Introduction
Pressure lesions (PL) are adverse events that emerge as consequence of a condition or chronic or acute state of health and can be related with the daily care of patients at risk.1 The definition of PL has been standardized by the National Pressure Ulcer Advisory Panel (NPUAP) and the National Group for the Study and Advisory on Pressure Ulcers and Chronic Wounds (GNEAUPP, for the term in Spanish)2 as a “localized damage on the skin and/or underlying soft tissue generally over an osseous prominence or related with a medical device or another, which can be painful”, bearing in mind the factors associated to the appearance of PL.2 These predisposing factors include age,3 nutritional status, urinary or fecal incontinence, alteration in tissue perfusion (e.g., in patients with cardiovascular problems, or hemodynamic alteration)4 and certain comorbidities (e.g.,, anemia, immobility due to neurological alteration).4 Additionally, increased pressure, friction and shearing, especially on osseous prominences, are determinants of the appearance of lesions.5,6
The incidence and prevalence rates of PL in patients hospitalized and which have been described in the literature have broad ranges of variation.6-8 An example of this are the data reported from a survey applied to hospitals to explore the incidence and prevalence rate of PL in the United States in 2006 - 2007. The results showed 4.5% incidence (n=2313/51842), and 16.7% prevalence (n=502/2999) during the hospital stay.6 Similarly, a wide range of variation exists between the data of incidence and prevalence among themselves. For example, the literature has reported variable rates of incidence of 7%7 and 71%;8 and, likewise, prevalence rates described varying between 8.8%9 and 53.2%.10 In Colombia, prevalence was evidenced at 2.21%, obtained from a national survey of hospitals in Bogotá, Yopal, and Valledupar conducted in 2013,11 reported by caregivers in the hospitals, without evaluating the validity of the information. Although the incidence and prevalence rates may vary depending on several factors, among these the hospital, care practices, and the health condition, thus, the existence of an adequate evaluation of the events and an adequate process of their validation is also important.
One of the factors that can explain the variation in the report of events (incidence and prevalence) in research studies may be due to the limitations in the blind validation of the lesions and of their degree of complexity.12 Given that reporting these lesions is a quality indicator in health services throughout the world, the assessment of PL must follow a methodology that certifies their presence or absence (given that they may be one or another type of lesion) and defines the degree of complexity of the lesion.13 The identification of the incidence rate and prevalence of PL permits establishing the level of risk in each hospital, while promoting the development of improvement plans in hospitals requiring them. These improvement plans include developing preventive care programs, which can lead to the reduction of the events and of the complications associated with the appearance of PL.14 Some clinical practice guides and global consensus of skincare have established a system to assess and qualify PL, but deficiencies have not been overcome in the knowledge about the appropriate methods to validate said events.14,15 Although the practice of assessing PL is carried out by the nurses who provide direct care, the validation of the existence of the ulcer (confirmation of the lesion) and validation of the classification of its degree must be conducted by a quality team.14 Precision on the definition of a PL is a component of optimal nursing care. It is possible that some lesions are classified erroneously as PL, producing an overestimation of the incidence; or on the contrary that they are not recognized as such, reducing artificially the incidence, losing the opportunity of healing according to a plan of adequate care.14 Limitations in care and in research related with the appearance of PL are related with the lack of a process that validates the events (PL yes; PL No) and the degree of the lesion, bearing in mind the existence of a guide that defines the degrees of the lesions.14
Using the photographic record to evaluate the evidence of events in health has been used in identifying PL,12,16 but its implementation and standardized use accompanied by a methodological plan to validate the reproducibility of the events has presented methodological limitations.12,16 The aim of this study was to evaluate inter-observer agreement among experts in identifying PL and the degree of lesions in adult patients hospitalized with risk of PL, using photographic records. Likewise, agreement was assessed between expert evaluators and the record and degree of PL described in the nursing registry in the electronic clinical record.
Methods
Study design
An observational study of agreement was conducted on a sample of photographic records of patients included in the study “Prevention in Nursing of Pressure Ulcers” (PENFUP, for the term in Spanish) (clinicaltrials.gov/ NCT02565745).
