Introduction
Heart failure (HF) is part of the group of cardiovascular diseases. Defining this disease is complex, given that it involves different processes and its etiology is also varied, which is why it is referred to as a “syndrome”. Simply stated, it may be understood as “state in which the heart is not capable to pump the amount of blood necessary to fulfil the needs of the organism”.1) Moreover, due to its high morbidity and mortality figures,2,3 currently, HF is considered a public health problem, besides implying a high cost for governments and health systems. Evidence shows that the prevalence of HF increases gradually with age and it is estimated to affect 10% of elderly adults, becoming the first cause of hospitalization in this population.4)
In relation with the socioeconomic burden due to HF, some European and South American countries show high costs for health services;3,5,6 which has become a great concern for the governments and health institutions. Another one of the serious problems of HF is the increase of readmissions of patients due to the decompensation of the disease.4 Within this context, over time, specialized units have been created with programs of multidisciplinary approach for the integral management of patients with HF.3 Among these programs, education of patients is crucial to improve the clinical outcomes of patients. Health education is one of the professional roles of nursing. Nurses must have the ability to evaluate the patients’ individual needs for education and be able to improve their self-care practices that contribute to the reduction of readmissions.2) Educational interventions can vary in their intensity, methodology, or strategy. The effect sought with these interventions is to achieve a greater number of patients with HF aware of their disease and of the importance of self-care habits for their health. This, in turn, favors better control of the disease and reduction of the different complications and costs associated with HF.5,6
Due to the aforementioned, up-to-date syntheses are required of the literature that evidences the effect the educational interventions have on reducing readmissions due to decompensation of the HF syndrome. Although primary studies exist to address this problem, it is important to group systematically every evidence to permit greater comprehension of the phenomenon and generate new results that contribute to the recovery of individuals who endure this disease. Hence, the objective of this study was to estimate the combined effect of the educational interventions on reducing hospital readmissions and time of hospital stay in adults with HF, compared with usual care.
Methods
Design and registry of the protocol. This was a systematic review (SR) and meta-analysis (MA) of randomized controlled trials (RCTs) that followed the recommendations of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement 7 and of the Cochrane Handbook 8 for SR of intervention studies. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with code CRD42019139321.
Source of data and search strategy. The information was collected from the following electronic databases: PubMed/Medline, Embase, Lilacs, Cochrane CENTRAL, Scopus, and Web of Science. Searches were made from inception until July 2019, using MeSH terms and entry terms for PubMed/Medline, emtree terms for Embase and descriptors for the other databases. Likewise, the following filters were used for the search strategy: randomized controlled trials, studies in humans and English, Portuguese, Spanish languages. To identify additional studies, search was made in other sources that included the review of references of the studies included, SR published, and the network of primary registries of RCTs recognized by the World Health Organization.
The following search strategy was used for PubMed/Medline: ((Heart failure[MeSH Terms]) OR (Cardiac Failure)) OR (Heart Decompensation)) OR (Decompensation, Heart)) OR (Congestive heart failure)) OR (Heart Failure, Congestive)) )) AND (Knowledge[MeSH Terms])) AND (Self-care[MeSH Terms]))) OR (Care, Self)) OR (Self-care behaviors[MeSH Terms])) OR (Self-management[MeSH Terms])) OR (Management, Self)) OR (Self-efficacy[MeSH Terms])) OR (Efficacy, Self)) OR (Self Concept[MeSH Terms])) OR (Self-confidence)) OR (Confidence, Self)) AND (Education[MeSH Terms])) AND (Patient education[MeSH Terms]) ) ) OR (Education, Patient)) ) OR (Education of Patients) ) AND (Education, nursing [MeSH Terms])) ) OR (Nursing Education)) OR (Educations, Nursing)) OR (Nursing Educations)) AND (Health education[MeSH Terms])) OR (Education, Health)) AND (Standard of Care)
Eligibility criteria of the studies. This SR and MA included experimental studies or CCT-type intervention studies. The following PICO (population, intervention, comparator, outcomes) research question was used to consider the eligibility of the studies, P: adult patients with HF in any stage of the disease; I: educational interventions; C: usual or standard care, and O: reduced readmissions and time of hospital stay due to decompensation of the HF.
Data extraction. Identification and selection of the studies was performed independently by two reviewers, who were young undergraduate researchers with prior training and certification in SR and MA. Disagreements were solved through the intervention of a third reviewer, senior researcher with PhD formation and experience in SR and MA. Articles duplicated in several databases were considered only once. The Mendeley reference manager was used to store references and eliminate duplicate studies.
Outcomes. The principal outcome was the decrease of hospital readmissions due to decompensation of the HF and the secondary outcome was the decrease of days of hospital stay.
Evaluation of the risk of study bias. The risk of bias (RoB 1) tool from the Cochrane Collaboration 9 was used to evaluate the risk of bias in RCTs. The following parameters were evaluated: random sequence generation and allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting of results and other sources of bias.
Data analysis. Estimation of the grouped effect was conducted with the Review Manager (RevMan 5.4) software from the Cochrane Collaboration. The dichotomous results are presented and compared by using relative risk (RR) through the Mantel-Haenszel method and for continuous results the mean difference (MD) is presented through the inverse-variance weighted; both with their respective 95% confidence intervals (CI). Likewise, to quantify the heterogeneity of the studies included, the inconsistency (I2) statistic was used and the graphic presentation of the MA results used the forest plot. To evaluate publication bias or bias due to missing results, the Stata 16.0 software was used, through the Egger test and the funnel plot.
