Introduction
Diabetes mellitus type 2 (DM2) is one of the non-communicable diseases that make up the high burden of morbidity and mortality in the world, representing a considerable public health problem.1 In agreement with International Diabetes Federation, there are 463 million adults with diabetes worldwide, and it is estimated that this number will increase to 578 million by 2030 and 700 million by 2045, since DM2 represents 90% of cases in the world and among people aged 50 to 74 years it is the fifth cause of death.2) Different strategies have been used in health services since the performance of the interdisciplinary team, seeking to face a problem that is expanding globally.3 However, for this, the commitment that the patient assumes with his care is decisive.
The programs conducted for self-care in patients with DM2 have been widely addressed by different studies that have been able to identify the benefits of the implementation of educational interventions in the context of primary health care for patients with DM2. These benefits are specifically identified in activities that promote a healthy lifestyle, motivating self-efficacy and a better level of adherence and disease control.4 In the development of programs focused on the individual, in order to contribute to decision-making and the search for a change in some patterns of risk in lifestyle, strategies that impact on primary health care services are seen as relevant.4) The literature shows that the use of educational interventions in patients with DM2, compared to habitual care, can improve self-control and the management of clinical parameters as well as reduce costs in health systems.5 Therefore, educational interventions have a high level of importance within self-care. Consequently, seeking to condense the literature, discover new strategies framed in the interventions, and call the attention of nursing professionals to the urgent need to deal with this problem, this scoping review aimed to synthesize the evidence on educational interventions for DM2 in primary health care.
Methods
Design and registration of the protocol. This is a scoping review (SR) guided by the recommendations of the Joanna Briggs Institute (JBI);6 and followed the Preferred Reporting Items for Systematic Reviews and the Meta-Analyses (PRISMA) checklist for scoping reviews.7 The protocol was registered under the serial number INPLASY202150091.8
Source of data and search strategy. Searches were performed in the following databases: MEDLINE (via PubMed), Excerpta Medica Database (EMBASE), Latin American Caribbean Health Sciences Literature (LILACS via BIREME), and Web of Science. In addition, gray literature was considered in the selection process. These searches were performance out from inception until March 2021 as indicated in Supplemental online 1.The following search strategy was used for MEDLINE: (Diabetes Mellitus, Type 2[MeSH Terms]) OR (Diabetes Mellitus, Type II) OR (Diabetes, Type 2) OR (Type 2 Diabetes) OR (Type 2 Diabetes Mellitus) AND (primary health care[MeSH Terms]) OR (Care, Primary Health) OR (Health Care, Primary) OR (Primary Healthcare) OR (Healthcare, Primary) AND (Education[MeSH Terms]) OR (Patient education[MeSH Terms]) OR (Education, Patient) OR (Patient Education) OR (Education of Patients) OR ((Health Education[MeSH Terms]) OR (Education, Health) OR (Education, Nursing[MeSH Terms]) OR (Nursing Education) OR (Educations, Nursing) OR (Nursing Educations) AND (Standard of Care[MeSH Terms]) OR (Care Standard) OR (Care Standards) OR (Standards of Care).
Eligibility criteria of the studies. This SR includes randomized controlled trials (RCTs), quasi-experimental, and cluster studies, published from inception until March 2021 in the languages of Portuguese, English, or Spanish, with both the abstract and full text available. The following PICO strategy (population, intervention, comparator, outcomes) was applied for study eligibility, P: adults with DM2 in primary health care, I: educational interventions; C: habitual or standard care, and O: improve clinical outcomes (adherence or compliance to treatment, diabetes control, knowledge and self-care).
Data extraction. The extracted data was collected in an Excel spreadsheet, containing the following information: author, year, country, study design, sample size, type of intervention, follow-up, control group, and main findings.
