposure to infected respiratory secretions, and applying the principles of infection prevention in hospitalized patients.(8) Findings by Ghadamgahi et al.(3) suggest that many nurses do not have enough knowledge about controlling NIs. Therefore, continuous education is needed to raise nurses’ awareness about NIs that can help reduce such infections.(9) Any training program designed to improve performance of nurses with the purpose of reducing NIs would be counterproductive without their awareness about their own practices and attitudes towards NIs control.(10) In order to achieve this goal, it will be necessary to identify factors influencing behavior.
Researchers use behavioral models to identify factors associated with behavior.(11) Theories can guide the performance of health educators and can be used during various stages of planning, implementation, and evaluation of a program.(12) Since the 1950s to the present, the Health Belief Model (HBM) has been widely used as a conceptual framework in studies related to health behavior to explain change or maintenance of health-related behaviors and also to guide the interventions related to health behaviors.(13) According to this model, a person adopts preventive health behavior under the influence of factors such as perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action and efficacy.(14) In this model, perceived susceptibility, i.e. attitudes regarding their vulnerability and exposure to the risk of acquiring NIs, as well as Perceived severity, i.e. attitude about the severity and complications of NIs, are measured. The sum of these two factors is the nurses’ perceived threat of NIs. Besides perceived threat, the perceived benefits and barriers, i.e. the analysis of the benefits of adopting preventive behaviors against NIs, analysis of potential barriers to appropriate preventive measures, and nurses’ perceived capabilities for doing preventive behaviors; as well as cues to action, i.e. doctors and health workers, educational materials, and television and radio, help guide nurses to preventive practices against NIs. Zeigheimat showed the effectiveness of health belief model-based education on healthcare behaviors of nursing staff in controlling NIs.(15) Since preventing NIs is a global priority and training members of the health team, especially nurses, can play a significant role in the prevention and control of NIs, this study aimed to determine the effect of education based on Health Belief Model on promoting nurses’ preventive behaviors about NIs.
Methods
This randomized controlled trial study was conducted on 120 nurses working in Vali-e-Asr hospital, Fasa City, Fars (Iran) in 2016. Sample size was estimated based on a previous study by Zigheimat et al. (15) in the intervention group, the mean and standard deviation of practice before and after the study were 37.88 ± 5.78 and 41.9 ± 5.42 in the study groups. Then, based on the mentioned study and considering β = 0.90, α = 0.05, S1 = 5.78, S2 = 5.42, μ1 = 37.88, and μ2 = 41.9, 55 the number a subjects were estimated to be needed in each group. Therefore 60 subjects were recruited in each group to compensate the possible attrition.
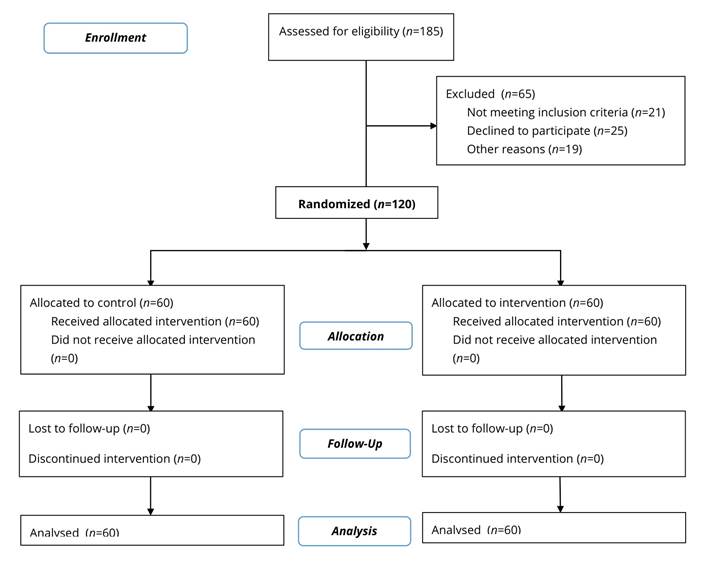
After obtaining written consent from the university authorities, the researcher obtained the consent of hospital officials as well. Random allocation of the intervention method was used to select 120 nurses who were assigned to intervention (n=60) and control groups (n=60). Figure 1 presents the study flow diagram.
