Introduction
Simulation training is an experience-based teaching methodology for rehearsing events in a safe environment.1,2 The use of simulators in any area is based on two principles: guaranteeing safety and preventing critical errors.3 In the case of clinical simulation, the manufacturers of medical equipment were the first to promote its initial development,4,5 but during its evolution, more attention has been paid to the underlying pedagogy.6 All simulation programs follow a well-defined structure, with clear pedagogic objectives, and following a series of stages: (a) Prebriefing: an initial informational session in which guidance is provided to students on the objective of the simulation, the environment, and the tools that will be utilized.4 (b) Scenario: this is the simulation experience itself, designed in agreement with the learning objectives, in which the students will perform various procedures, and make decisions that are similar to real clinical contexts.4,7 (c) Debriefing: time dedicated for reflecting on the events that took place during the simulated situation. This is the moment in time in which to confront and discuss the errors, as well as the technical and cognitive skills of students.3,8 Experiential learning is acquired in the debriefing phase, thanks to the reflection performed on the experience itself.9 Thus, many simulation programs include various scenarios in which different students participate, while the rest become observers. Likewise, some programs record the development of the scenario to later make comments and discuss it in the debriefing phase. Given its importance, many specific tools and guides have been developed to structure the debriefing, such as “The Diamond”9 and “Promoting Excellence and Reflective Learning in Simulation” (PEARLS).10
The simulation scenario can be developed through different tools, which result in many different simulation methods. Thus, we can differentiate between scenarios based on role playing, in which the students enter a controlled physical space, and which can be classified as simulation with manikins or anatomical models11,12 and simulations with actors, standardized patients or role-playing;13 and methods based on Information and Communication Technologies (ICT),12 which can be sub-classified as computer-based simulations14 and virtual reality methods.15
An important aspect in the design of training programs based on simulation is fidelity, which refers to the degree in which the simulation reproduces reality.12 The degree of fidelity depends on many aspects, mainly the realism of the simulator, the equipment used, and the degree in which the students are able to overcome their disbelief and act in the simulation as if they would in the real world.12 Having this in mind, clinical simulations are classified as low, medium, and high fidelity, with the latter being the gold standard in the field of simulation.16 Recently, a step forward was been taken with in situ simulation programs. These simulations take place in the space in which real clinical activities take place, thereby allowing health professionals to practice their skills in the work environment itself.17
The general objective of the present study is to analyze the most recent scientific evidence on the usefulness and implementation of training programs through simulations for Health Professionals. The specific objectives are: (i) to describe the scientific literature in the field of clinical simulation as an education method; (ii) to discover the characteristics of the most-utilized simulation methods and their efficacy, and (iii) to study the degree of implementation of simulation as a teaching methodology in different areas of healthcare.
Methods
For the development of the search and systematic review, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) method18 was used on large databases, Web of Science and Scopus, with the following combinations of keywords: (Simulation AND healthcare AND Professional Training) OR (Simulación AND Formación profesional). The inclusion criteria that the articles had to meet to be included in the review were: (a) complete original scientific articles, in English or Spanish, published in scientific journals, (b) articles published in the last 5 years, (c) articles that describe a simulation in the area of Health care, as well as a method of evaluation of its quality of training and the results of this evaluation, highlighting the pedagogic point of view, and (d) the study subjects must be Health Professionals, that is, health sciences students.
The following filters were applied during the search: (a) the words selected must be found in the article’s abstracts, (b) articles published between 2017 and 2021, (c) original scientific articles published in scientific journals, (d) articles published in English or Spanish (Figure 1).