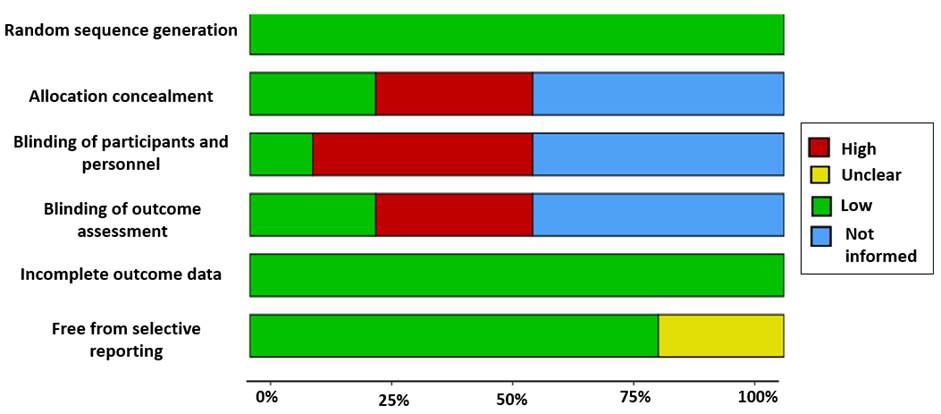
Risk of bias assessment. The risk of bias tool (RoB 1) from the Cochrane Collaboration was used to evaluate the risk of bias in RCTs. The following elements were evaluated: random sequence generation and allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting of results and other sources of bias.9 In addition, the JBI recommendations were used to assess the level of evidence of the studies.10 For the graphical visualization of the result of the methodological quality of the individual studies, it was carried out in the robvis web application. 11
Results
Identification and selection of the studies
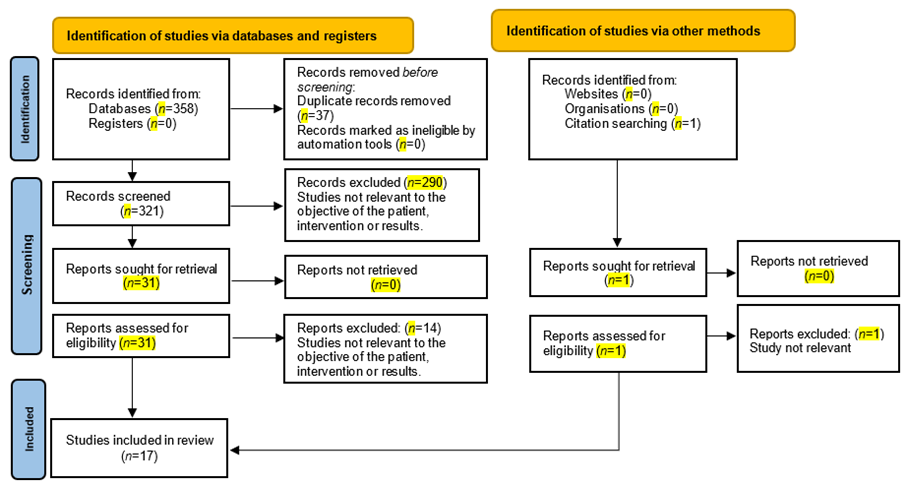
In total, 358 studies were identified (Figure 1). Of these, 37 duplicate articles were excluded, 321 studies being included for reading the title and abstract. Of those 321, 290 studies were excluded because they did not meet the objectives of the type of patient, type of study, educational intervention, location, or results found. Of the 31 remaining studies included for full text reading, 14 articles that did not meet the criteria established in the PICO strategy were excluded. Finally, seventeen studies meet the eligibility criteria for inclusion in this scoping review.
Characteristics of studies included
Of the 17 studies included in the SR. The studies were carried in 11 countries; of these, 65% of the studies were conducted in high-income countries, the rest being from low- and middle-income countries. These studies were published between 2010 and 2020. In relation to the type of study, it was found that 13 of the studies were randomized controlled trials and four cluster-randomized trials. Sample sizes ranged from 76 to 1589, with a mean of 344. The included studies were followed up for different periods, ranging from the first month after the intervention to 24 months. Studies with follow-up at 3, 6, and 12 months predominated. Although educational interventions showed a wide diversity, common strategies were found, such as education for diabetes control, a diabetes adherence and empowerment program, activities that included the individual, family, and communities. Education focused on the knowledge of the disease, warning signs, diet, and self-care practices. Regarding the control group, it was evident that all studies included standard care, that is, usual care. Educational interventions for the management of adults with DM2 were identified, which were grouped into four large categories, with the goal of projecting a better understanding of this review and a more delimited guide that serves health professionals in the implementation of interventions that respond to the needs identified in their practical environments.
