Introduction
Non-alcoholic fatty liver disease (NAFLD) is one of the common liver diseases, a chronic disease associated with lifestyles with no physical activity and inappropriate nutritional habits.1,2 This disease is characterized by the deposition of triglycerides as fat droplets in the cytoplasm of liver cells. In this case, liver fat content is defined higher than 5.5%.1 NAFLD has a broad spectrum, while its severity varies from simple steatosis to non-alcoholic steatohepatitis, if it is not treated effectively, can lead to advanced cirrhosis and even liver cancer.2 In various studies, risk factors, the relationship between unhealthy nutritional habits, reduced physical activity and the occurrence of the disease has been proven.3 In fact, unhealthy nutritional habits along with inadequate physical activities have led to the prevalence of obesity and diabetes, blood lipid disorders, blood pressure, and metabolic syndrome. Consequently this has exposed large number of population to the risk of NAFLD.4,3 According to an ever increasing report of unhealthy nutritional habits caused by lifestyle and reduced physical activity, as well as an increase in the prevalence of obesity, the prevalence of NAFLD in the community is on the rise.3 The prevalence of this disease in the eastern countries is estimated to be about 16-30% amongst the general population, which is comparable with the western countries. In Iran, the prevalence of fatty liver is estimated to be around 32.8% detected by ultrasound.1
Diagnostic methods for this disease include biopsy, ultrasonography, CT scan, MRI, and blood tests. At present, liver biopsy is a gold standard to diagnose NAFLD, but due to invasive nature of this method it cannot be used for the population-based studies. Ultrasonography is a non-invasive diagnostic method for detecting non-alcoholic fatty liver disease, which is used more than other methods, since it is readily available and cheaper than the other graphical instruments while it is highly reliable.5 There are currently two strategies to treat NAFLD including lifestyle interventions (including weight loss, diet and physical activity), and/or drug therapy.6 Weight loss and lifestyle changes along with diet and increasing physical activity is usually recommended as the first step in treating this disease.2
In this regard, studying the effect of low calorie diet on patients with non-alcoholic fatty liver revealed a significant reduction in weight, liver enzymes (ALT and AST), and significant improvement in their ultrasound results.7 In another study, the effects of 15 months of diet and exercise were evaluated, with an emphasis on weight loss, while a significant reduction in weight, liver enzymes and improvement in quality of life were observed.8 One of the most important causes of treatment failure and lack of favorable response to prescribed treatment is undesirable follow through of the treatment by the patients. (9 Effective follow up is considered as an essential part of care services. Repeated interventions and regular follow-ups seems necessary to promote healthy behavior.10 One of the follow-up method is tele-nursing.9 Tele-nursing is defined as the use of telecommunication technology to promote patient care.10 Tele-nursing increases the relationship between the nurse and patients that leads to provision of patient care without time and place considerations, while it can also improve healthcare and reduce health costs.11
A number of studies verified the effect of nursing follow-up through phone by achieving the specified objectives.9-11 In this regard, telenursing effects on glycemic control and BMI of patients with type 2 diabetes were examined, which determined that telenursing was capable of improving patients’ metabolic indices.12 Another research that had investigated the effect of telenursing on complying to diet in patients with type 2 diabetes, the results showed that telenursing led to enhancement of patients obedience to diet with type 2 diabetes.13 NAFLD can be controlled and treated during its primary stages; however, if it is not diagnosed and treated on time, it will progresses, leading to undesirable complications. Hence it can be prevented by informing the patients about the course of the disease, appropriate training in from of weight loss, adherence to diet and increasing physical activity, and through follow-up.10 Since to this point no study has been conducted in Iran, we aimed to investigate the effect of follow-up on dietary control and increased physical activity via phone on ultrasound findings of patients with NAFLD.
Methods
This randomized controlled clinical trial study was conducted from May 2013 to Dec 2016. The local ethics committee of Shiraz University of Medical Sciences approved this study with (Ethics committee code CT-92-92-62-6602), and registered in the Iranian Registry of Clinical Trials ( IRCTcode: IRCT2015040411691N5). Based on the results from previous studies, 60 patients with NAFLD who had referred to subspecialty gastroenterology clinics affiliated to Shiraz University of Medical Sciences were enrolled in this study.14,15 NAFLD was confirmed by an expert physician using ultrasound and laboratory tests. The inclusion criteria of the study were anyone who was 19 years or older, being overweight or obese (Body Mass Index (BMI) > 25 kg/m2), having the ability to do moderate physical exercise, having a telephone at home or a mobile phone, and not having any speech or hearing problems. The exclusion criteria were having any history of chronic liver diseases, such as viral or drug hepatitis, confirmed Wilson disease, primary hemochromatosis, suffering from hyperthyroidism or hypothyroidism, bile duct cancer, diabetes mellitus, obesity due to excessive use of corticosteroid, Cushing’s syndrome, Addison syndrome, and chronic infections, such as tuberculosis, use of hepatotoxic drugs within the past 6 months, incidence of gall stones in the gallbladder, having been exposed to petrochemicals, alcohol consumption, drug abuse, and genetic diseases related to lipid disorders.
