Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Salud Uninorte
Print version ISSN 0120-5552On-line version ISSN 2011-7531
Salud, Barranquilla vol.27 no.1 Barranquilla Jan./June 2011
Body Mass Index and its correlation with pulmonary function in patients with cystic fibrosis from Cartagena (Colombia)
Indice de Masa Corporal y su correlación con la función pulmonar en pacientes con fibrosis quística en Cartagena (Colombia)
Gustavo Mora Garda1, Enrique Ramos Clason2, Fabio Anaya Lorduy3, Dacia Malambo García4, Claudio Gómez Alegría5, Doris Gómez Camargo6
1 MD. Estudiante doctoral, Facultad de Medicina, Universidad de Cartagena. Doctorado en Medicina Tropical.
2 MD, MSc. Profesor, Universidad de Cartagena, Facultad de Medicina, Departamento de Investigaciones.
3 Clínica Universitaria San Juan de Dios, Departamento de Neumología Pediátrica.
4 MSc. profesora de la Universidad de Cartagena.
5 Ph. D profesor asociado, Facultad de Ciencias, Departamento de Farmacia de la Universidad Nacional.
6 Ph. D. Universidad de Cartagena (Colombia). degomez@hotmail.com
Correspondencia: Universidad de Cartagena, Facultad de Medicina, Laboratorio de Investigaciones, primer piso. Campus de Zaragocilla, sede Ciudad de Bolívar, Avenida el Consulado, calle 30 n° 481452. degomez@hotmail.com
Fecha de recepción: 26 de octubre de 2010 Fecha de aceptación: 8 de febrero de 2011
Abstract
Background. Sinus-pulmonary manifestations are a major concern in CF patients. Pulmonary function shows a strong relationship with nutritional status. In Colombia, malnutrition is a public health issue; however there are no reports that fully analyze nutritional status and lung function in CF children.
Materials and Methods. A cross-sectional study was developed conducted with 32 patients registered in the CF Attention Program. Measurements were performed following the NIOSH Spirometry Training Guide. Body Mass Index (Z-Score) was calculated according to Onis.et.al. Correlation was determined by a regression model. Results. 14 children were able to perform the test with criteria for the study, mean for age 12.4 ± 3.4 years. % Forced Expiratory Volume1 and % Forced Vital Capacity means were 66.7 ± 28.5 and 69.5 ± 2.0, respectively. Body Mass Index (Z-score) mean was -1.17. BMI-regression for % Forced Expiratory Volume1, r2=0.31(P<0.01); % Forced Vital Capacity, r2=0.22(P<.01).
Conclusions. Results demonstrated a correlation between Body Mass Index and Lung Function. This correlation persists, even in populations with notorious nutritional deficit such as this group. Special nutritional therapies should be implemented for this group and similar populations.
Keywords: Cystic fibrosis, nutritional status, Body Mass Index, spirometry.
Resumen
Introducción: Las manifestaciones sinopulmonares son de gran interés en pacientes con fibrosis quística. La función pulmonar se ha correlacionado con el estado nutricional en estos pacientes. En Colombia, la malnutrición es un problema de importancia para la salud pública; sin embargo, no se han publicado reportes que analicen el estado nutricional y la función pulmonar en pacientes con fibrosis quística.
Materiales y métodos: Se disenó un estudio transversal con 32 pacientes registrados en el Programa de Atención Integral para Pacientes con Fibrosis Quística y sus familias. Los exámenes se realizaron siguiendo la guía de entrenamiento de la NIOSH. El índice de Masa Corporal (Z-Score) fue calculado siguiendo las recomendaciones de Onis et al. El grado de correlación fue determinado por un modelo de regresión.
Resultados: 14 ninos fueron incluidos para realizar las pruebas con los criterios del estudio; la edad media fue 12,4±3,4anos; para %Volumen Expiratorio Forzado y %Capacidad Vital Forzada las medias fueron 66,7±28,5 y 69,5±22,0 respectivamente. La media del índice de Masa Corporal (Z-score) fue -1,17. La regresión del índice de Masa Corporal para %Volumen Expiratorio Forzado1 fue r2=0,31(P<0,01), y para %Capacidad Vital Forzada, r2=0,22(P<0,01).
Conclusiones: Los resultados demostraron correlación entre el índice de Masa Corporal y la función pulmonar. Esta correlación persistió incluso en poblaciones con un notorio déficit nutricional como la de este estudio. Una terapia nutricional específica debería ser implementada en este grupo y poblaciones similares.
Palabras clave: Fibrosis quística, estado nutricional, índice de Masa Corporal, espirometría.