Study population
The study universe comprised 6474 photographic records of 600 patients included in the PENFUP project between October 2016 and June 2017. “Prevention in Nursing of Pressure Ulcers” is a randomized, controlled, blind, simple clinical trial on patients ≥18 years, with high or very high risk according to the BRADEN scale, whose objective was to evaluate the impact of applying skin protectors (Intervention) compared with the application of moisturizing cream (Control) upon the appearance of pressure ulcers in patients hospitalized due to medical/surgical reasons with healthy skin. Evaluation of the events of the PENFUP study was carried out through photographic records on admission (healthy areas of risk) and upon discharge from the study (with or without lesion). The patients were included according to the anatomic position at which they had more exposure during hospitalization (SIMS, PRONE, SUPINE). The photographs were taken of the areas at risk according to each position (SIMS 6 areas, PRONE 10 areas, SUPINE 11 areas).
Sample
The sample was made up of 225 photographic records, corresponding to 184 patients from the PENFUP study, selected through a simple random sampling. Pressure lesions were identified in 97 photographic records and in the 128 remaining there were no findings.
Procedure
Position and areas at risk
All the patients in PENFUP study, independent of the group to which they were assigned (Intervention/Control), had photographs taken of the zones of higher risk of lesion according to the position and the side in which the patient would spend the greatest time during hospitalization. In patients in supine position, photographs were taken of 11 areas (scapulae, elbows, sacrum, malleolus, heels, trochanters); in patients assigned to prone position, photographs were taken of 10 areas (forehead, chin, cheekbones, ribcages, iliac crests, knees), and in patients assigned to Sims position (left lateral or right lateral), photographs were taken of 6 areas (Pinna, ribcage, trochanter, elbow, knee, and malleolus). The photographic records to be evaluated by the adjudicators of events (two evaluators who were experts on management and treatment of PL and the most expert taken as a “gold standard”) were sent in packages of 50 equal pairs of photographic records to each evaluator separately. These evaluators were blind to the patient’s intervention (Hydrocolloid dressings/Moisturizing cream) and the evaluators did not know each other. To give their verdict, they were sent the photograph from the start of the study (healthy skin) and the photograph to be evaluated (state of the skin on discharge from the study).
Taking of photographs
Training was offered on the specialized technique of photographs to the staff of professional nurses in charge of taking the photographic records. Special care was taken to cover the genitalia, breasts, areas with tattoos, and faces of the participants, according to that agreed in the informed consent, as well as institutional logos, and the procedures were standardized through the elaboration of a manual on taking of photographs to reduce the variability and bias in each image registered. The same photographic camera model was used in both centers, NIKON COOLPIX L330 with 20.2 megapixels with means of storage and SD, SDHC or SDXC memory card. The distance to take the photograph could not be greater than 45 cm, and perpendicular to the area of interest to register, according to the positioning of the patients. If it was decubitus, the patient was rotated to the left or right turning the back to the camera to take the record. If the patient was to spend most of the time possible in prone position, the patient was left in decubitus supine position to take the photographic records of the zones of interest. The lighting depended on each service; in patients hospitalized in ICU, each unit had LED lighting and no flash or any other type of light was used when taking the photograph. To adapt the lighting of patients hospitalized in ward, the curtains were drawn to avoid day light and bright lights to avoid altering the brightness or contrast of the image, preferably using light tone background (sheets from the ICU and the hospitalization wards), grays or blacks and using the camera in automatic or manual setting and without effects. The moment of taking the photographic record was done after the patient’s bath with the skin clean and dry, and several shots were taken to select the image with the best quality, corresponding to each body site.
All the photographs were stored in a common file of the PENFUP study through DROPBOX™ with a blind code. Additionally, the images were included in a registry reading base to then be attached to an evaluation format that was sent (via Gmail or in USB memory) to the evaluators with the photographs before the intervention and the photographs to be evaluated after removing the intervention (upon discharge from the study). The evaluation format only had the information from the blind code. Lastly, from the PENFUP study, broadened information was obtained of each patient related with the general variables, bearing in mind demographic aspects, health antecedents, admission diagnosis, and in-hospital care and complications.