Therapeutic adherence
Therapeutic adherence has historically represented one of the most important elements in the care of patients with DM2 and, with it, the execution of adequate treatment and control of the disease. Therefore, different countries have focused their educational intervention programs on adequate therapeutic adherence and, with this, seek to contribute to the management of DM2.12 Thus, as a study aimed to provide training to community health workers on the pathophysiology of the disease, risk factors for DM2, and lifestyle strategies with an impact on glycemic control (nutrition, exercise, physical activity, and prevention of diabetic complications), this educational intervention, which was received by the professionals who guided the patients with DM2, allowed a greater adherence to the treatment, which consequently brought the improvement of the blood glucose levels of the study participants.
Table 1 Characteristics of the included studies
| Authors, (year), country | Type of study | Sample size | Intervention group (IG) | Follow-up | Control group (CG) | Main findings | Level of evidence |
|---|---|---|---|---|---|---|---|
| Chen et al. (2020)13 China | Randomized clinical trial | 1325 | Education conferences | 12 months | Standard care | Blood glucose level decreased in the IG compared to the CG: | 1C |
| Intervention: 665 | Periodic follow-up interviews with physical examination | Difference-in-difference model (DID) = 0.53mmol (95% CI 0.90, to 0.16); p=0.005 | |||||
| Control: 660 | Specialized medical services | Diabetes knowledge score increased significantly in the IG compared to CG: | |||||
| DID = 0.91 (95 % CI 0.64-1.18) | |||||||
| De la Fuente et al. (2020)14 Spain | Randomized controlled clinical trial | 236 | Structured education provided by a nurse: | 12 and 24 months | Standard care | Glycated hemoglobin (HbA1C) | 1C |
| Intervention: 97 | Accompaniment to a family member or caregiver | IG:(−0.55, 95% CI −0.20, −0.90; p<0.001) | |||||
| Control: 139 | Basic knowledge of diabetes | CG: (0.06, 95% CI −0.14, +0.28, p=0.530) | |||||
| Use of empowerment model | HbA1C <7%: | ||||||
| IG: 35.2% vs. CG: 24.7% | |||||||
| Presley et al. (2020)15 United States | Randomized controlled trial | 97 | Community-based diabetes self-management education and peer support through the mHealth web application: | 6 months | Standard care | HbA1C reduction after 6 months: | 1C |
| Intervention: 62 | 12 weekly phone calls | IG: 10.1 (SD 1.7) to 9.6 (SD 1.9) | |||||
| Control: 35 | 3 monthly calls | CG: 9.8 (SD 7) to 9.1 (SD 1.9) | |||||
| Reduction of diabetes distress in both groups: | |||||||
| p<0.001 | |||||||
| White et al. (2020)16) United States | Cluster randomized clinical trial | 364 | Partnership to improve diabetes education: | 12 and 24 months | Standard care | Treatment effects on 12 months: | 1C |
| Intervention: 184 | Literacy-sensitive, provider-centered health communication intervention | Adjusted HbA1C: | |||||
| Control: 180 | IG: (−0.76 [95% CI, −1.08 to - 0.44]; p<0.001 | ||||||
| CG: (-0.54 [95% CI, - 0.86 to - 0.21]; p=0.001) | |||||||
| Satisfaction with treatment: | |||||||
| IG: (3.93 [95% CI, 2.48-6.21]; p<0.001) | |||||||
| CG: (3.04 [95% CI, 1.93-4.77]; p<0.001) | |||||||
| Self-efficacy: | |||||||
| IG: (2.97 [95% CI, 1.89-4.67]; p<0.001) | |||||||
| CG: (1.81 [95% CI, 1.1-2.84]; p=0.01) | |||||||
| Sharoni et al. (2018)17) Malaysia | Randomized controlled trial | 76 | Health education program, based on: | 1 month and 3 months | Standard care | Foot self-care behavior after 12 months: | 1C |
| Intervention: 36 | Theory of self-efficacy of Albert Bandura | IG: 62.61 (SD 7.54) | |||||
| Control: 36 | Group Diabetes Education Seminars | CG: 47.55 (SD 7.30) | |||||
| Foot care self-efficacy after 12 months: | |||||||
| IG: 40.89 (SD 4.91) | |||||||
| CG: 34.37 (SD 4.69) Knowledge of foot care after 12 months: | |||||||
| IG: 7.68 (SD 1.49) | |||||||
| CG: 5.16 (SD 3.09) | |||||||