Introducción
Cystic Fibrosis (CF) is the most common life-limiting autosomic recessive disease among Caucasians and its incidence is approximately 1/3000 live births (1-4). In Latin America, incidence range varies due to the ethnic heterogeneity. There are values reported as high as 1/1587 and others considerably lower, expressed between 1/8500 and 1/32258 (3, 5, 6).
CF alterations are caused by several mutations in Cystic Fibrosis Conductance Trans-membrane Regulator (CFTR) gene that encodes for a transmembrane protein (4, 7-8). This defect disrupts chloride conductance, expressing clinical features that involve respiratory and digestive systems, and exo-crine glands (9-11). The sinus-pulmonary manifestations are the major focus of morbidity and mortality, characterized by a continued deterioration in lung function, persistent inflammation and chronic infection with opportunistic agents such as Pseudo-monas aeruginosa, Staphylococcus aureus, and Haemophilus influenzae (12, 13).
Spirometry is the most important test to evaluate and monitor pulmonary function in patients with CF (14-16). Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1) are the most used standard parameters in order to determinate patient's lung function (17). FEV1 is the principal reference value for monitoring lung function and is the most accurate predictor for mortality in CF (14, 17).
Pulmonary function shows a strong relation with nutritional status, expressed generally by the Body Mass Index (BMI), nutrition indexes have predictive value over FEV1 (18, 19). According to this, the Patient Registry Annual Data Report established the BMI percentile 50 as the goal for children with CF (18). Moreover, nutritional status is correlated with quality of life in adults with CF(20). Thus, nutritional indexes and lung function test are the most important values in order to monitor the evolution of patients with CF. In Colombia, malnutrition is a public health issue, however there is no report concerning to the correlation between BMI and pulmonary function in Colombian patients with CF. The aim of this study was to describe these variables, and calculate the grade of association between nutritional status and lung function parameters in CF patients (21).
MATERIALS AND METHODS
A cross-sectional study was performed, with 32 pediatric patients included in the "Programa de Atención Integral para Pacientes con Fibrosis Quística" (Integral Attention Program for Patients with Cystic Fibro-sis), designed by the "Universidad de Cartagena", in the Colombian Caribbean Coast. All patients had clinical features suggestive of CF and were positive for at least 2 iontophoresis tests. Due to difficulties previously reported, to perform lung function tests by spirometry in patients younger than 6 years old, this group was excluded (15).
Nutritional status for all patients was calculated by the Body Mass Index (BMI), and then compared with the standard values published in 2007 by Mercedes de Onis et al. (22). Indexes were finally expressed as Z-Scores for specific age and percentiles referenced for specific age and gender, following the recommendations published by Sinaasappel M. et al. in their consensus report (23).
Spirometer Pneumos 300 (H&C SPA, Italy) was used to perform lung function measurements in concordance to its tecnical specification with the requirement published by the American Thoracic Society and the European Respiratory Society already verified. Lung function tests were made domiciliary by staff's members previously trained and specialized in management of patients with CF (16, 24, 25). Procedures were performed on stiff chairs, with no wheels, in rooms with adequate ventilation and stable temperature (environmental temperature between 29°C and 33°C), all patients were asked to make themselves comfortable before and during the test.
Although most patients are familiar with the test, all of them were verbally trained; relevance of useful results was emphasized. Neck movements were specially evaluated during the procedures, in order to conserve an appropriate position and preserve the reproducibility of measurements. Nose clips were not used. Other general considerations were made, following the maneuvers described in the NIOSH Spirometry Training Guide (26).
The first three measurements considered as reproducible were registered; mean value of these three tests was defined as a reliable result. None of the patients performed 8 attempts or more in order to obtain acceptable values for FVC and FEV1. For this study, only FVC and FEV1, and their respective % FVC and % FEV, were registered to determine lung function.
Values for %VEF1, %CVF and BMI Z-Score were defined as continuous quantitative variables, and their association was based on an n-dimensional analysis. Linear regression was applied to establish correlation between BMI and lung function, with a 95% confidence limit. P< 0.05 was considered as significant. The procedures were conducted using EpiInfo 3.3.2, developed by the Epidemiology Program Office of the Centers for Disease Control and Prevention (CDC).
Informed consent was evaluated and approved by the University of Cartagena Ethics Committee. A written consent was requested for each patient and their parents.
RESULTS
Residents from the Colombian Caribbean
A total of 14 children (9 boys, 5 girls) fulfilled the criteria for the study. Average age was 12.4 ± 3.4 years old. Measurements for lung function were taken at least 4 times; the mean of the 3 highest percents was registered as the final value.