At the beginning of the study, one of the researchers introduced himself to the participants and explained the objectives of the study for them. The pre-test questionnaire was administered to both groups. Inclusion criteria were: having at least a diploma in nursing, consent to participate in the study, and work experience for at least three months in the ward. Exclusion criteria encompassed refusing to continue participation in the study and lack of cooperation due to illness and leave.
Educational intervention for the intervention group consisted of eight training sessions of 55-60 minutes including lecture, group discussion, questions and answers, as well as posters, pamphlets, videos, and PowerPoint presentations. Focus of the sessions were: first and second: introduction to NIs and symptoms and complications of infections; third and fourth: the principles of proper sterilization of hands, use of gloves and masks, isolation of patients, hand hygiene, hospital waste disposal, and prevention of contact with contaminated respiratory secretions; fifth and sixth: benefits and barriers to the use of standard precautions; seventh: the role of the self-efficacy, standard precautions, and adoption of preventive behaviors against NIs were discussed; and, eighth: the past materials were reviewed, and some manuals were distributed among the participants, and educational resources were introduced to them. Training sessions were held in the hospital’s conference room and were planned in a way that did not interfere with their schedules. Immediately after the intervention, both intervention and control groups completed the questionnaire. To protect and promote the efforts of individuals in the intervention group, a training SMS (Short Message Sevice) about NIs was sent to each participant in the intervention group on a weekly basis. They also participated in a monthly training session held for retraining and follow-up activities. Four months later, both groups (intervention and control) completed the questionnaire.
The questionnaire was developed based on Health Belief Model and included: Knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, performance checklist, and demographic information. The performance of nurses regarding the adoption of preventive behaviors against NIs based on standard precautions was examined. The questionnaire was developed based on other studies and sources,(3,8,15) the Iranian National Nosocomial Infections Surveillance (NNIS), and also a survey of 15 experienced professors and faculty members in the field. In this regard, the panel of experts was asked to evaluate the clarity, simplicity, and relatedness of all items. Based on their comments, come items were excluded and some were modified. The content validity of the instrument was confirmed and the CVI was 85 percent for susceptibility, 87 percent for perceived severity, 81 percent for perceived benefits, 81 percent for perceived barriers, 89 percent for cues to action, 84 percent for perceived self-efficacy, and 92 percent for performance. The reliability of the questionnaire was also measured and the Cronbach's alpha coefficient was higher than 7.0 in all areas of the questionnaire. The high internal consistency of constructs was also confirmed (perceived susceptibility = 0.82, perceived severity =0.78, perceived benefits =0.8, perceived barriers = 0.79, perceived self-efficacy = 0.81, cues to action =0.83, and performance =0.84).Test-retest method was used to examine the reliability for stability of the instrument. To this end, first, the questionnaire was administered twice to 10 subjects with a 10-day interval. Then, the correlation between the two sets of test scores was calculated the Intra class Correlation Coefficient (ICC) = 0.80 for perceived susceptibility, ICC=0.75 perceived severity, ICC=0.82 for perceived benefits, ICC=0.81 for perceived barriers, ICC=0.82 for cues to action, ICC=0.80 for perceived self-efficacy, and ICC=0.83 for performance.
Besides the HBM constructs, the questionnaire collected demographic data on age, sex, education, work history, and workplace of subjects. The items included: 10 items on awareness (True=1 and False=0); 5 items on perceived susceptibility, 5 items on perceived severity, 5 items on perceived self-efficacy, 5 items on perceived benefits, 5 items on perceived barriers, and 5 items on cues to action (a five-point Likert scale from strongly agree to strongly disagree). The performance checklist included 17 items (Yes=1 and No=0, for a total score of 0-17).
For ethical considerations, the approval of the Fasa University of Medical Sciences and the consent of all nurses participating in the study were obtained. The participants were assured that their information would remain confidential. After the study, some educational booklets on preventive behaviors against NIs were distributed among the nurses.The collected data were coded and analyzed via SPSS version 22 using Chi-square, independent samples t-test, Mann-Whitney, Wilcoxon, and Repeated Measures ANOVA at a significance level of 0.5.
