INTRODUCTION
8-10% of girls and 2-3% of boys will have symptomatic UTI before the age of seven, being more frequent in males in the first three months of life and producing a progressive increase with predominance of girls from the first year of life 1.
In the first 4-6 months of age, it is more frequent in the male sex, with a boy / girl relationship with a 4/1 ratio. After 3 years, the UTI is much more frequent in girls, so that 5% of school girls suffer from it, with a girl / boy ratio greater than 10/1 2.
UTIs are one of the most common bacterial infections, approximately 5-14% of pediatric emergencies are due to this cause 3,4.
Finally, we can say that its incidence is related to age and sex. Existing epidemiological studies are very heterogeneous, with variations between one and the other regarding the definition of UTI, the populations studied and the methodology used for the collection of the urine samples. On the other hand, children with UTI, especially the smallest ones, present a nonspecific symptomatology, which sometimes makes the UTI be undetected 5.
The UTI encompasses a heterogeneous group of conditions that their commonality is the presence of bacteria in the urine. Urinary tract infection (UTI) is defined as the invasion, colonization and bacterial proliferation of the urinary tract, which can compromise from the bladder to the renal parenchyma.
In the same way, we can classify it according to its location, presence or absence of complications, and degree of recurrence.
Location:
Upper UTI:
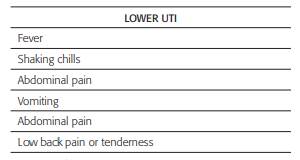
Acute pyelonephritis: It is characterized by fever> 38.5 °C associated with signs of inflammation such as increased acute phase reactants such as C-reactive protein, erythrocyte sedimentation rate and is a potential risk for kidney damage with possible cortical scars 6.
Lower UTI:
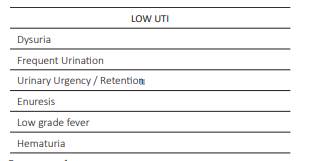
Cystitis: It occurs when there is localized involvement in the urinary bladder, fever usually does not occur, with the presence of voiding symptoms such as dysuria, frequency and absence of lumbar pain. Other than that, it does not represent a risk of kidney damage 2.
Urethritis: it is a pathology that occurs infrequently in the pediatric age. It can be manifested in the same way with voiding symptoms without fever and, occasionally, exudate may occur, which is more frequent in adolescence. In younger children, it can be part, practically indifferent from the clinic, of balanoposthitis, or of vulvovaginitis.
According to its clinical presentation and / or renal structural damage
Uncomplicated UTI: characterized by absence of alteration in the structure or function of the urinary tract evidenced by imaging studies 6. These symptoms correspond to low UTI, and an uncomplicated UTI is characterized by the following:
Febrile or fever
Age > 2 years
Urinary symptoms
No toxic appearance
No associated co-conditions
Little or no elevation of acute phase reactants
Complicated UTI: alteration in renal function or damage at the structural level, corresponding to high UTI, usually occurs:
Fever> 38.5.
Infants.
Toxic aspect.
Antecedents of UTI and / or associated comorbidities.
Leukocytosis and increased acute phase reactants.
According to its recurrence: Reinfection, relapse and recurrent.
Reinfection: Recurrent UTI due to a germ that may be the same or another but with an interval greater than 6 weeks.
Relapse: recurrent UTI due to the same germ but with a time interval of less than 6 weeks.
Recurrent: defined as 3 or more episodes of low UTI or 2 or more pyelonephritis in a period of 1 year.
It is important to be clear about the definition of asymptomatic bacteriuria since it occurs very frequently and can sometimes be confusing as to the initiation or not of antibiotic therapy.
Asymptomatic bacteriuria: asymptomatic patient with absence of elevation of acute phase reactants and inflammatory markers and positive urine culture 7.
ETIOLOGY
The etiologic agent of UTIs in Pediatrics is very similar to that of the rest of the population, however the etiological agent most frequently isolated in UTI continues to be Escherichia coli, occurring in approximately 76-90% of the episodes, followed by other germs such as Klebsiella 0,5-8%, Proteus 0,5-6%, Staphylococcus spp. 1-5%, And Pseudomona spp. 2%, which are related to some risk factors of each patient 8.
PATHOGENY
The route of infection is almost always ascending, from microorganisms from the intestine that are found in the perineal area and ascend through the urethra to the bladder 2. Some strains of E. coli have adhesion factors on their surface that facilitate union to the bladder mucosa and the subsequent development of UTI.