Height and weight Z-score average for specific age were (-0.005) and (-1.10), respectively. In percentile distribution for height, 1 patient was below percentile 3; (21%) (n = 3) were in the 3-10 percentile interval; and another (21%) of patients were within the 10-25 percentile interval; 1 patient (7%) was in the 25-50 percentile interval; (21%) were in the 75-90 interval, 1 patient was in the 9097 interval, and 2 patients (14%) were over the 97 percentile.
There were no patients in the 50-75 percentile interval.
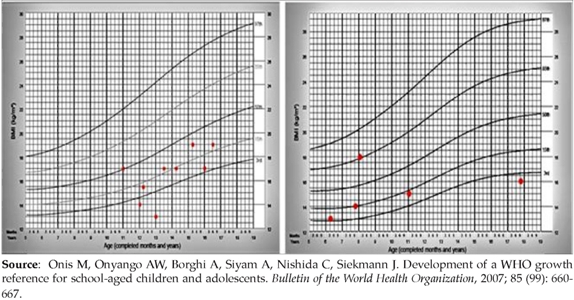
BMI Z-Score average for specific age was (-1.1). The variation range for BMI Z-Score was expressed for the interval at (-2.44: 0.5). The BMI value of one boy was over 50 percentile and only one girl, registered an index, over this percentile (figure 1).
Figure 1. (Modified from WHO Bulletin [22]) BMI distribution associated to specific genderand page in pediatrics patients. A) Graphic adapted to boys. M=-109, Z-Score; B) Graphic adapted to girls. M= -1.31, Z-Score.
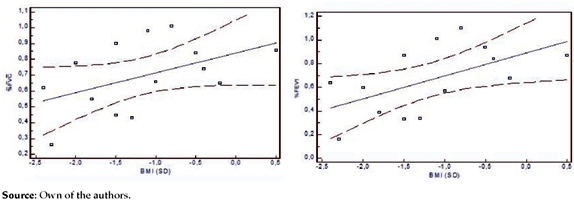
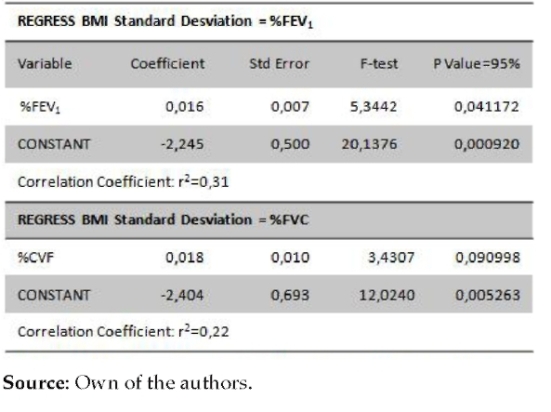
The measurements for FEV: and FVC were registered in litters; means for these variables were (1.8 ± 1.2) lt. and (2.0 ± 1.3) lt., respectively. Mean for predictive %FEV: was (66.7 ± 28.5) and for %FVC was (69.5 ± 22.0). %FEVj and %FVC predictive values were both below 80% in 9 patients (Figure 2). %FEVj and %FVC dispersion related with BMI is demonstrated in figure 2. Central tendency lines slopes described a direct relation between both %FEV1 and %FVC, expressing that an increase in BMI coincides with improvement in pulmonary function values. BMI Z-Score regression for %FEV: was r2 = 0.31 (P<0.01); and for %FVC was, r2 = 0.22. (P<0.01) (Tabla 1).