Results
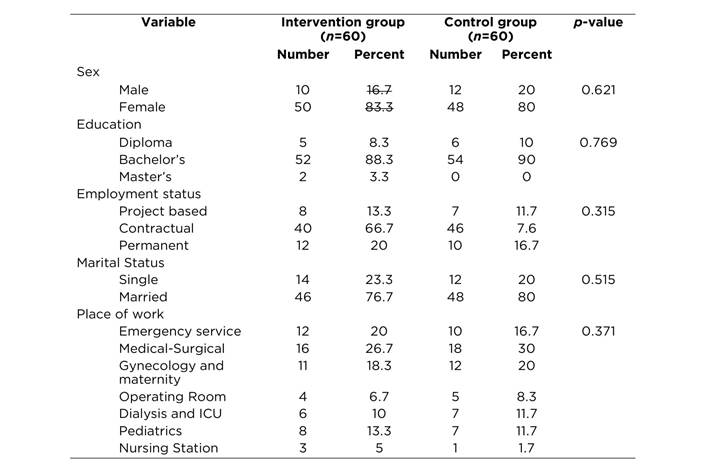
The mean age of subjects was 27.8±5.5 in the intervention group and 28.12±5.3 years in the control group. The mean work experience period was 10.1±5.2 years in the intervention group and 9.9±5.6 years in the control group. The independent t-test showed no significant difference between the two groups. Table 1 shows the demographic data including sex, education level, employment status, marital status, and place of work. The predominant charachteristics of the groups were: married women, with Bachelor’s education, with contractual employment, and they work principally in emergency and medical-surgical services. Based on chi-square test there was no significant difference between the two groups.
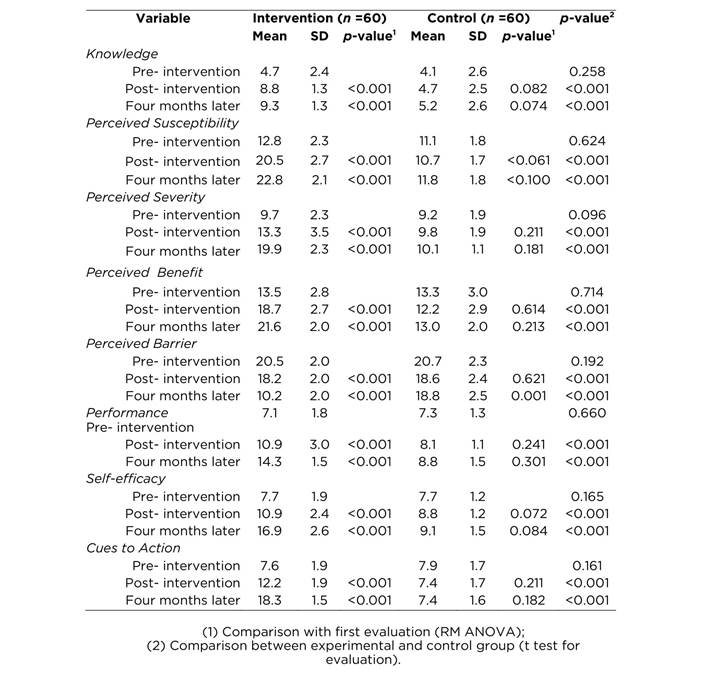
The results showed no significant differences between the intervention and control groups before the intervention in terms of level of knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, performance and cues to action. However, immediately after the intervention and four months after the intervention, the intervention group showed a significant improvement compared to the control group in each of these areas except perceived barriers. The perceived barriers component significantly decreased for the intervention group compared to the control group (compare the difference between the mean score of the groups) (Table 2).