| Santos et al. (2017)18) Brazil | Cluster randomized clinical trial | 238 | Adherence and empowerment program in diabetes: | 12 months (3-months intervals) | Standard care | Glycemic control (HbA1c): | 1C |
| Intervention: 127 | Group education | IG: 7.10 (5-12.4); p=0.001 | |||||
| Control: 111 | Home visits | CG: 7.40 (4.9-13.9); p=0.3000 | |||||
| Telephone monitoring | Self-care questionnaire for DM2: | ||||||
| IG: 4.05 (1.75-6.25); p=0.0001 | |||||||
| CG: 3.00 (1.25-6.1); p=0.9700 | |||||||
| Empowerment questionnaire for DM2: | |||||||
| IG: 4.13 (2.75-5); p=0.001 | |||||||
| CG: 4.00 (2.5-4.88); p=0.001 | |||||||
| Paz-Pacheco et al. (2017)19 Filipinas | Randomized clinical trial | 155 | Diabetes self-management education: | 3 and 6 months | Standard care | Glycemic control (HbA1C≤7.0) after 6 months: n (%) | 1C |
| Intervention: 85 | During the follow-up visits, 8 topics were taught. | IG: 43 (59.72) | |||||
| Control: 70 | CG: 20 (38.46) | ||||||
| Foot examination after 3 months: n (%) | |||||||
| IG: 49 (76.56) vs. CG: 34 (57.63) | |||||||
| Grillo et al. (2016)20 Brazil | Randomized clinical trial | 137 | Diabetes self-management education: | 12 months | Standard care | Knowledge of diabetes mellitus after 12 months: | 1C |
| Intervention: 69 | Identification of modifiable factors | IG: 16 (3%) | |||||
| Control: 68 | Non-pharmacological treatment | CG: 12 (4%) | |||||
| Drug therapy | Glycemic control (HbA1C) after 12 months: | ||||||
| Complications of chronic diabetes | IG: 8.7 (1.7%) vs. CG: 9.2 (2.2%) | ||||||
| Foot care | |||||||
| Pérez-Escamilla et al. (2015)12 United States | Randomized clinical trial | 211 | Latino Diabetes Best Practices Program: | 3, 6, 12 and 18 months | Standard care | Glycemic control (HbA1C) after 18 months: | 1C |
| Intervention: 105 | Self-management of diabetes | IC: 9.32 (8.91, 9.74) | |||||
| Control: 106 | Medications for diabetes | CG: 8.77 (8.35, 9.20) | |||||
| Nutrition and exercise | |||||||
| Intercultural counseling | |||||||
| Mental health | |||||||
| Merakou et al. (2015)21 Grecia | Clinically controlled trial | 193 | Structured group educational program: | Not informed | Standard care | Glycemic control (HbA1C) after 6 months: | 1C |
| Intervention: 138 | Conversation Maps: Learning About Diabetes | IG: 1.4 (95% CI: 1.1, 1.7; p<0.001) | |||||
| Control: 55 | CG: 0.5 (95% CI: 0.5, 0.3; p=0.003) | ||||||
| Maps for people with DM2 are more effective in diabetes self-management | |||||||
| Ruggiero et al. (2014)22 United States | Randomized controlled clinical trial | 266 | Physician Assistant Self-Care Coaching: | 6 and 12 months | Standard care | Medication adherence: | 1C |
| Intervention: 134 | Patient-centered and individualized | IG: 6.6 (SD 2.0) | |||||
| Control: 132 | Transtheoretical model | CG: 6.12 (SD 2.4) | |||||
| Empowerment model | Diabetes self-care behaviors: | ||||||
| Best practice advice | IG: 3.81 (SD 2.2) | ||||||
| CG: 3.48 (SD 2.2) | |||||||
| There results were not significant. | |||||||
| Plotnikoff et al. (2011)23 Canada | Randomized clinical trial | 96 | Diabetes Education Program Plus Physical activity: | 3, 6 and 12 months | Standard care | Glycemic control after 12 months: | 1C |
| Intervention: 49 | Energy Expenditure and Fitness | IG: -0.5 (-0.9 to -0.2; p<0.01) | |||||
| Control: 47 | Modified Canadian Aerobic Fitness Test | CG: -0.4 (-0.7-0.0) | |||||
| Phone support | Physical Activity after 12 months: | ||||||
| IG: 654.2 (466.9-841.6; (p<0.01) | |||||||
| CG: -33.9 (-213.6-145.8) | |||||||
| Quinn et al. (2011)24 Canada | Cluster-randomized clinical trial | 163 | Mobile Diabetes Intervention: | 12 months | Standard care | Glycemic control after 12 months: | 1C |
| Intervention: 107 | Coach-only | IG: 1.9% (95% CI 1.5-2.3) | |||||
| Control: 56 | Coach primary care providers portal | CG: 0.7% (0.3-1.1) | |||||
| Coach primary care providers portal with decision-support | There were no significant results in relation to diabetes distress, depression, diabetes symptoms, or blood pressure and lipid levels (all p>0.05). | ||||||