Results
Identification and selection of the studies
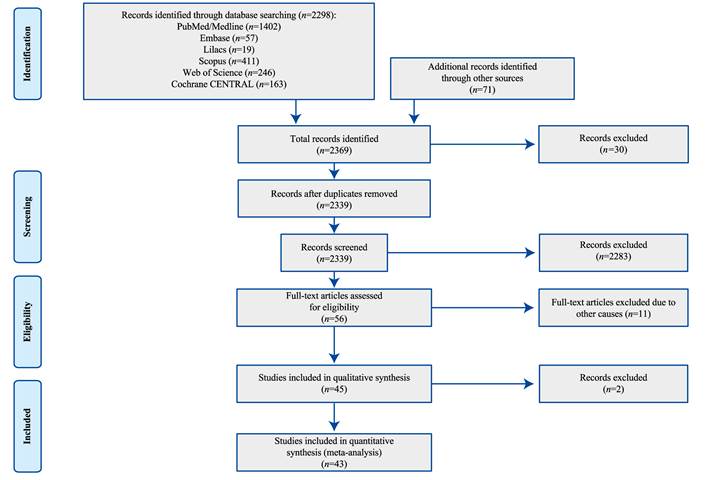
The work identified 2369 studies, of which 45 studies were included in the SR and data from 43 studies were included in the MA. Two studies were excluded from the MA because the data on readmissions corresponded to follow-up times different from the other studies and, hence, it was not possible to meta-analyze. The flow diagram for the selection and exclusion of studies is shown in Figure 1.
Characteristics of studies included
The general description of the studies is shown in Table 1, which contains the author, year of publication, country, a brief description of the intervention, time of follow-up, and most relevant results for the research.
Table 1 Characteristics of the included studies
| First author, year | Country | Sample size | Intervention group | Follow-up | Control group | Main outcomes |
|---|---|---|---|---|---|---|
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Readmissions* at 12 months |
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Intervention: 55 |
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Control: 57 |
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Days of hospital stay+ |
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Intervention: 8.5 (6.4) |
| Aldamiz-Echevarría et al., 2007 (10) | Spain | 279 | Educational program on basic data of HF and its treatment. | 3, 6 and 12 months | Standard care | Control: 8.4 (11.6) |
| Atienza et al., 2004 (11) | Spain | 338 | Education before discharge on knowledge of the disease and its management. Home visits. | 12 months | Standard care | Readmissions* at 12 months Intervention: 61 Control: 122 |
| Atienza et al., 2004 (11) | Spain | 338 | Education before discharge on knowledge of the disease and its management. Home visits. | 12 months | Standard care | Intervention: 61 |
| Atienza et al., 2004 (11) | Spain | 338 | Education before discharge on knowledge of the disease and its management. Home visits. | 12 months | Standard care | Control: 122 |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Readmissions* at 12 months |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Intervention: 12 |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Control: 26 |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Days of hospital stay+ |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Intervention: 3.43 (12.2) |
| Blue et al., 2001 (12) | Scotland | 165 | Education through home visits and telecare on knowledge and treatment of HF. Educational brochure. Instruments for self-monitoring. | 12 months | Standard care | Control: 7.46 (16.6) |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Readmissions* at 3 months |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Intervention: 8 |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Control: 10 |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Readmissions* at 12 months |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Intervention: 8 |
| Boyde et al., 2018 (13) | United States | 200 | Education prior to discharge on HF. Brochure and video. | 1, 3 and 12 months | Standard care | Control: 14 |
| Brian et al., 2009 (14) | United States | 749 | Education on HF. Brochure and telephone follow-up. | 1 month | Standard care | Readmissions* at 1 month |
| Brian et al., 2009 (14) | United States | 749 | Education on HF. Brochure and telephone follow-up. | 1 month | Standard care | Intervention: 55 |
| Brian et al., 2009 (14) | United States | 749 | Education on HF. Brochure and telephone follow-up. | 1 month | Standard care | Control:76 |
| Brotons et al., 2009 (15) | Spain | 283 | Pre-discharge education on HF with brochure. Home visits for one year. Phone follow-up every 15 days. | 12 months | Standard care | Readmissions* at 12 months |
| Brotons et al., 2009 (15) | Spain | 283 | Pre-discharge education on HF with brochure. Home visits for one year. Phone follow-up every 15 days. | 12 months | Standard care | Intervention: 52 |
| Brotons et al., 2009 (15) | Spain | 283 | Pre-discharge education on HF with brochure. Home visits for one year. Phone follow-up every 15 days. | 12 months | Standard care | Control: 62 |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Readmissions* at 2 months |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Intervention: 11 |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Control: 5 |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Days of hospital stay at 2 months |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Intervention: 6.27 (5.93) |
| Cañon-Montañez et al., 2013 (16) | Colombia | 116 | Education on HF and its management. Face to face and phone education. | 1 and 2 months | Standard care (phone call) | Control: 11 (11) |
| Cui et al., 2019 (17) | China | 96 | Structured education in HF for one hour upon admission, and one hour before discharge. Phone or face-to-face consultation every 4 weeks. | 12 months | Standard care | Readmissions* at 12 months |
| Cui et al., 2019 (17) | China | 96 | Structured education in HF for one hour upon admission, and one hour before discharge. Phone or face-to-face consultation every 4 weeks. | 12 months | Standard care | Intervention: 5 |
| Cui et al., 2019 (17) | China | 96 | Structured education in HF for one hour upon admission, and one hour before discharge. Phone or face-to-face consultation every 4 weeks. | 12 months | Standard care | Control: 13 |
| Davis et al., 2012 (18) | United States | 125 | Education during hospitalization. Phone call after discharge. Video with recorded sessions. Supplies to aid self-care. | 1 month | Standard care | Readmissions* at 1 month |
| Davis et al., 2012 (18) | United States | 125 | Education during hospitalization. Phone call after discharge. Video with recorded sessions. Supplies to aid self-care. | 1 month | Standard care | Intervention: 14 |