This ability of some microorganisms to adhere to the cells of the urinary epithelium is the main factor that contributes to the initial colonization of the mucosa. Adhesion to epithelial cells occurs due to filamentous structures that are located in the capsule of bacteria called fimbrias or Pili.
Children who have an abnormality of their excretory pathways that cause an obstruction to urinary flow or a vesicoureteral reflux, have a much higher risk of infected urine reaching the kidney and causing pyelonephritis 9.
Hematogenous spread to the urinary system is a rare cause of UTI, this can occur in newborns and children with immunodeficiency. In this case the related germs are group B Streptococcus, Staphylococcus aureus, Candida and Salmonella can cause pyelonephritis through of the hematogenous route.
One of the defense mechanisms to prevent bacterial growth in the urinary tract is basedon urination itself, which leads to a continuous desquamation of the superficial epithelial cells to which the bacteria are attached. That is, the bacteria are washed out of the bladder by repeated urination and the sterility of the urine depends to a large extent on the absence of interruption of the urinary flow 5.
PREDISPONENT FACTORS FOR UTI
Predisposing factors for the development of UTI are urinary tract anomalies that favor the slowing of the urinary flow, including VUR, phimosis in male infants, lower urinary tract dysfunction and constipation, as well as instrumentation. of the urinary tract, the neurogenic bladder and nefrourolithiasis. Some studies show the protective factor of prolonged breastfeeding for more than six months 5.
Finally, there are risk factors for the presence of permanent renal damage, such as in patients with high-grade vesicoureteral reflux and recurrent UTI. There is some evidence, but with contradictory data, in relation to the age of the patient and the delay in starting treatment as risk factors for the appearance of scars 10.
Predisposing factors for UTI in the pediatric age: White race in both sexes, Absence of breastfeeding, Male sex during the first year of life, Constipation Presence of renal anomaly, Vesicoureteral Reflux, Arterial hypertension, Pole failure UTI, Background Lip synechia Pathological phimosis Frequent bladder catheterization 4,
CLINIC
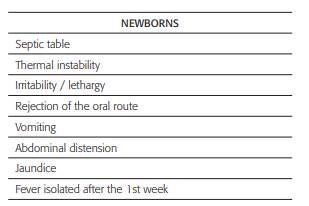
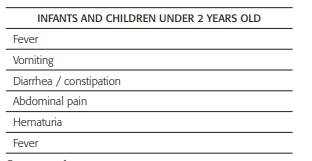
The clinical presentation of UTI varies with age. In infants, infection is usually diagnosed later due to non-specific initial signs, such as fever, in addition to the inability to express symptoms or localize pain. Older children can usually manifest the first symptoms of UTI, such as dysuria or abdominal pain, and therefore the infection can be identified slightly earlier than in infants 11-13.
UTI RISK ESTIMATION
Neonates and children younger than 24 months who present with UTI often present with fever. Fever is a common and nonspecific symptom for which physicians should consider UTI as a possible etiology, especially when there are no other obvious signs or symptoms to suggest another diagnosis.
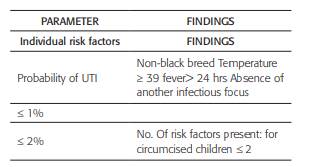
The probability of a UTI increases as the number of risk factors, or findings, increases. The risk factors for urinary tract infection in female infants include the white race, age less than 12 months, temperature higher than or equal to 39°C and absence of another source of infection.
The probability of developing UTI in male patients is influenced by whether or not they present circumcision. In children under 24 months without circumcision, the risk of UTI without any additional risk factor exceeds 1%. The probability of UTI in infants is related to the presence of some risk factors which are presented in the following tables:
Table 5 Probability of UTI in female infants according to the number of findings
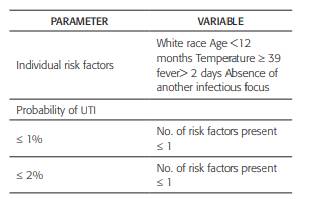
Source: reference 4.
DIAGNOSIS
It is considered necessary to obtain a urine sample to confirm or rule out a suspicion of UTI, especially when there is a febrile condition without a clear focus 7,14.
We must suspect a UTI when presenting a pathological uroanalysis. This must be confirmed by the uroculture which is considered the gold standard test.
There are situations in which bacteria may be present in the urine without causing infection and inflammation, this is defined as asymptomatic bacteriuria.