Figure 2. Pulmonary function dispersion over BML. Upper cancel) WHVC dispersion over BMI, and tendenev line, shows a direct associaten. Lower cancell) WHEVI dispersion shows direct association with BMI. Weight for specific age distribution was: 14% (n=2) of patients below percentile 3; 35% (n=5) of patients in the 3-10 percentile intervals; 7% (n=1) of patients in the 10-25 interval; 14% (n=2) in the 25-50 interval; 21% (n=3) in the 50-75 interval, and 1 patient 7% in the 75-90 interval. There were no patients over the 90 percentile. DISCUCION Results demonstrated correlation between BMI and Lung Function, indicating that lower nutritional status is related to lower FEVj and CVF values. Although causality cannot be inferred from this study, it is possible to affirm that approximately 30% of pulmonary function can be explained by nutritional pattern (Tabla 1). Similar correlation had been revealed before in larger studies with growth and nutritional indexes (19, 27). We found that this correlation persists even in groups of patients with severe nutritional deficit, as exposed in this analysis. Table 1 Shows a linear regression for BMI = %FEVr The correlation coefficients were calculated according to a bidimensional analysis. This group of patients exhibited a poor nutritional status, even lower than expected in patients with CF. (18-23) However, this finding is in agreement with high malnutrition prevalence related to Colombian pediatric population (28), suggesting an addition of community-associated risks (i.e. dietary deficit, recurrent enteroviral infection) and CF-associated factors contributing to weight loss and patients deterioration. According to other authors, severity of these notorious deficits would be also linked to variables that are beyond the scope of this study, such as genotypic characteristic, age at time of CF diagnosis and chronic P. aeruginosa infection. (10, 13, 29) Naturally, pulmonary function showed a parallel deterioration in this group. Despite the coexistence of multiple variables, BMI control and malnutrition treatment offer an important possibility to improve pulmonary conditions, mainly in these cases in Colombian Caribbean cities, where early diagnoses are difficult due to CF low incidence (3,6) and socioeconomical conditions are complex (30). Thus, results coincided with several reports suggesting that groups of patients with CF require special attention to nutritional therapy (18-19, 23, 27). According to these results, increasing BMI until percentile 50 or Z-score = 0, would improve pulmonary function in approximately 30% from baseline. Unfortunately approaching to optimal weight and height in children with CF has shown to be difficult, even with aggressive treatments (23). Due to singular economical conditions in the Colombian Caribbean Coast, considered as one of the poorest in Colombia (29), a nutritional strategy should be based on general guidelines, like those implemented successfully in Antioquia, another Colombian region (31), in order to supply intake deficits that do not correspond to the phy-siopathology of CF. Naturally, it is necessary to adjust these strategies adding components to supply special requirements for patients with CF, related principally to pancreatic insufficiency (11). Funding: Universidad de Cartagena. Interest Conflict: None. REFERENCIAS (1) Rosenstein B, Cutting G. The Diagnostics of Cystic Fibrosis: a consensus. J Pediatrics 1998; 132(4): 589-95. Available at: http:// www.ncbi.nlm.nih.gov/pubmed/9580754. [ Links ] (2) Ratjen F, Dõrin G. Cystic Fibrosis. The Lancet 2003; 361(9358): 681-9. [ Links ] (3) World Health Organization, Human Genetics Program. The molecular genetic epidemiology of cystic fibrosis. Report of a joint meeting of WHO/ECFTN/ICF(M)A/ECFS 2002. Available at: http://www.cfww.org/docs/who/2002/who_hgn_cf_wg_04.02.pdf [ Links ] (4) Scotet V, De Braekeleer M, Roussey M, Rault G, Parent P, Dagorne M et al. Neonatal screening for cystic fibrosis in Brittany, France: assessment of 10 years' experience and impact on prenatal diagnosis. The Lancet 2008; 356 (9232): 789-94. [ Links ] (5) Pérez M, Luna M, Pivetta O, Keyeux G. CFTR Gene Analysis In Latin American CF Patients: Heterogeneous origin and distribution of mutations across the continent. JCyst Fibros 2007; 6 (3): 194-208. [ Links ] (6) Raskin S, Pereira-Ferrari L, Caldeira F, Abreu F, Marostica P, Rozov T et al. Incidence of cystic fibrosis in five different states of Brazil as determined by screening of p.F508del, mutation at the CFTR gene in newborns and patients. J Cyst Fibros 2008; 7 (1): 15-22. [ Links ] (7) Heijerman H. Infection and inflammation in cystic fibrosis: A short review. J Cyst Fibros 2005; 4: suppl 3-5. [ Links ] (8) Cui L, Aleksandrov L, Chang X, Hou Y, He L, Hegedus T, et. al. Domain Interdependence in the Biosynthetic Assembly of CFTR. J MolBiol 2007; 365 (4): 981-94. [ Links ] (9) Rowe S, Miller S, Sorscher E. Cystic Fibrosis. N Engl J Med 2005; 352: 1992-2001. [ Links ] (10) Mckone E, Emerson S, Edwards K, Aitken M. Effect of genotype on phenotype and mortality in cystic fibrosis: a retrospective cohort study. The Lancet 2003; 361 (9370): 1671-6. [ Links ] (11) Taylor C, Aswani N. The Pancreas in cystic fibrosis. Paediatr Respir Rev 2002; 3 (1): 7781. [ Links ] (12) De Boeck K, Wilschanski M, Castellani C, Taylor, Cuppens H, Dodge J et al. Cystic fibrosis: terminology and diagnostic algorithms. Thorax 2006; 61 (7): 627-35. [ Links ] (13) Valenza G, Tappe D, Turnwald D, Frosch M. Kõnig C, Hebestreit H et al. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J Cyst Fibros 2008; 7 (2): 123-7. Available at http://www.ncbi.nlm.nih.gov/pubmed/17693140 [ Links ] (14) Rosenbluth D, Wilson K, Ferkol T, Schuster D. Lung Function Decline in Cystic Fibrosis Patients and Timing for Lung Transplantation Referral. Chest 2004; 126 (2): 412-9. [ Links ] (15) Williams EM, Madgwick R, Thomson A, Morris M. Expiratory Airflow Patterns in Children and Adults with Cystic Fibrosis.Chest 2002; 117 (4): 1078-84. [ Links ] (16) American Thoracic Society, European Respiratory Society. Ats/Ers Task Force: Standardization of Lung Function Testing: General considerations for lung function testing. Eur Respir J 2005; 26: 153-61. [ Links ] (17) Vilozni D, Bentur L, Efrati O, Minuskin T,Barak A, Szeinberg A et al. Spirometry in Early Childhood in Cystic Fibrosis Patients.Chest 2007; 131 (2): 356-61. [ Links ] (18) Cystic Fibrosis Foundation Patient Registry 2007. Annual Data Report 2006. Available at: http://www.cff.org/. [ Links ] (19) Konstan MW, Butler SM, Wohl ME,Stoddard M. Matousek R, Wagener JS et al. Growth And Nutritional Indexes In Early Life Predict Pulmonary Function In Cystic Fibrosis. J Pediatr 2003; 142 (2): 624-30. [ Links ] (20) Kin S, Nyulasi, Kotsimbos T, Wilson J.Nutritional status and quality of life are associated in adults with cystic fibrosis.Nutrition 2008; 24: 497-514. [ Links ] (21) Ortiz-Moncada R, Ruiz-Cantero MT, Álva-rez-Dardet C. Análisis de la Política de Nutrición en Colombia. Rev. Salud Pública 2006; 8 (1): 1-13. Available at http://www.scielosp.org/scielo.php?script=sci_arttext_&_pid=S0124-00642006000100001_&_lng=pt_&_nrm=iso_&_tlng=es [ Links ] (22) De Onis M, Onyango AW, Borghi A, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization 2007; 85 (9): 660-7. [ Links ] (23) Sinaasappel M, Stern M, Littlewood J, Wolfe S, Steinkamp G, Heijerman HG et al. Nutrition in patients with cystic fibrosis: a European Consensus. Journal of Cystic Fibrosis 2002; 1: 51-75. [ Links ] (24) American Thoracic Society, European Respiratory Society. Ats/Ers Task Force: Standardization of Lung Function Testing: Standardization of the measurement of lung volumes. Eur Respir J 2005; 26: 511-22. [ Links ] (25) American Thoracic Society, European Respiratory Society. Ats/Ers Task Force: Standardization of Lung Function Testing: Standardization of spirometry. Eur Respir J 2005; 26: 319-38. [ Links ] (26) Universities Occupational Safety And Health Educational Resource Center, Centers For Disease Control, Prevention National Institute For Occupational Safety And Health. NIOSH Spirometry Training Guide. NIOSH Grant Number 2003. T15-OH-07125. Available at: http://www.cdc.gov/niosh/docs/2004-154c/pdfs/2004-154c-intro.pdf [ Links ] (27) Peterson ML, Jacobs DR, Milla C.E. Longitudinal Changes in Growth Parameters Are Correlated With Changes in Pulmonary Function in Children With Cystic Fi-brosis. Pediatrics 2003;112: 588 -92. Available at http://www.ncbi.nlm.nih.gov/pubmed/12949289 [ Links ] (28) Alcaraz G, Bernal C, Cornejo W, Figueroa N, Múnera M. Nutritional status and living conditions in children in an urban area of Turbo (Antioquia, Colombia). Biomédica 2008; 28(1): 87-98. http://www.ncbi.nlm.nih.gov/pubmed/18645664 [ Links ] (29) Sophia S, Wang S, O'Leary LA, Fitz Simmons SC, Khoury MJ. The impact of early cystic fibrosis diagnosis on pulmonary function in children. J Pediatr 2002; 141: 804-10. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12461497. [ Links ] (30) Ojeda G, Ordónez M, Ochoa L. Salud sexual y reproductiva en Colombia. Encuesta Nacional de Demografia y Salud. Bogotá. Profamilia 2005: 267-71. [ Links ] (31) Bernal C, Velásquez C, Alcaraz G, Botero J. Treatment of Severe Malnutrition in Children: Experience in Implementing the World Health Organization Guidelines in Turbo (Colombia). Journal of Pediatric Gastroenterology and Nutrition 2008; 46: 322-8. [ Links ]