| Davis et al., 2012 (18) | United States | 125 | Education during hospitalization. Phone call after discharge. Video with recorded sessions. Supplies to aid self-care. | 1 month | Standard care | Control: 12 |
| De Souza et al., 2014 (19) | Brazil | 252 | Home visits to educate on HF. Phone calls to reinforce education. | 6 months | Standard care | Readmissions* at 6 months |
| De Souza et al., 2014 (19) | Brazil | 252 | Home visits to educate on HF. Phone calls to reinforce education. | 6 months | Standard care | Intervention: 20 |
| De Souza et al., 2014 (19) | Brazil | 252 | Home visits to educate on HF. Phone calls to reinforce education. | 6 months | Standard care | Control: 30 |
| DeBusk et al., 2004 (20) | United States | 462 | Education with a videotape. Telephone counseling and printed educational materials. | 12 months | Standard care | Readmissions* at 12 months |
| DeBusk et al., 2004 (20) | United States | 462 | Education with a videotape. Telephone counseling and printed educational materials. | 12 months | Standard care | Intervention: 76 |
| DeBusk et al., 2004 (20) | United States | 462 | Education with a videotape. Telephone counseling and printed educational materials. | 12 months | Standard care | Control: 86 |
| Delaney et al., 2013 (21) | United States | 100 | Telemonitoring. Brochure with information on HF and its management. | 3 months | Standard care | Readmissions* at 3 months |
| Delaney et al., 2013 (21) | United States | 100 | Telemonitoring. Brochure with information on HF and its management. | 3 months | Standard care | Intervention: 3 |
| Delaney et al., 2013 (21) | United States | 100 | Telemonitoring. Brochure with information on HF and its management. | 3 months | Standard care | Control: 7 |
| Dewalt et al., 2006 (22) | United States | 127 | Education on HF and warning signs. Phone calls for reinforcement of the education. Educational brochure. | 6 and 12 months | Standard care | Readmissions* at 12 months |
| Dewalt et al., 2006 (22) | United States | 127 | Education on HF and warning signs. Phone calls for reinforcement of the education. Educational brochure. | 6 and 12 months | Standard care | Intervention: 18 |
| Dewalt et al., 2006 (22) | United States | 127 | Education on HF and warning signs. Phone calls for reinforcement of the education. Educational brochure. | 6 and 12 months | Standard care | Control: 20 |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Readmissions* at 3 months |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Intervention: 20 |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Control: 23 |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Readmissions* at 12 months |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Intervention: 22 |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Control: 42 |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Days of hospital stay at 12 months+ |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Intervention: 4.1 (6.4) |
| Domingues et al., 2011 (23) | Brazil | 120 | Phone calls after hospital discharge to educate and evaluate signs of decompensation of HF. | 3 months | Standard care | Control: 7.6 (12.1) |
| Doughty et al., 2002 (24) | New Zealand | 197 | Educational brochure on HF and its management. Home visits. | 12 months | Standard care | Readmissions* at 12 months |
| Doughty et al., 2002 (24)- | New Zealand | 197 | Educational brochure on HF and its management. Home visits. | 12 months | Standard care | Intervention: 36 |
| Doughty et al., 2002 (24) | New Zealand | 197 | Educational brochure on HF and its management. Home visits. | 12 months | Standard care | Control: 65 |
| Dracup et al., 2014 (25) | United States | 614 | Face-to-face education session delivered by a nurse focusing on self-care. Phone calls. | 3, 12 and 24 months | Standard care | Readmissions* at 24 months |
| Dracup et al., 2014 (25) | United States | 614 | Face-to-face education session delivered by a nurse focusing on self-care. Phone calls. | 3, 12 and 24 months | Standard care | Intervention: 63 |
| Dracup et al., 2014 (25) | United States | 614 | Face-to-face education session delivered by a nurse focusing on self-care. Phone calls. | 3, 12 and 24 months | Standard care | Control: 64 |
| Ducharme et al., 2005 (26) | Canada | 230 | Visits to the HF clinic to provide education in the management of the disease. Phone calls every month. Educational brochure. | 6 months | Standard care | Readmissions* at 6 months |
| Ducharme et al., 2005 (26) | Canada | 230 | Visits to the HF clinic to provide education in the management of the disease. Phone calls every month. Educational brochure. | 6 months | Standard care | Intervention: 45 |
| Ducharme et al., 2005 (26) | Canada | 230 | Visits to the HF clinic to provide education in the management of the disease. Phone calls every month. Educational brochure. | 6 months | Standard care | Control: 66 |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Readmissions* at 12 months |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Intervention: 11 |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Control: 14 |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Days of hospital stay at 12 months+ |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Intervention: 6.7 (13.5) |
| Gámez-López et al., 2012 (27) | Spain | 208 | Follow-up in the HF clinic after discharge. Phone call after discharge to reinforce education. Home visit. | 12 months | Standard care | Control: 10.7 (22.2) |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Readmissions* at 12 months |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Intervention: 14 |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Control: 18 |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Days of hospital stay at 12 months+ |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Intervention: 16.8 (18.2) |