| Sönnichsen et al. (2010)25 Austria | Cluster-randomized controlled trial | 1489 | Disease management programs “Therapie aktiv”: | 12 months | Standard care | Glycemic control (HbA1C): | 1C |
| Intervention: 649 | Group for Preventive Medicine Salzburg | IG: 0.41% [95 CI % 0.32; 0.50] | |||||
| Control: 840 | Standardized documentation of physical examination | CG: 0.28% [95 CI % 0.21; 0.35] | |||||
| Structured interdisciplinary care | Eye examination: | ||||||
| IG: 71.0% vs. CG: 51.2% | |||||||
| Foot examination: | |||||||
| IG: 73.8% vs.CG: 45.1% | |||||||
| Patient education: | |||||||
| IG: 49.5% vs. CG: 20.1% | |||||||
| Gaillard et al. (2015)26 United States | Randomized clinical trial | 96 | Diabetes Self-Management and Support: | 6 months | Standard care | Glycemic control (HbA1C) after 6 months: | 1C |
| Intervention: 58 | Community health worker | IG: 7.5 (1.3%; p=0.02) | |||||
| Control: 38 | Diabetes self-management training | CG: 7.7 (1.5%; p=0.405) | |||||
| Weekly call support | No significant changes in metabolic parameters | ||||||
| Community resources | |||||||
| Gehlawat et al. (2019)27 India | Randomized controlled trial | 314 | Diabetes Self-Care Activities: | 6 months | Standard care | Self-care of the feet: | 1C |
| Intervention: 157 | Education sessions of 45 minutes | IG: 3.64 vs. CG: 2.21 | |||||
| Control: 157 | Self-care kits (mirror, an oil bottle, and glucose tablets) | Both groups: 1.95 (1.4-2.4; p<0.001) | |||||
| Inspect the inside of your footwear: | |||||||
| IG: 1.34 vs. CG: 0.04 | |||||||
| Both groups: 0.78 (0.5-1.0; p<0.001) | |||||||
| Romero-Guevara et al. (2019)28 Colombia | Randomized controlled trial | 200 Intervention: 98 Control: 102 | Teaching: Individual: | 6 and 12 months | Standard care | Systolic blood pressure in 24 (mmHg): | 1C |
| Six educational sessions of 20 to 40 minutes: Behavior modification; teaching, disease process, prescribed medication, prescribed diet and exercise and coping enhancement | IG: 125 (SD 14.6) | ||||||
| By two nurses | CG: 123 (SD 13.9) | ||||||
| HbA1c: | |||||||
| IG: 6.19 (SD 1.71) | |||||||
| CG: 6.15 (SD 1.44) | |||||||
| These results were not significant. |
In the United States, a study which carried two groups through an intervention using two guides on educational intervention for DM2 (one of the groups used the kit designed to improve diabetes education in the intervention, sessions were carried out that included updating on diabetes and instruction on techniques to improve communication in health, and the second group received guidance based on the National Health Program as an intervention. Diabetes Education to carry out discussions for the care of the disease) found that after these interventions in patients with diabetes, satisfaction with treatment presented significant results (3.93 [95% confidence interval (CI), 2.48-6.21]; p<0.001 versus 3.04 [95% CI, 1.93-4.77]; p<0.001), improving adherence to treatment.16) Another study through the delivery of material created by an interdisciplinary group based on the American Diabetes Association and the American Association of Diabetes Educators, was carried out with an educational intervention in small groups with 45-minute sections, focused on the self-care of “healthy eating, being active, regular blood sugar control, taking medication on time, problem solving, risk reduction and healthy coping,” resulting in 2% adherence to medication for control of blood glucose levels by the participants.27
Self-care and self-management in diabetes