Selection of the expert evaluators
Three evaluators were selected to classify the photographs. Two of them through an initial adjudication assessment using historical photographic records of PL and a third evaluator was included through merit and expertise to improve the quality of the evaluation and solve disagreements. For the initial standardization of two evaluators, 50 pairs of photos were selected (50 healthy and 50 with pressure ulcer) by an expert and 50 photographs were randomly distributed (with and without PL) to each of the evaluators on two moments to revise them in masked manner. The Kappa index of inter-observer reproducibility between the two evaluators was 0.82 (EE 0.07, CI95%: 0.70 - 0.96) for the first pair of 50 photos and 0.76 (EE 0.07, CI95%: 0.62 - 0.89) for the second pair of 50 photos. With these results (good and very good Kappa) these two evaluators were accepted. The three evaluators did not know each other, and conducted the evaluation independently.
Follow up of patients and identification of lesion
During the development of the PENFUP study, follow up was conducted of all the patients after the initial session of photographs, directly on the seventh day and then every day during their hospital stay through the clinical record. Once a registry of a lesion appeared, verbally or in the clinical record, a photograph was taken of the zona of lesion. The clinical records were revised by a nurse in each investigation center. The REHCE revised on the presence and degree of PL, the date of detection of the event, area, and degree of the lesion.
Criteria to evaluate the photographs
The evaluators knew the categories for the classification of the ulcers according to the EPUAP and NPUAP1 to standardize the evaluation of the PL. The totality of the photographs (with and without PL) was sent to each evaluator in blind manner in a different sequence, in groups of 50 and only a package of 25 at the end, for their reading. Each evaluator had two weeks to conduct the reading and had to fill out a format for each photographic record in which the evaluator defined the presence of PL (Yes, No); and classified the degree of the lesion according to the depth of the lesion in category (I: presence of erythema that does not pale on intact skin, this lesion indicates that a patient is at risk; II: partial loss of the skin that affects the epidermis, dermis or both; it was classified as a superficial ulcer with an aspect of abrasion, blister, or superficial crater; III: there is total or complete loss of the skin thickness that implies lesion or necrosis of the subcutaneous tissue, which can extend down but not through the underlying fascia; IV: total loss of thickness of the subcutaneous tissue with extensive destruction, necrosis of the tissue, or lesion in muscle, bone, or support structure). We included a zero (0) category to denominate the absence of PL.1
Study variables
i) Result variables. Proportion and degree of Kappa agreement among the three evaluators on the presence and category of the PL. The proportion and degree of Kappa agreement was also evaluated between the REHCE and the presence or absence of PL and category assigned according to the evaluators, and
ii) Descriptive variables of the patients. Demographic variables were included (age, gender, schooling, occupation), health antecedents (comorbidities), and variables relating the diagnosis on admission. Additionally, complications and days of hospital stay were included.
Data analysis
The characteristics of the population included upon hospital discharge, including demographic variables and comorbidities. Qualitative variables were analyzed in proportions and quantitative variables were analyzed in summary measures, like the arithmetic mean, according to its nature and level of measurement. The qualitative agreement of the presence of PL (dichotomous variable) was evaluated in the photographs analyzed by using the Kappa index, through the fit of the random effect in the proportion of the agreement observed and interpreted, thus: poor or weak ≤0.40, moderate: 0.41-0.60, good: 0.61-0.80, and very good: 0.81-1.17 The inter-evaluator agreement was compared with the expert evaluator (E3 denominated gold standard) to conform the composite agreement for each of the evaluations.18
Ethical considerations
This study was approved by the institutional ethics committee in the centers of the PENFUP study based on resolution 8430 of 1993 by the Ministry of Health. All the participants or their relatives accepted the taking of photographs of the zones at risk on admission and discharge from the study, with prior signed informed consent.