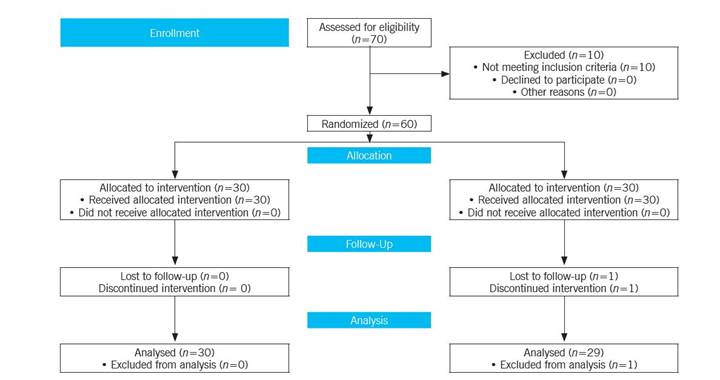
After obtaining written informed consents, simple randomization based on the table of random numbers was used to allocate patients to intervention (n=30) or control (n=30) groups. It should be noted that one participant in the control group was excluded due to lack of cooperation. In doing so, based on the suggestion of the statistician, numbers 0-4 were assigned to the control group and numbers 5-9 to the intervention group. At first, the researcher explained the nature of the disease, factors contributing to the disease, progression and prognosis, complications of the disease, and the importance of treatment and follow-up. Then, the researcher asked the participants to complete the demographic information form.
Before the intervention, to diagnose and evaluate the state of disease and parenchyma tissue and liver size, all participants were referred to specialized ultrasound center affiliated to Shiraz University of Medical Sciences. After ultrasound, patients were divided into 4 groups including normal (grade 0), mild steatosis (grade 1), moderate steatosis (grade 2), severe steatosis (grade 3) according to their liver echo condition. Grading the disease based on the size and condition of the liver echo and its histological comparison with the adjacent kidneys, as well as comparison with the spleen echo and the shape of the diaphragm and the periphery of the liver internal vessels. Patient's liver was assessed by an ultrasound specialist using the Medison ultrasound machine (SA8000 model made in Germany).
In this study, a nutritionist was hired to offer consultation at a nutritional counseling center affiliated to Shiraz University of Medical Sciences. The participants received a written dietary recommendation. Then, they were asked to perform moderate physical activities at least 30 minutes a day 4-5 times a week to raise their heart rate and respiration. Jogging, cycling, aerobic exercises or any other activities with similar intensity were prescribed. In addition to one-on-one consultation, all the participants received a training booklet. It should be noted that specialist physicians, radiologists, nutrition counselors and patients were unaware of how the participants were assigned in the control and intervention group.
In the intervention group, the intervention lasted for 12 weeks to see if the participants followed up the recommended diet and physical activity. The participants were given self-report forms designed by the researcher to register their daily diets and physical activities. This allowed them to easily report the items during their follow-ups. The form included items of participant's adherence to diet and physical activities. In case a patient had not followed the diet and training program, the researcher tried to recognize and analyze the reasons and provide a possible solution. It should be noted that the conversations were recorded by the researcher during each session. The researcher contacted all the patients between 8 AM to 8 PM twice a week during the first month and once a week during the following months. On average, each conversation lasted for 15-20 minutes.16,17) The control group participants did not receive any interventions and were only followed up as usual by a specialist. It is worth mentioning that the control group participants received the educational booklet at the end of study. After 12 weeks, participants were referred to the same center for ultrasound for re-evaluate the size and condition of their liver parenchyma. Then, the data were entered into the SPSS statistical software (version 22) and were analyzed using chi-square test, paired t-test, and independent t-test.
Results
This study was performed on 60 patients (30 in each group). It should be noted that one participant in the control group was excluded due to lack of cooperation, so, at the end of the study, there were 30 participants in intervention group and 29 participants in control group.
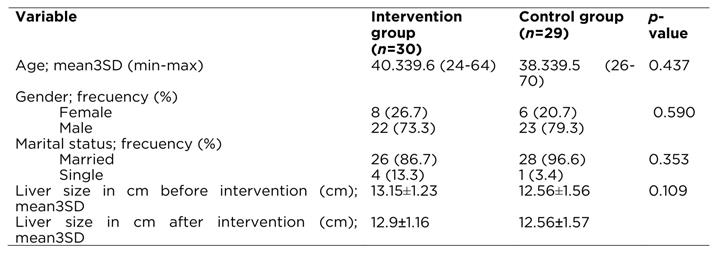
In Table 1 we can observe that in both groups was predominance of males, aged 38 - 40 years and married participants. The results of independent t-test showed no statistically significant difference between the groups for these demographic characteristics. In the same Table 1it is also reported that was no significant difference between the liver size before the intervention liver size of the studied groups before the intervention.