| González-Guerrero et al., 2014 (28) | Spain | 116 | Flyer with information about the disease. Follow-up call within 48 hours. Reinforcement of education after 10 days. Visits to the geriatric center to reinforce education. | 12 months | Standard care | Control: 20.6 (23.5) |
| Hägglund et al., 2015 (29) | Sweden | 72 | Educational sessions at home through a tablet about HF and its management. | 3 months | Standard care | Readmissions* at 3 months |
| Hägglund et al., 2015 (29) | Sweden | 72 | Educational sessions at home through a tablet about HF and its management. | 3 months | Standard care | Intervention: 7 |
| Hägglund et al., 2015 (29) | Sweden | 72 | Educational sessions at home through a tablet about HF and its management. | 3 months | Standard care | Control: 11 |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Readmissions* at 3 months |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Intervention: 12 |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Control: 9 |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Readmissions* at 6 months |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Intervention: 1 |
| Holland et al., 2007 (30) | United Kingdom | 399 | Home visit after discharge to educate on HF and its management. Follow-up visit to reinforce education. | 3 and 6 months | Standard care | Control: 1 |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Readmissions* at 3 months |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Intervention: 18 |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Control: 23 |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Days of hospital stay at 3 months+ |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Intervention: 3 (7) |
| Jaarsma et al., 1999 (31) | Netherlands | 174 | Education about HF, treatment and management during hospitalization. Phone call and home visit. | 1, 3 and 9 months | Standard care | Control: 4.1 (10) |
| Jaarsma et al., 2011 (32) | Netherlands | 1049 | Home visit after discharge and every 6 months to receive education on HF. Additional home visits (basic group). Monthly contact with the nurse, additional visits and telephone follow-up (intensive group). | 18 months | Standard care | Readmissions* at 18 months |
| Jaarsma et al., 2011 (32) | Netherlands | 1049 | Home visit after discharge and every 6 months to receive education on HF. Additional home visits (basic group). Monthly contact with the nurse, additional visits and telephone follow-up (intensive group). | 18 months | Standard care | Intervention: 134 |
| Jaarsma et al., 2011 (32) | Netherlands | 1049 | Home visit after discharge and every 6 months to receive education on HF. Additional home visits (basic group). Monthly contact with the nurse, additional visits and telephone follow-up (intensive group). | 18 months | Standard care | Control: 120 |
| Jerant et al., 2001 (33) | United States | 37 | Two home visits after discharge. Phone calls. Telecare. | 6 months | Standard care | Readmissions* at 6 months |
| Jerant et al., 2001 (33) | United States | 37 | Two home visits after discharge. Phone calls. Telecare. | 6 months | Standard care | Intervention: 1 |
| Jerant et al., 2001 (33) | United States | 37 | Two home visits after discharge. Phone calls. Telecare. | 6 months | Standard care | Control: 4 |
| Kato et al., 2016 (34) | Japan | 38 | Education and advice on knowledge about HF and self-care. | 24 months | Standard care | Readmissions* at 24 months |
| Kato et al., 2016 (34) | Japan | 38 | Education and advice on knowledge about HF and self-care. | 24 months | Standard care | Intervention: 2 |
| Kato et al., 2016 (34) | Japan | 38 | Education and advice on knowledge about HF and self-care. | 24 months | Standard care | Control: 7 |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Readmissions* at 3 months |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Intervention: 15 |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Control: 24 |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Days of hospital stay at months+ |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Intervention: 4.3 (10.2) |
| Kimmelstiel et al., 2004 (35) | United States | 200 | Home visit. Manual with information on HF. | 3 and 6 months | Standard care | Control: 7.8 (19.7) |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Readmissions* at 6 months |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Intervention: 16 |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Control: 33 |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Days of hospital stay at 6 months+ |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Intervention: 13.1 (36) |
| Koelling et al., 2005 (36) | United States | 223 | Education prior to discharge on the management of HF. Information brochure. Application of self-care questionnaires. | 1, 3 and 6 months | Standard care | Control: 17.1 (37) |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Readmissions* at 12 months |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Intervention: 22 |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Control: 42 |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Days of hospital stay at 12 months+ |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Intervention: 4.1 (6.4) |
| Krumholz et al., 2002 (37) | United States | 88 | Sequential education on HF and its management. Educational brochure. Home visits. Telemonitoring to reinforce education. | 12 months | Standard care | Control: 7.6 (12.1) |
| Leventhal et al., 2011 (38) | Switzerland | 42 | Home visit to provide HF education. Phone calls to reinforce education. Educational kit with self-care procedures. | 3, 6, 9 and 12 months | Standard care | Readmissions* at 12 months |