Results
This study included 184 patients, mostly men with a mean age of 61±18.2 years (minimum age = 20 and maximum age = 92); 46.7% of the patients included worked independently and 72.8% with some level of basic schooling. Among the comorbidities observed, those with the highest frequency were neurological and endocrine. The most frequent cause of admission to the hospital center was neurological alteration (14.7%) and the most common hospital collection service was that of medical hospitalization (77.2%). The individuals had on average 2.3 medical devices, like nasal cannula, vesical catheter, nasogastric catheter, mechanical ventilation, indicating a critical state of health that required support of vital functions. The median of days of hospitalization was 13.5 days (Q1=7, Q3=25, minimum=2 and maximum=154), and 52.2% had very high risk, according to the BRADEN scale. Complications during hospitalization in highest proportion were sepsis (42.9%), bleeding (23.9%) pneumonia (21.7%) and death (14.7%). Of the 97 PL included in the study, the experts identified 32 in the sacrum, 16 in scapulae, 15 in heels, 14 in trochanters, and 20 in other places (Table 1).
Table 1 General characteristics of 184 patients with high or very high risk of developing PL
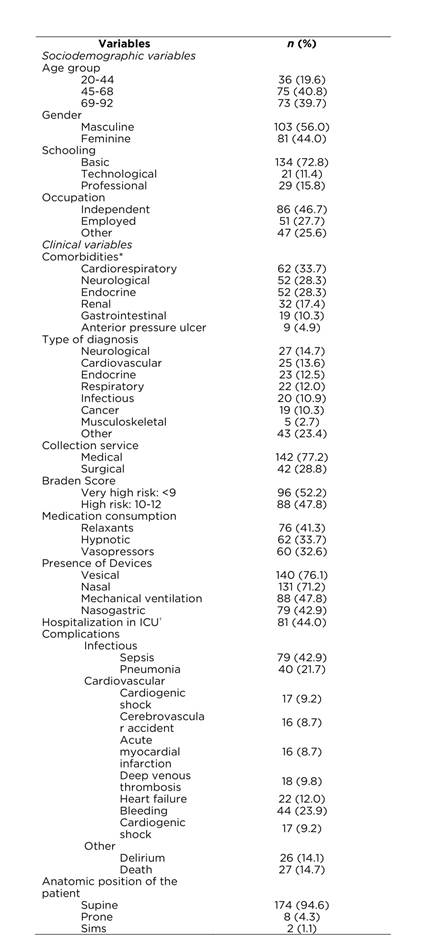
(*) A patient may have more than one comorbidity; (*) Intensive Care Unit
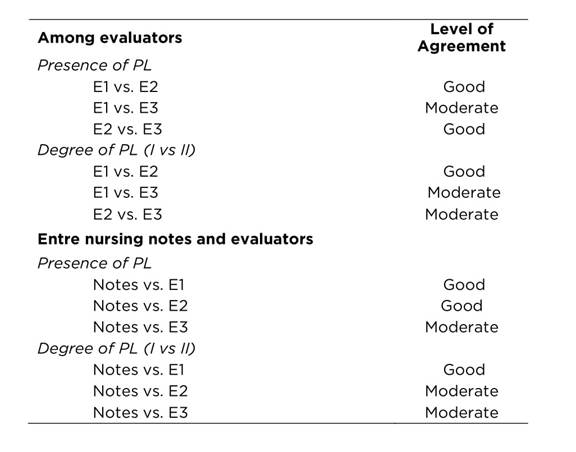
No PL degree III or degree IV were identified in the assessment by the experts, or in the registries of the clinical records. Table 2 displays that the evaluation of the agreement of the presence or not of PL was statistically significant in the photographic records among the three evaluators, presenting “good” agreement between evaluators 1 and 2, between evaluators 2 and 3 and moderate agreement between evaluators 1 and 3. Assessment of the agreement among the three evaluators for the degrees of PL include three categories (without PL 0, PL degree I, PL degree II). Good agreement was observed between evaluators 1 and 2 and moderate agreement between evaluators 1 and 3 and between evaluators 2 and 3.