The evidence has shown the high morbidity rate that diabetes mellitus represents. In this sense, the implementation of educational interventions that are focused on the proper management of it will consequently allow a positive impact on the self-care of patients. Thus, a study that applied the theory of self-efficacy in the self-care behavior with the feet in adults with DM2, allowed to obtain improvements in the performance and indirect experience of the physical and emotional states and verbal persuasion of the participants.17The application of this theory has shown significant results in self-care and knowledge of DM2 when comparing the intervention group to which the theory was applied and the control group that received standard treatment (p<0.01).16) Structured education programs in primary health care settings have shown the effectiveness of self-care practices and a significant improvement of 33.5% [95% CI: 22.9-44.0].27 This, therefore, shows foot care’s considerable relevance since it seeks to also impact the patient's own self-care and thereby improve knowledge about the disease, which has led to significant results at 6 at 12 months of intervention (p<0.01).22) On the other hand, adherence and empowerment are indicators that can present improvement through self-care practices. A study carried out in Brazil implemented a strategy of group education and family visits. This group education strategy produced better results in relation to glycemic control and diabetes self-care.18 Through educational interventions, it has also been shown that knowledge about diabetes significantly increased in the group that received the educational intervention versus the control group (where it decreased), with the difference-in-difference model (DID) equal to (0.91 [95% CI: 0.64-1.18], p<0.001).13 Likewise, a study found that community-based, peer-supported education shows a significant reduction in diabetes distress (p<0.001).15
Glycemic control of diabetes
The versatility of measures such as web applications for the education of patients with DM2 that have allowed a significant reduction in HbA1C (p=0.004).15 A study with the intervention with web portals showed a mean decrease in glycated hemoglobin of 1.9% in contrast to standard care 0.7%, which has a variance of 1.2% (p=0.001) at 12 months.24 The literature has been consistent in demonstrating the positive results of group programs for education in patients with DM2. Two studies showed significant results (p<0.001) in the reduction of glycated hemoglobin compared to other interventions, such as home visits, or standard care.16,21 Interventions in structured groups have also made it possible to improve the knowledge of patients in relation to DM2, and with this, they have prevented the elevation of HbA1C.20) The inclusion of cultural aspects in educational interventions in a Latino population residing in the United States achieved a significant reduction in the HbA1C difference at 3 months (p=0.043), followed by a reduction difference at 6 months (p=0.05) and finally at 18 months (p=0.009).12 Similarly, a culturally adapted self-care coaching intervention for racial/ethnic minority populations showed significant improvement in blood glucose levels.22) Likewise, the individualized educational intervention in a study carried out in Austria showed significant reductions in weight and cholesterol, but it did not significantly influence metabolic control measured by HbA1C after one year.25 With this, physical activity advice as an educational intervention has been effective in promoting a significant reduction in HbA1C 0.5% (p<0.01). Additionally, it has left positive results in glycemic control and the health of patients with DM2.23 These types of activities that provide accompaniment and support in lifestyle have shown that it is possible to obtain a significant reduction in HbA1C (p=0.02) and in random blood glucose levels (p=0.03), compared to standard care. Thus, approaching the patient as an integral being through empowerment and commitment undoubtedly allows for even more successful interventions for diabetes self-management.19,26)
Nursing and its role in educational interventions in patients with DM2