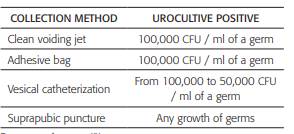
In neonates and children under 24 months of age, collection of urine with a collection bag tends to be contaminated; therefore, bladder catheterization (catheter) should be used for urine sample collection for uroanalysis and urine culture. Observational studies estimate a high risk of contamination and low positive predictive value of urine cultures with a collection bag. Only those cases that the results of the uroanalysis, whose sample was taken with a collection bag when it is not pathological, should be taken into account 15.
Technique: Vesical catheterization
Advantage: It can be used for initial urine culture
Disadvantages: Pain and discomfort Technique: Collection bag Advantage: No discomfort and pain
Disadvantage: More time, Pathological results must be confirmed by urine culture
INTERPRETATION OF UROANALYSIS
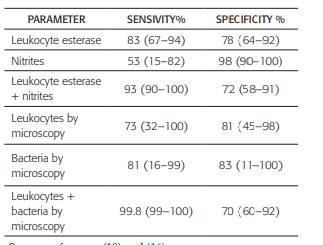
Urine dipstick can be used to analyze the presence of leukocyte esterase (a marker of white blood cells) and nitrites (a marker of some gram-negative bacteria). However, it does not detect the concentration of leukocytes, therefore microscopy should be used to evaluate this and other parameters, and in this way improve sensitivity. Pathological ≥5 leukocytes / field in non-centrifuged urine and ≥ 10 leukocytes / field in centrifuged urine is considered pathological.
The nitrite test has little sensitivity in neonates since they empty their bladders frequently, often before the required 4 hours for gram- negative bacteria to form nitrites. As such, the absence of urinary nitrites does not rule out UTI 6. Another parameter that is currently used is the presence of bacteria in the gram of urine without centrifuge which has a sensitivity of 90.3% and a specificity of 93.5%
INTERPRETATION OF THE UROCULPT
The results must be interpreted carefully. Consider the number of colony forming units (CFU) per milliliter, type of bacteria species identified, and the time elapsed in processing the urine sample.
COMPLEMENTARY STUDIES AT UTI
Kidney and urinary tract ultrasound:
It should be done to all patients with febrile or afebrile UTI, it is a comfortable, non-invasive, economical method that does not emit radiation. However, this only serves to evaluate the anatomy of the urinary tract and it has no use for the diagnosis of vesicoureteral reflux, pyelonephritis and much less renal scars 16,17
Renal scintigraphy with DMSA:
It is the gold standard for the diagnosis of acute pyelonephritis and the presence of scars and their extension, it should be indicated when a clinical pyelonephritis is diagnosed, alterations in renal ultrasound and recurrent UTI. This should not be done at the time of infection since there is a high percentage of children under 5 years of age who are positive; for this reason, it is recommended that it be performed 4 to 6 months after the acute event with the objective of showing renal scars 18.
Voiding cystourethrography:
It is the main imaging study for the diagnosis of vesicoureteral reflux and dysfunctional elimination syndrome. It is not recommended to perform it after 3 years of age since it is unlikely that at this age this is the cause of a first episode of UTI, and that this is secondary always be performed in UTI treated with negative urine culture
HOSPITALIZATION CRITERIA
Regarding the management of UTIs, it is important to establish taking into account the evolution and the presence of some risk factors that patients should be treated in-hospital.
TREATMENT
Generally, the treatment of a UTI starts before clinical suspicion and, empirically, this will depend clearly on the evolution, presence of complications and local epidemiology according to studies carried out in each institution taking into account types of isolated germs and resistance profile to antibiotic therapy 19.
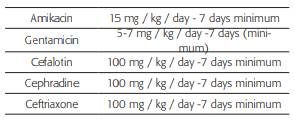
Table 10 Empiric antibiotic therapy of first choice in complicated UTI neonates younger than 4 months to vesicoureteral reflux. This study should Age less than three months
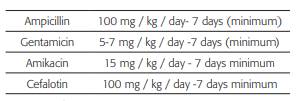
Source: authors.
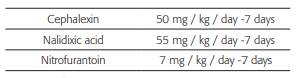
ANTIBIOTIC PROPHYLAXIS
Indications:
Grade III vesicoureteral reflux, Pedalcalyceal ectasias, Neurogenic bladder, recurrent UTI, less than 2 years with febrile UTI until studies are completed.
Antibiotics for antibiotic prophylaxis: Cephalexin 15 mg / kg / day Nitrofurantoin 25 mg/ kg / day Nalidixic acid 30 mg / kg / day Trimetropin sulfamethoxazole 2 mg / kg / day Antibiotic prophylaxis should be performed with 30% of the therapeutic dose at night, and should be used continuously at least until the relevant studies are done and the Etiology is clear.