Table 2 Agreement among experts and between nursing notes and experts on the presence and degree of PL
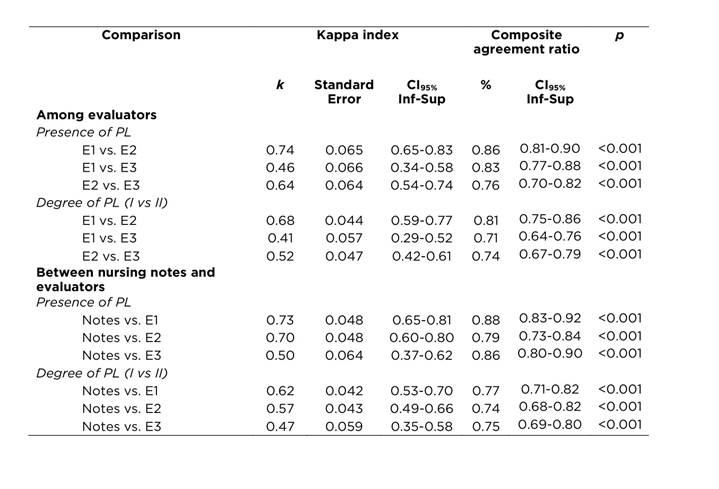
Table 2 details the evaluation of agreement of the presence or not of PL among that observed among the three evaluators of photographic records and the REHCE by nursing presented the following findings, all significant: good agreement between REHCE and evaluator 1 and good agreement between REHCE and evaluator 3; and moderate agreement between REHCE and evaluator 2. Assessment of the agreement of the degree of PL between REHCE and the evaluators identified good agreement between REHCE and evaluator 1, moderate between REHCE and evaluator 2 and between REHCE and evaluator 3.
This study showed moderate agreement between evaluators E1 and E3 and good agreement among the expert evaluators of photographic records for the existence of a PL and moderate agreement for E1 and E2 versus the expert, while the agreement among those not so expert (E1 and E2) is good in the degree of the lesion. Similarly, good agreement was observed to determine the presence of lesion and moderate for its degrees among the nursing registries and the three expert evaluators (Table 3).
Discussion
This study recalls the importance of using photographic records of the skin in patients admitted to hospitalization services with healthy skin but with high risk for developing PL, as key element in the validation of the lesions.12 This type of evaluation through photographic records permits blind adjudication of events, quite important in investigation. These photographic records can be used by institutional quality groups and provide greater precision to the adjudication of the events of obligatory report to the Ministry of Health and Social Protection, like the case of pressure lesions. Photographic records, when evaluated by several experts, can reduce variation in the definition of PL, as well as their degree17,18 and permit the comparison and adjudication of final events, especially in research projects. The existence of an adequate and permanent training plan of the professional direct caregivers, as conducted in these centers that participated in the PENFUP study, shows minor variation among the registries by the nursing staff and the external evaluators.
Given that greater difference exists in the agreement on the types of PL, more emphasis should be made on training in identification or discrimination of the degree of PL in care groups.20 The precise definition of the degree of the ulcers is directly related with the type of treatment required to prevent progress of the lesion (degree I) or its healing. A periodic evaluation by experts using photographic records could improve quality of care and the precise use of resources in hospitals or outpatient care groups. This type of record can be used for remote expert assessment; this becomes a resource to help caregivers in remote regions of the country with greater needs in the orientation of caring for PL.19,20
In conclusion, identification, definition, and classification of PL is a task that is still not performed systematically in our hospitals and we still have much to learn. Certainty in the definition of whether a skin lesion is a PL or not, and what is the degree of complexity are the base to enhance preventive care plans and structure adequate treatment for each type of lesion. Adequate classification of lesions in each hospital permits valid reporting to quality regulation entities from the Ministry of Health and Social Protection and, thus, better assessment of the quality of health care in our hospitals.











 text in
text in