| Leventhal et al., 2011 (38) | Switzerland | 42 | Home visit to provide HF education. Phone calls to reinforce education. Educational kit with self-care procedures. | 3, 6, 9 and 12 months | Standard care | Intervention: 1 |
| Leventhal et al., 2011 (38) | Switzerland | 42 | Home visit to provide HF education. Phone calls to reinforce education. Educational kit with self-care procedures. | 3, 6, 9 and 12 months | Standard care | Control: 2 |
| Mau et al., 2017 (39) | United States | 150 | Educational modules on HF and its treatment. | 12 months | Standard care | Readmissions* at 12 months |
| Mau et al., 2017 (39) | United States | 150 | Educational modules on HF and its treatment. | 12 months | Standard care | Intervention: 5 |
| Mau et al., 2017 (39) | United States | 150 | Educational modules on HF and its treatment. | 12 months | Standard care | Control: 18 |
| Melin et al., 2018 (40) | Sweden | 72 | Education of self-care practices and management of HF. | 6 months | Standard care | Readmissions* at 6 months |
| Melin et al., 2018 (40) | Sweden | 72 | Education of self-care practices and management of HF. | 6 months | Standard care | Intervention: 14 |
| Melin et al., 2018 (40) | Sweden | 72 | Education of self-care practices and management of HF. | 6 months | Standard care | Control: 16 |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Readmissions* at 12 months |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Intervention: 40 |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Control: 72 |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Days of hospital stay at 12 months+ |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Intervention: 11.1 (7.2) |
| Naylor et al., 2004 (41) | United States | 239 | Daily education during the hospitalization period. Home visits to reinforce education about HF and its management. | 3, 6 and 12 months - 2, 6, 12, 26, 52 weeks | Standard care | Control: 14.5 (13.4) |
| Negarandeh et al., 2019 (42) | Iran | 80 | Telemonitoring with HF education. | 1 and 3 months | Standard care | Readmissions* at 3 months |
| Negarandeh et al., 2019 (42) | Iran | 80 | Telemonitoring with HF education. | 1 and 3 months | Standard care | Intervention: 7 |
| Negarandeh et al., 2019 (42) | Iran | 80 | Telemonitoring with HF education. | 1 and 3 months | Standard care | Control: 14 |
| Otsu et al., 2011 (43) | Japan | 102 | Educational program in HF clinic about the disease and its management. | 3, 6, 9 and 12 months | Standard care | Readmissions* at 6 months |
| Otsu et al., 2011 (43) | Japan | 102 | Educational program in HF clinic about the disease and its management. | 3, 6, 9 and 12 months | Standard care | Intervention: 1 |
| Otsu et al., 2011 (43) | Japan | 102 | Educational program in HF clinic about the disease and its management. | 3, 6, 9 and 12 months | Standard care | Control: 1 |
| Ramachandran et al., 2007 (44) | India | 50 | Education on HF, management and treatment. Reinforcement of education by phone calls. Patient education manual. Follow-up in the HF clinic. | 6 months | Standard care | Readmissions* at 6 months |
| Ramachandran et al., 2007 (44) | India | 50 | Education on HF, management and treatment. Reinforcement of education by phone calls. Patient education manual. Follow-up in the HF clinic. | 6 months | Standard care | Intervention: 6 |
| Ramachandran et al., 2007 (44) | India | 50 | Education on HF, management and treatment. Reinforcement of education by phone calls. Patient education manual. Follow-up in the HF clinic. | 6 months | Standard care | Control: 4 |
| Rodríguez-Gázquez et al., 2012 (45) | Colombia | 63 | Educational program in nursing (educational meetings, home visits, telenursing and a printed book) in the improvement of self-care behaviors. | 9 months | Standard care | Readmissions* at 9 months |
| Rodríguez-Gázquez et al., 2012 (45) | Colombia | 63 | Educational program in nursing (educational meetings, home visits, telenursing and a printed book) in the improvement of self-care behaviors. | 9 months | Standard care | Intervention: 30 |
| Rodríguez-Gázquez et al., 2012 (45) | Colombia | 63 | Educational program in nursing (educational meetings, home visits, telenursing and a printed book) in the improvement of self-care behaviors. | 9 months | Standard care | Control: 24 |
| Ruschel et al., 2018 (46) | Brazil | 252 | Home visits and phone calls. Education on HF and self-care practices. | 6 months | Standard care | Readmissions* at 6 months |
| Ruschel et al., 2018 (46) | Brazil | 252 | Home visits and phone calls. Education on HF and self-care practices. | 6 months | Standard care | Intervention: 30 |
| Ruschel et al., 2018 (46) | Brazil | 252 | Home visits and phone calls. Education on HF and self-care practices. | 6 months | Standard care | Control: 30 |
| Sethares et al., 2004 (47) | United States | 70 | Education about HF during hospitalization. Reinforcement education after discharge. | 3 months | Standard care | Readmissions* at 3 months |
| Sethares et al., 2004 (47) | United States | 70 | Education about HF during hospitalization. Reinforcement education after discharge. | 3 months | Standard care | Intervention: 6 |
| Sethares et al., 2004 (47) | United States | 70 | Education about HF during hospitalization. Reinforcement education after discharge. | 3 months | Standard care | Control: 12 |
| Stewart et al., 2015 (48) | Australia and New Zealand | 624 | Home visit after discharge. Education on HF and its management. Personalized care plan. | 1 and 36 months | Standard care | Readmissions* at 36 months |
| Stewart et al., 2015 (48) | Australia and New Zealand | 624 | Home visit after discharge. Education on HF and its management. Personalized care plan. | 1 and 36 months | Standard care | Intervention: 17 |