In the development of educational interventions, the multidisciplinary health team plays a fundamental role. However, it is recognized that nursing professionals have a differentiated scope within the team. Patient-centered interventions, which have the execution and accompaniment of the nursing staff, have allowed patients to self-identify their challenges and thus together be able to develop different strategies to overcome them.26) It has also been shown that the educational strategies that are stimulated by other educational components outside the standard, and that guide the restructuring of behaviors, through education on the disease process, prescribed medication, diet, prescribed exercise, and improvement in coping with the disease by nursing professionals in the care of patients with DM2, it has generated encouraging results.28 A study showed the importance of having professionals who have vast experience in education on DM2 through various structured and individualized educational interventions. The participants and their caregivers improved autonomy, allowing greater metabolic control and achievement of their long-term therapeutic goals.14) Educational interventions have shown a great role in the care of diseases. The evidence showed that the performance of the nursing professional in the execution of these interventions prevents the increase in HbA1C in patients with diabetes. This is possible through the training of groups with patients with DM2, through familiarization and training in diabetic education for the identification of risk factors, and the non-compliance with pharmacological treatment when compared to other educating agents.20
Risk of bias of the studies included
The results of the analysis of the quality of the included studies is presented in Table 2, performed based on the parameters evaluated by RoB 1 in the 17 included studies. 88% described adequate random sequence generation12-16,18-20,22-28 and 23% described allocation concealment.17,24,25,28 Only two articles described blinding of participants and staff,12,28 and 23% described blinding of outcome assessment.12,14,20,28 Regarding the risk of selective reporting of results, it was shown that 76% described the proposed results from the beginning12-14,16-18,20-22,25-28 (Figure 2 and Table 2). According to the JBI, the level of evidence of the 17 studies was 1C.
Table 2 Risk of bias among included studies
| Studies | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting of results |
|---|---|---|---|---|---|---|
| Chen et al. (2020)13 | Low risk | High risk | Not informed | Not informed | Low risk | Low risk |
| De la Fuente et al. (2020)14 | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Presley et al. (2020)15 | Low risk | Not informed | Not informed | Not informed | Low risk | Unclear risk* |
| White et al. (2020)16 | Low risk | Not informed | Not informed | Not informed | Low risk | Low risk |
| Sharoni et al. (2018)17 | High risk | Low risk | High risk | High risk | Low risk | Low risk |
| Santos et al. (2017)18 | Low risk | Not informed | High risk | High risk | Low risk | Low risk |
| Paz-Pacheco et al. (2017)19 | Low risk | Not informed | Not informed | Not informed | Low risk | Unclear risk* |
| Grillo et al. (2016)20 | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Pérez-Escamilla et al. (2015)12 | Low risk | Not informed | Low risk | Low risk | Low risk | Low risk |
| Merakou et al. (2015)21 | High risk | High risk | High risk | High risk | Low risk | Low risk |
| Ruggiero et al. (2014)22 | Low risk | High risk | High risk | High risk | Low risk | Low risk |
| Plotnikoff et al. (2011)23 | Low risk | Not informed | Not informed | Not informed | Low risk | Unclear risk* |
| Quinn et al. (2011)24 | Low risk | Low risk | Not informed | Not informed | Low risk | Unclear risk* |
| Sönnichsen et al. (2010)25 | Low risk | Low risk | High risk | High risk | Low risk | Low risk |
| Gaillard, et al. (2015)26 | Low risk | Not informed | Not informed | Not informed | Low risk | Low risk |
| Gehlawat et al. (2019)27 | Low risk | Not informed | Not informed | Not informed | Low risk | Low risk |
| Romero-Guevara et al. (2019)28 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
* Study registration or published protocol not found.