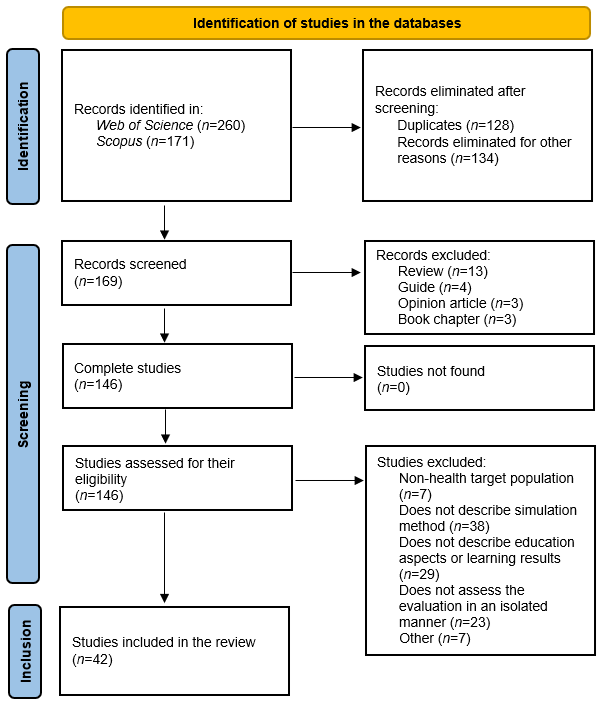
Figure 1 Summary of the articles identified in the systematic search, excluded and included in the review
For the evaluation of the studies obtained, a registration and analysis template was designed. The variables for which a specific number of options were available, were categorized, while the others were maintained with empty fields, for a qualitative study. After the systematic reading of the articles and the collection of data, the quantitative variables were analyzed with the graphics and statistical package Excel 2016. The numerical variables are presented as mean and standard deviation (SD), while the categorical ones were analyzed based on their frequency, and are therefore presented as percentages (%) of the total or absolute value (n). A thematic analysis was performed with the qualitative variables.
Results
Bibliometric analysis
Most of the studies included were accepted in 2020.19-24,25,26-31 With respect to the geographical distribution of the studies, most of them were conducted in the United Kingdom (29%) and the United States (21%), and were local, that is, they were conducted in a single center, or at different centers in the same city (81%), no international studies or studies conducted in collaboration between more than one country were found, while only three were conducted at the national level.19,20,32 Only one article from a Spanish-speaking country was included (Argentina).30
Methodological characteristics of the studies
A predominance of pre/post-test and mixed studies was observed. The most-utilized data collection instruments were: questionnaires (n=19) specifically designed by the research team, and composed by various types of questions, and externally-validated questionnaires (n=14 that assessed the students’ perceptions about their learning. The use of Likert-type scales was underlined in both types of questionnaires.
Within the qualitative studies (n=21), most used a thematic analysis of the data collected from one or many of the following sources: Open-ended questions included in the questionnaires (n=16); Focus groups or in-depth interviews (n=8), and debriefing sessions recorded on video (n=2).32,33 Some studies (n=15), also included data for the external assessment of the competencies acquired, such as the recording of events at hospitals, or assessments by their peers, the research team, or those in charge of the students, through the use of checklists, tests, and parameters collected by the instruments or manikins used. Among the main limitations of the studies, the most common aspects were related with the sample (small, convenience, low follow-up, previous experience with simulation, voluntary participants, or lack of a control group), and data collection (lack of validated instruments, data collection through the phone or online, lack of long-term data, and assessment of the impact of the program beyond the assessment by students).
Characteristics of the students
Most of the articles analyzed (60%, n=25) presented proposals framed within non-formal education, more specifically, continuous education, as an improvement strategy for professional qualifications. The rest of the works had formal education proposals (40%, n=17), with all of them conducted at the university level. In this area, it is important to underline that 67% of the studies were directed to more than one target professional. In this group of articles, the objective in most of them (75%) was the training of interprofessional teams, that is, the target was a team of professionals, instead of a specific type of professional, underlining the need and importance of multidisciplinary collaboration in complex tasks. Likewise, seven studies were identified,19,22,34-38 whose objective was the training of diverse types of professionals, with nursing personnel represented in all of them.
Methodological trends in simulation training
Most of the studies reviewed (64%) were only based on the role-playing methodology. On the other hand, about 15% of the works described a combination of more than one simulation method, with the role-playing one present in all of them, along with another method (computer simulation, virtual reality, and simulation with anatomical models). Only 17% (n=7) of the studies presented proposals that included the use of simulations via computer or virtual reality, and within them, almost half (n=3) were combined with role-playing.30,34,39 In most of them, the prebriefing, scenarios, and debriefing structure was followed. More specifically, nine articles used structured or validated debriefing models.22,31,35,40-45
As for fidelity, most of the article had high-fidelity simulation proposals (67%), while in 21% (n-9) of the articles, the type of fidelity could not be determined, as it was not specified in the text.2,24,27,33,38,45-48 With respect to the locations selected for the simulation to take place, 31% were conducted in simulation centers, and 24% at universities. It must be underlined that up to 19% (n=8) of the studies described simulation projects that took place in situ.2,28,31,38,49-52 As for the types of competencies that were worked on in the different simulation proposals, most of the studies included the acquisition of general or cross-sectional competencies, either in combination with the acquisition of specific competencies (43%, n=18), as well as in an isolated manner (36%, n=15). Thus, teaching methods with simulation seem to be evolving from technical competencies, to general ones. More specifically, three works33,34,53 aimed at training students on the use of the communication tool SBAR (Situation, Background, Assessment and Recommendation).54 This tool is becoming important in the area of health, for communication between professionals and patients. Also, in two studies,34,47 the simulation consisted in students experiencing the point of view of the patient and the complexity of the procedures they are subjected to, to stimulate empathy with people who are sick.