| Stewart et al., 2015 (48) | Australia and New Zealand | 624 | Home visit after discharge. Education on HF and its management. Personalized care plan. | 1 and 36 months | Standard care | Control: 17 |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Days of hospital stay at 6 months+ |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Intervention: 1 (2.45) |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Control: 0.84 (1.89) |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Days of hospital stay at 12 months+ |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Intervention: 1.23 (2.55) |
| Tomita et al., 2009 (49) | United States | 40 | Information online about HF and its management. | 6 and 12 months | Standard care | Control: 2.42 (5.07) |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Readmissions* at 6 months |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Intervention: 6 |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Control: 15 |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Readmissions* at 12 months |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Intervention: 6 |
| Tsuchihashi‐Makaya et al., 2013 (50) | Japan | 164 | Pre-discharge education on HF and its management. Educational brochure. Home visits once a week for two months. Monthly telephone follow-up for six months. | 2, 6 and 12 months | Standard care | Control: 9 |
| Wakefield et al., 2008 (51) | United States | 148 | Follow-up after discharge. Phone calls to provide HF education. | 3, 6 and 12 months | Standard care | Readmissions* at 12 months |
| Wakefield et al., 2008 (51) | United States | 148 | Follow-up after discharge. Phone calls to provide HF education. | 3, 6 and 12 months | Standard care | Intervention: 21 |
| Wakefield et al., 2008 (51) | United States | 148 | Follow-up after discharge. Phone calls to provide HF education. | 3, 6 and 12 months | Standard care | Control: 29 |
| Wierzchowiecki et al., 2006 (52) | Poland | 160 | Education and follow-up in the HF clinic. Phone calls for educational reinforcement. | 12 months | Standard care | Readmissions* at 12 months |
| Wierzchowiecki et al., 2006 (52) | Poland | 160 | Education and follow-up in the HF clinic. Phone calls for educational reinforcement. | 12 months | Standard care | Intervention: 13 |
| Wierzchowiecki et al., 2006 (52) | Poland | 160 | Education and follow-up in the HF clinic. Phone calls for educational reinforcement. | 12 months | Standard care | Control: 25 |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Readmissions* at 12 months |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Intervention: 46 |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Control: 18 |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Days of hospital stay at 12 months+ |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Intervention: 9.4 (13.6) |
| Wright et al., 2003 (53) | New Zealand | 197 | Clinical review after discharge. Home visits every 6 weeks to educate on HF, treatment and management. | 12 months | Standard care | Control: 14.9 (18.8) |
| Yu et al., 2015 (54) | China | 178 | Education before discharge about HF. Home visits and phone calls for educational reinforcement. | 6 weeks, 3 and 9 months | Standard care | Readmissions* at 6 weeks - 3 months - 9 months |
| Yu et al., 2015 (54) | China | 178 | Education before discharge about HF. Home visits and phone calls for educational reinforcement. | 6 weeks, 3 and 9 months | Standard care | Intervention: 7 - 12 - 6 |
| Yu et al., 2015 (54) | China | 178 | Education before discharge about HF. Home visits and phone calls for educational reinforcement. | 6 weeks, 3 and 9 months | Standard care | Control: 10 - 7 - 3 |
HF: heart failure; * Data presented as number of patients readmitted due to decompensation of HF; + Data presented as mean (standard deviation).
Table 1 shows that this SR included 9688 adult patients with HF. The studies were published between 1999 and 2019. The investigations were conducted in 16 countries, with the highest number of these in the United States and Spain (16 and 5, respectively). The follow-up of the studies included was carried out during different periods, comprised between the first month after the intervention and at 36 months. Studies with follow-up at 3, 6 and 12 months were predominant.
With respect to the educational interventions, these were diverse; however, common strategies were found in the studies included, like: education during hospitalization, telephone follow-up, home visits to reinforce the education, visits to HF clinics, and delivery of printed or digital educational material (brochures, videos or manuals) for consultation by the patients. The education centered on knowledge of the disease, warning signs, diet, and self-care practices.
Regarding the comparison with the control group, it was found that in general, the usual care was perceived as the clinical care by the cardiologist and a single control visit in the outpatient care service.
Analysis of the risk of bias of the studies included
The evaluation of the risk of bias of the studies is presented in Table 2. According with the parameters evaluated by the RoB 1 tool,9) it was obtained that all the studies performed an adequate random sequence generation; allocation concealment was optimal in 65.1% of the studies included. Due to the nature of the educational interventions, in the studies it was not possible to conduct blinding of the patients and of the staff who offered the interventions. In relation blinding of outcome assessment, only 48.8% low risk was presented for this domain. In all, 93% of the studies described clearly the losses presented during the follow-up and if the data analysis was carried out through intention of treatment, which reduced the risk of bias due to incomplete results. Finally, regarding the risk of selective reporting of the results, it was found that 97.7% described the results proposed since the beginning (Table 2).