Discussion
Reducing incompliance with hygiene guidelines is considered as the end goal of health education. The Health Belief Model used in this study as the theoretical framework, is an applied model, which has been widely used by various scholars for planning and evaluating interventions aimed at behavior change.(16) The results of the present study, which was carried out to evaluate the effect of HBM-based education on nurses’ preventive behaviors against NIs, confirm the efficiency of this model in changing the nurses’ behavior. The findings showed a significant increase in nurses’ awareness four months after the educational intervention, while no significant change was observed in control group in this area. This finding of this study is consistent with the results of other studies, such as Zigheimat,(15) Suchitra,(17) and Ghaffari.(18)
In a study conducted in India by Sabane(19) on 108 nursing students, the subjects’ awareness increased significantly after the intervention. The increase in intervention group’s awareness after educational intervention shows the effects of the training sessions on the nurses. Training and awareness raising are among the most effective methods of combating NIs. Obviously, continuous awareness alongside effective methods of disinfection and sterilization can decrease infections. The mean scores of the intervention group on perceived susceptibility and perceived severity (perceived threat) after educational intervention showed a significant increase compared to before the intervention, but did not change in the control group. Zigheimat’s study showed that in order to strengthen the health beliefs of nurses, one of the fundamental steps would be to create a sense of vulnerability to NIs among them.(15) The results of this study are consistent with theory-based studies by Gorman et al.(20) and Tehrani et al.(21) Health Belief Model is a useful model to interpret communities’ responses to infectious disease.(22) Highlighting the severity of a condition (disease) in the community can cause people to see themselves at a higher risk and probably to take a series of health-related measures. The results of this study showed that the intervention group’s scores on the perceived benefits in the post-test increased significantly compared to the control group, but their score on the perceived barriers decreased. Since the nursing staff are at a risk due to the nature of their job, which requires dealing with patients and doing risky behaviors, one of the fundamental steps in order to create a positive attitude among them and strengthen their health beliefs is to create a sense of being vulnerable to such infections among them and to highlight the benefits of such an attitude for nurses and the reduced costs for patients and hospitals. In addition, the nurses’ perceived barriers should be reduced by regular interventions. Zigheimat et al. found that the perceived benefits of nurses increased after the educational intervention, but their perceived barriers declined.(15) Noruzi et al.(23) showed that the perceived benefits of nurses were mostly about their own and their families’ health interests as well as the treatment of the patients. Shalanski’s study(24) showed that perceived barriers were the most important obstacle for adopting new behaviors.
Ghadamgahi et al.(3) and Ghanbari et al.(25) evaluated the perceived benefits and perceived barriers of nurses and found that they were at an acceptable level. The results of this study showed that the self-efficacy of nurses in the intervention group enhanced after educational interventions. Pike recommended that self-efficacy could be used in the clinical environment for stimulating and motivating nursing students for professional development.(26) In another study, self-efficacy was mentioned as an important factor in academic nursing education.(27) Results of the study by Zigheimat et al.(15) showed an increase in self-efficacy of nurses in the intervention group in controlling NIs after educational intervention compared to the control group. The results of this study in this regard are consistent with other studies.(21,28,29) The mean score of the intervention group on cues to action showed a significant increase after educational intervention compared to the control group. Zigheimat et al.(15) also found that cues to action mean score increased after educational intervention. In studies by Masood Hussain(30) and Boyce(31) training seminars were found to be the most important cues to action. Ghanbari(25) found that workshops were the most important cues to action.(25) Jeihooni et al.(32) found an increase in the mean scores on cues to action after the educational intervention.
In this study, the mean score of the intervention group on preventive behaviors against NIs increased after the intervention. In the same line, Suchitra et al.(17) concluded in their study that education had a positive impact on performance of health care workers regarding NIs. They also pointed to the need to develop a system of continuing education for health care workers (17). Zigheimat et al.(15) suggested that nurses’ performance in controlling NIs increased after the intervention in the intervention group compared to the control group. Studies by Kaewchana(33) and Fazrzan(34) showed that training improved the subjects’ hand washing performance. Javaheri Tehrani(21) showed that training based on HBM enhanced women’s performance regarding the urinary tract infection.
The results of this study show the effectiveness of the intervention program and the need for educational interventions on preventive behaviors against NIs. As a result of the HBM-based education, the intervention group’s scores on the components improved significantly leading to better NIs preventive behaviors. Given the importance of NIs, the need for fundamental solutions and proper planning to prevent them is felt. Educational programs for nurses, doctors and other health care personnel as well as educational programs on radio and television are essential. Therefore, educational interventions should improve the perceived susceptibility and severity of people about compliance with NIs control standards. Analyzing the benefits associated with infection control standards, removing barriers, and increasing self-efficacy and cues to action among nurses can help them change their behavior in controlling NIs. Periodic and in-service training should also be held for nurses based on the HBM and other health training and promotion models. One of the limitations of this study was self-reporting of performance on NIs control by nurses.
Acknowledgments: This study is part of the approved projects by Research Council of Fasa University of Medical Sciences under number 93218. The researchers appreciate the Research Deputy of Fasa University of Medical Sciences as well as nurses, who participated in this study.