Discussion
The results of the review made it possible to identify educational interventions in individuals with DM2 in primary health care, which were categorized into four main aspects, representing a challenge for nursing professionals seeking: control of the disease, adherence by the patient to the programs, adherence to the therapeutic regimen, showing to a positive impact on quality of life. Our results were consistent in showing that educational interventions have shown significant impacts on adherence and therapeutic satisfaction.
This result agrees with other findings where the patient's adherence to the drug regimen showed a reduction in the severity of complications. It is believed that medication adherence factors in chronic patients can be made up of five major categories including economic and social factors, the health team, and the patient care system as well as treatment-related factors. Patient-related factors can be modified through education and increased knowledge.29Likewise, the evidence has shown the positive effects of educational interventions with an emphasis on self-care, these have shown improvements in self-efficacy during the health-disease processes faced by the population, highlighting an aspect that becomes relevant and that was evidenced in the results for coping with health conditions, such as empowerment and awareness of the disease. It is also shown that the inclusion approach of the patient and their family environment brings an improvement in knowledge and that it will thus have an influence on prevention of future complications such as foot care and other organs that may be affected.4,30 Through the application of these educational interventions, different strategies have been implemented, providing educational interventions individually and in groups. However, a meta-analysis supports our findings. It shows significant results to improve knowledge, self-control of the disease based on knowledge about the condition itself, and the treatment and identification of one's own abilities. This consequently brings about the reduction of HbA1C levels in self-care interventions aimed at groups (p<0.0001).31
Within this review, the relevant role of the use of strategies through technological resources was evidenced, giving an encouraging panorama in the combination of methodologies that seek to adapt to the specific conditions of the population and have shown a favorable impact on the lifestyle of patients presenting a reduction in HbA1C levels up to 0.38%. It also allows secondary results in the improvement of knowledge and other comorbidities, all this giving support for the combination of methodologies that will impact positive results both in the population and in the health system with the use of low-cost strategies.32) Therefore, showing the very positive results of educational interventions in patients with DM2, the nursing professional plays a very important role in the proper planning and execution of these patient-centered interventions for the self-control of the disease and its role in decision making, demonstrating with this relevant scope in the modification and obtaining of controlled clinical parameters in patients.30 Thus, educational interventions in patients with diabetes mellitus have identified a relevant reference point, when compared to care, not only because it involves compliance with figures between normal values in clinical parameters but also because it allows contributions in the implementation of these programs with different methodologies, multidisciplinary teams, and both individual and group approaches.4,33
Although this SR was carried out under PRISMA guidelines, it has some limitations. First, searches were only carried out in MEDLINE, EMBASE, LILACS, Web of Science and gray literature. Second, the analysis of the quality of the included studies showed lack of information on allocation concealment, blinding of outcomes assessment and blinding of participants and staff in some studies. Lastly, this review did not use the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) methodology to evaluate the degrees of recommendation of the studies selected. Nonetheless, the JBI recommendations were used to assess the level of evidence of the studies.
Conclusion
The findings of this review suggest that educational interventions in patients with DM2 in the primary health care setting can have a positive impact on therapeutic adherence, self-control and knowledge of the disease. In addition, it was possible to identify the influence of health teams, pointing out the scope of nursing professionals in the construction and implementation of educational interventions for better health outcomes. This way, the value of the performance of the nursing profession in its investigative, academic, practical, and management role that results in a contribution to the discipline and the community is pointed out.