Table 2 Assessment of risk of bias among included studies
| Studies | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Aldamiz-Echevarría et al., 2007 (10) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Atienza et al., 2004 (11) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Blue et al., 2001 (12) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Boyde et al., 2018 (13) | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Brian et al., 2009 (14) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Brotons et al., 2009 (15) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cañon-Montañez et al., 2013 (16) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cui et al., 2019 (17) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Davis et al., 2012 (18) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| De Souza et al., 2014 (19) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| DeBusk et al., 2004 (20) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Delaney et al., 2013 (21) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Dewalt et al., 2006 (22) | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Domingues et al., 2011 (23) | Low risk | Unclear risk | Low risk | Unclear risk | Unclear risk | Low risk |
| Doughty et al., 2002 (24) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Dracup et al., 2014 (25) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ducharme et al., 2005 (26) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Gámez-López et al., 2012 (27) | Low risk | Unclear risk | Low risk | Low risk | Unclear risk | Low risk |
| González-Guerrero et al., 2014 (28) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Hägglund et al., 2015 (29) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk |
| Holland et al., 2007 (30) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Jaarsma et al., 1999 (31) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Jaarsma et al., 2011 (32) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Jerant et al., 2001(33) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Kato et al., 2016 (34) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kimmelstiel et al., 2004 (35) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Koelling et al., 2005 (36) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Krumholz et al., 2002 (37) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Unclear risk |
| Leventhal et al., 2011 (38) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Mau et al., 2017 (39) | Low risk | High risk | Low risk | Unclear risk | Low risk | Low risk |
| Melin et al., 2018 (40) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Naylor et al., 2004 (41) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Negarandeh et al., 2019 (42) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Otsu et al., 2011 (43) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk |
| Ramachandran et al., 2007 (44) | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Rodríguez-Gázquez et al., 2012 (45) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Ruschel et al., 2018 (46) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Sethares et al., 2004 (47) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Stewart et al., 2015 (48) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Tomita et al., 2009 (49) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk |
| Tsuchihashi‐Makaya et al. 2013 (50) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk |
| Walkefield et al., 2008 (51) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Wierzchowiecki et al., 2006 (52) | Low risk | Unclear risk | Low risk | Unclear risk | Unclear risk | Low risk |
| Wright et al., 2003 (53) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk |
| Yu et al., 2015 (54) | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
Meta-analysis
The work included the results from 43 studies and analyzed hospital readmissions, during different follow-up periods, i.e., 6 weeks, 1 month, 2, 3, 6, 9, 12, and 24 months. Upon evaluating the combined effect, no statistically significant results were obtained in studies with follow-up <3 months nor at three months (Figure 2). Significant results were also not found at nine months (RR: 0.98, 95% CI: 0.64 to 1.54, I2: 61%), as well as at 24 months (RR: 0.72, 95% CI: 0.24 to 2.17, I2: 62%).
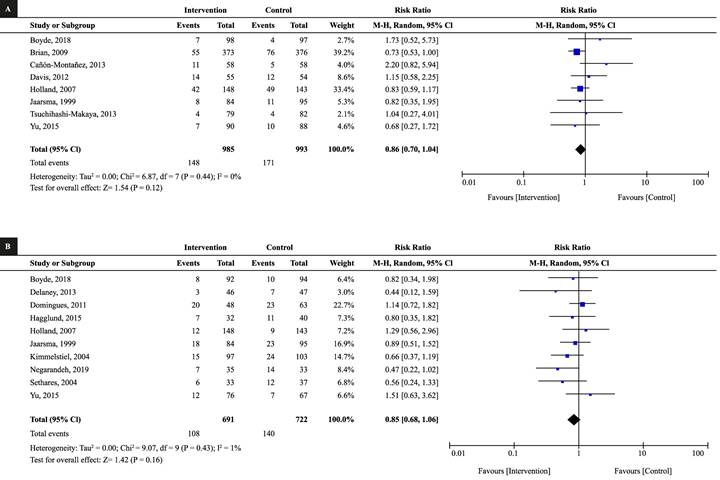
Figure 2 Meta-analysis of the effect of the educational interventions on reducing readmissions due to heart failure. (A) Follow-up <3 months, (B) Follow-up at 3 months
The MA of studies with follow-up at six months showed a 30% decrease in readmissions (RR: 0.70; 95% CI: 0.58 to 0.84; I2: 0%) and the 12-month follow-up evidenced 33% reduction (RR: 0.67; 95% CI: 0.58 to 0.76; I2: 52%); both analyses in favor of the group of educational interventions (Figure 3).
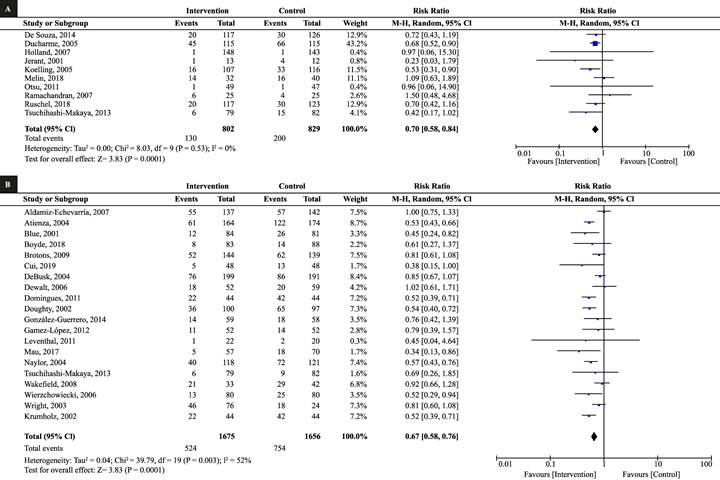
Figure 3 Meta-analysis of the effect of educational interventions on reducing readmissions due to heart failure. (A) Follow-up at 6 months, (B) Follow-up at 12 months
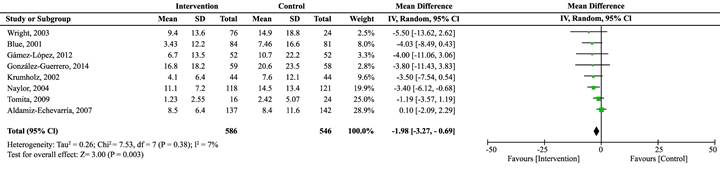
For the secondary outcome, days of hospital stay, no favorable effect was found of the educational interventions during the follow-up at three months (MD: -1.71; 95% CI: -3.87 to -0.46; I2: 0%) and six months (MD: 0.07; 95% CI: -1.33 to 1.45; I2: 0%). Nevertheless, the MA with follow-up at 12 months (Figure 4) evidenced a reduction of approximately two days in patients who received the educational interventions (MD: -1.98; 95% CI: -3.27 to -0.69; I2: 7%).