Results of learning through simulation
Most (n=32) of the studies described positive results in their objectives and hypotheses. Ten articles showed partially negative results with respect to their learning objectives. The negative results were associated with: (a) Simulation proposals based on ICT: one of them was not effective,20 while the bad execution of the rest was due to a connection problems, software, or the lack of awareness about the importance of learning through the use of these technologies.34 (b) Acquisition of knowledge: two studies showed the same efficacy between presentation-based methods, or conventional independent work,29,55 while in others, no differences were observed in this specific area between the pre- and post-test. (c) Target students: in the studies with groups of heterogeneous professionals, some of the learning results were not met in certain types of professionals, although they were obtained in the group of students as whole. The studies with a long-term assessment observed a decrease in the knowledge or skills acquired, which indicates the need for constant updating in this area, and justifies the planning of repeated training sessions.
The results of the qualitative analyses from most of the studies stressed improvements in: leadership and communication, teamwork, critical thinking, reflective learning, making of decisions, trust, and clinical skills. It is important to note that in all the studies that assessed the perception of the students on the simulation methodology, the responses were favorable towards the use of this training method, and the importance of learning by doing. In one study, only a minority of the students indicated their preference for presentation-type methods, as compared to computer-based simulations.55 On the other hand, the thematic analysis of a study whose simulation proposal was developed at a large scale, also revealed the theme of the complexity in organizing and developing a simulation with these characteristics.28 Additionally, the intervention developed in four studies promoted the assessment of errors and risks, and changed the management of the medical services themselves, where the interventions took place.31,49-51
Discussion
There is a large body of scientific bibliography on the field of simulation as a teaching-learning method for Health Professionals. However, publication in high-impact scientific journals predominated in English-speaking countries, and were immersed in university education and continuous education. Teaching through simulation is a well validated methodology.2 It has repeatedly been shown that it improves competency in many skills,56 as well as the trust perceived, the behaviors of speaking out loud, communication, and teamwork,57 so that simulation as an teaching method is deemed to be an excellent tool for addressing the skills required in multidisciplinary teams.56) The results of this systematic review indicate that the simulation methods did not increase the level of knowledge acquired, although they benefited the acquisition of skills and competencies, the central axes of modern education.58 Most of the works analyzed showed that these skills were acquired in a more significant manner in the high-fidelity simulation method through role-playing, in which person-to-person interactions are produced in a space with high-fidelity. The posterior debriefing sessions stimulate self-criticism, supported or not by watching the recorded scenarios, so that this methodology successfully combines experiential and reflective learning.59) Likewise, most of the simulation programs were positively evaluated by students, although only a few studies assessed the efficacy of this methodology beyond the first evaluation model by Kirkpatrick.60
On the other hand, although simulation through the use of virtual reality seems to be a very attractive area in the field of health education,15 the present review indicates that currently, there is little evidence on this respect. It is perhaps that this development is hampered by the technological difficulty inherent in simulation programs through virtual reality, together with its associated costs. Thus, the methods based on role-playing are still the gold standard in Healthcare. Also, the design of simulation programs must consider the need to repeat it in the long term, as our analysis pointed to the existence of a decrease in the knowledge or skills acquired through time; the modification of programs at the educational level and the training of the students, especially in the case of interdisciplinary groups, to obtain good results ;61 or the costs and logistic complications derived from the organization of large simulation training programs.28
Among the limitations of the study, we must consider those from the included studies themselves. Most of the studies were local in nature, and with small samples selected by convenience. However, most of the studies included utilized a mixed methodology and assessed the learning of the individuals through repeated measurements before and after the event (pre/post-test), and their systematic analysis offered very homogeneous results with respect to the advantages of learning through simulation.4
In conclusion, clinical simulation is a teaching methodology that has been progressively implemented in the last two decades, mostly in English-speaking countries, that utilizes techniques for its execution and assessment that have been validated and contrasted in many scientific studies, and which is useful for the training of general competencies and multidisciplinary teams.