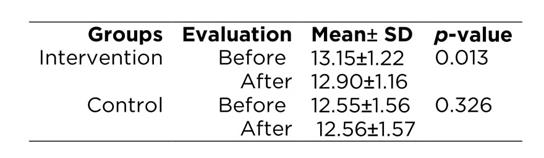
As it can be seen in Table 2, the mean liver size in the intervention group was reduced after intervention, but the liver size did not change significantly in the control group. Based on the paired t-test, these changes were statistically significant only in the intervention group.
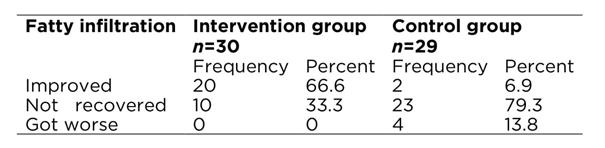
According to independent t-test, the greater difference in the mean liver size between the moments before was in the intervention group with 0.26±0.53cm versus -0.003±0.018cm cm in the control group (p=0.012). Table 3 shows that in terms of fatty infiltration status 66.6% of the intervention group versus 6.9% of the control group improved their status. According Fisher exact test the difference between the two groups was statistically significant (p<0.001).
Discussion
This study aimed to investigate the effect of tele-nursing on ultrasound findings of patients with NAFLD. It revealed that after 12 weeks of follow-up, the mean liver size decreased in the intervention group, but this index did not change in the control group. After the intervention, Changes were statistically significant only in the intervention group and the difference in mean liver size among the studied groups was statistically significant. Also, after the intervention, the fatty infiltration status of the liver tissue in the intervention group was better than the control group, and the differences between the two groups were statistically significant.
The results of this study are consistent with the results of the study by Hang et al.,18 on the compliance with the diet, especially the nutritional diet and physical activity. They had phone counseling with the patients after bone marrow transplantation, their results showed that patients in the follow-up group via phone followed the treatment regimen more, and there was a significant difference between the intervention and control groups. A study by Kamrani et al.9 was conducted with the aim to investigate the effect of patient training and following-up via phone by nurses on observing diet by patients with acute coronary syndrome, but they concluded that patient training and follow up via phone were both effective methods. However, the patients in the phone follow up group in comparison with the training group had better compliance with the dietary treatment.
In fact, all patients required to be trained and consulted continuously,19 because training patients and follow up is an effective way to change lifestyle and observation of treatment diets.9 Lack of treatment program observation is a therapeutic problem in chronic diseases,11 hence, continuous and regular follow up by nurses is highly important. Investigating the behavior and patients follow up when they are at home as well as follow up and control through renewing the trained issues can help to institutionalize the trained healthy behaviors. This in turn will reduced the frequency of referring to doctors and hospitalization, reduced economic burden, increased longevity, and reduced mortality.19 At the present, follow up at home via phone has become a popular method in managing chronic diseases.10
Follow up via phone is a very useful and inexpensive method to assess the patient requirements that can lead to reduced number of patient visits with to treatment teams.20 It also removes time and place barriers for nursing care. This care method will increase the positive results of the treatment, promotes nurse-patient communication that controls the health status of patients, as well as continuous nurse's encouragement increases patients autonomy, which encourages them to take care of themselves.21 For example, Baker et al.,22) found that the use of training programs, along with continuous phone follow up, led to increased awareness, promotion of healthy behavior and quality of life in patients with heart failure. Another study conducted by Shojaei et al.,23) on patients with heart failure revealed that educating patients who are being discharge and follow up via phone after discharge will reduce the re-admission of these patients to hospitals and doctors' offices. Anderson reported that patients' education by nurse, nutrition expert and social worker at the time of discharge by nurses through visiting their house or follow up via phone after discharge led to reduced readmissions in the intervention group in comparison with control group.24
However, the results of some studies are not line with the present study. A study by Beur et al.on patients with breast cancer stated that phone follow-up had no significant impact on treatment of patients who had no advanced breast cancer.25 The reason for ineffective results of call follow up in these patients might be due to the nature of the disease and its impact on the patient's ability to accept treatment. Another study by Wang et al. also showed the effect of home visits and call follow ups on the training after the discharge and re-admission of patients, but they concluded that call follow up alone might not be effective in reducing re-admission of patients, and it is necessary to simultaneously use different methods of training after discharge.26 Generally it can be stated that this type of counseling might lead to continuous and continuity of patient-health communication with the health system, and can also have a positive impact on all aspects of the health care and its outcomes, while it can highlight the effect of nurse in preventing and treating the chronic diseases by preventing the development of disability and complications caused by the disease.
As the results of this study show, tele-nursing improves liver size and liver histology state in patients with non-alcoholic fatty liver. It can be stated that tele-nursing promotes healthy behaviors by increasing patient's awareness. In fact, regular follow-up and telephone counseling services after clinical counseling can be a continuation and complementary trainings that can lead to the emergence of healthy behaviors in patients as well as improving the outcome of treatment. Further studies are recommended to investigate the effect telenursing on improving patient's health statues with NAFLD and other chronic illnesses. Conducting qualitative researches on this subject would be beneficial.