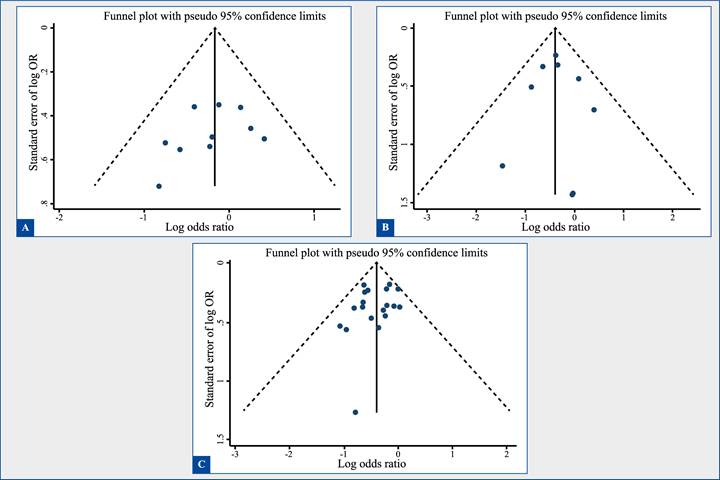
Evaluation of publication bias or bias due to missing results
Figure 5 shows funnel plot graphics to evaluate publication bias under analysis of 10 or more studies (three months, six months, and twelve months of follow-up). For the three times of follow-up, it is possible to observe generally a funnel shape that indicates that the studies are distributed uniformly on both sides of the average, which suggests lack of publication bias. The Egger statistical test also indicated absence of publication bias (3 months, p = 0.30; 6 months, p = 0.87, and 12 months, p = 0.26).
Discussion
This up-to-date synthesis of the evidence shows the favorable combined effect of educational interventions during prolonged follow-up times (six and twelve months) to reduce readmissions and time of hospital stay in adults with HF. These results are coherent with other SR and MA conducted prior to this study.55-57 In addition, the results found reinforce the importance of education for patients and of the multidisciplinary management of the HF syndrome. Similarly, these educational strategies become an alternative of effective intervention to improve the clinical outcomes of patients and which can be useful to reduce costs associated with health services due to HF decompensation. Within this context, a 2017 SR 55 concluded that educational interventions, especially those guided by nurses, have positive effects on decreasing readmissions due to HF.
Two of its studies, which are also part of this SR38,42 evidenced 50% reduction in readmissions when patients were subjected to educational interventions. In addition, an MA from 2019,56 that included seven of the RCTs from this study, demonstrates a reduction in hospital readmissions due to HF in follow-up from 6 to 12 months of 27% (RR: 0.73; 95% CI: 0.61 to 0.88; I2: 0%) and a general 22% reduction, which groups all the follow-up times. The previously stated, reaffirms the results obtained in this study and gives value to educational interventions as a low-cost strategy to improve the clinical response of patients with HF.
Likewise, another MA from 2019,57 obtained similar data. The researchers showed reduction of readmissions at 12 months of 36% (RR: 0.64; 95% CI: 0.53 to 0.78; I2: 51%). Moreover, this study also evidenced a decrease of approximately two days in hospital stay of adult patients with HF at 12-month follow-up and favorable for the educational interventions. However, no evidence was found of other SR or MA that have evaluated the effect of educational interventions for this result, becoming a significant contribution of this SR and which opens an important path to study this clinical outcome.57) These results of the evidence can be a starting point to restructure nursing care and management programs for adults with HF. A proactive scenario is proposed in which patients after their discharge continue being a priority and responsibility for health institutions to avoid new readmissions. The findings of studies with prolonged follow-up times show that companionship and active monitoring of patients by a multidisciplinary team generate a positive impact on the clinical outcomes of patients. 56,57
Another relevant aspect of this SR is that the educational interventions from the studies selected were variables on frequency, duration, methodology and personnel in charge of conducting them. Nevertheless, it is worth highlighting that a vast number of them were carried out by the nursing staff experienced in the cardiovascular area, which reinforces the importance of the nurses’ educator role as an effective strategy in reducing hospital readmissions and maintaining the quality of life of patients with HF. The aforementioned is based on nurses being the professionals called on to provide primary care in patients with chronic diseases.58,59
Also, it is important to mention although the study followed the methodological recommendations by the Cochrane Collaboration, this SR and MA had some limitations. First, lack of information is highlighted on the blinding of outcome assessment in some studies. Second, no additional analyses or meta-regressions were performed to explain possible sources of heterogeneity during some follow-up times I2 values > 60%. Lastly, this SR and MA did not use the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) methodology to evaluate the degrees of recommendation of the studies selected. Nonetheless, the evaluation of the risk of bias de los RCTs showed that most of the studies included had low risk of bias for the principal domains of the Cochrane RoB 1 tool.
In conclusion, this study demonstrates the protective effect of the educational interventions in adult patients with HF, compared with usual care, to reduce readmissions and days of hospital stay due to decompensation of the disease. Additionally, the results can be useful to reaffirm the need to implement in the clinical practice these intervention strategies during broad follow-up periods and which approach the patient during the transition from hospital to the home. Finally, the importance of participation of nurses in the multidisciplinary teams for the therapeutic approach of adult patients with HF is evident.