INTRODUCTION
Flexor tendons injuries in children represent a diagnostic and therapeutic challenge for surgeons. These injuries can go unnoticed and rehabilitation is difficult, but good results are achieved after treatment.
The incidence of these lesions in children has been estimated at 3.6 / 100,000 children per year 1. Flexor zones II and V are the most commonly affected and it is very strange to see these lesions in children younger than two years old, although they have been described in newborns occurring during emergency caesarean deliveries 2. "Buds" or higher incidence peaks have also been observed in holidays times, in which children tend to manipulate sharp instruments 2.
The most common trauma mechanism is caused by cutting glass, followed by sharp object injuries (knives). Associated neurological injuries are commonly found in III and V flexor zones, and they are not frequently associated with finger fractures or extensor tendon injuries 1. These injuries are more common in men than in women, and most commonly affect the right hand 1,3.
The objective of this study is to describe the clinical features of a series of patients with flexor tendon injuries of the hand and their functional results in short term.
MATERIALS AND METHODS
This is a retrospective study of pediatric patients with flexor tendon injuries of the hand, during a period of two years from April 2015 to April 2017, in the hospital base of the study.
Inclusion criteria were age between 0 and 16 years, with a diagnosis of flexor tendon injury made by a specialist, and a minimum follow-up of 10 weeks.
The variables analyzed were: age, gender, laterality, trauma mechanism, affected flexor zone, associated injuries and, in short term, the functional outcome were assessed with the Total Active Motion (TAM) scale of the American Society of Surgery of the Hand (ASSH).
The study was approved by the medical ethics committee of the Hospital.
RESULTS
Twenty-two (22) patients were included in the study. The average age was 7.28 years 1-16. Fifteen patients (71.4%) were men. The right limb was affected in twelve cases (52.4%), and there was a case with bilateral involvement. The most common trauma mechanism corresponded to sharp trauma (15 cases, 71.4%), partly produced by broken glasses, glass windows or paintings. The sharp mechanism traumas were caused by knife (13%) in three cases, associated with neglected or aggressive acts. Table 1.
Table 1 Characteristics of patients in the study
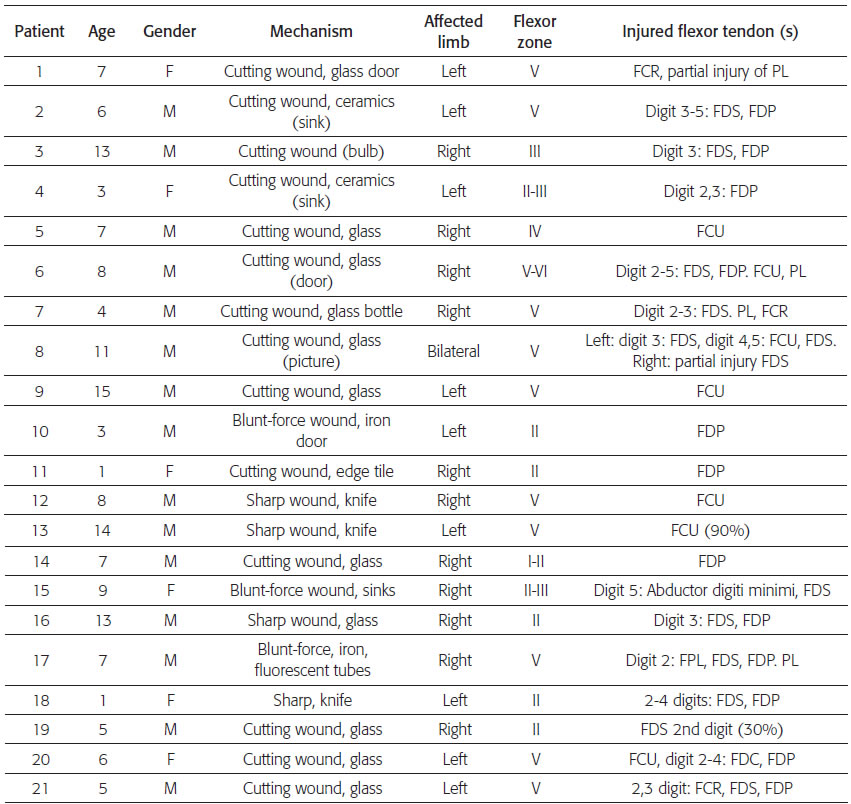
M: male, F: female. FCR: flexor carpi radialis, PL: palmaris longus, FDS: flexor digitorum superficialis, FCU: flexor carpi ulnaris, FDP: flexor digitorum profundus, FPL flexor poflicis longus.
Affected flexor zones
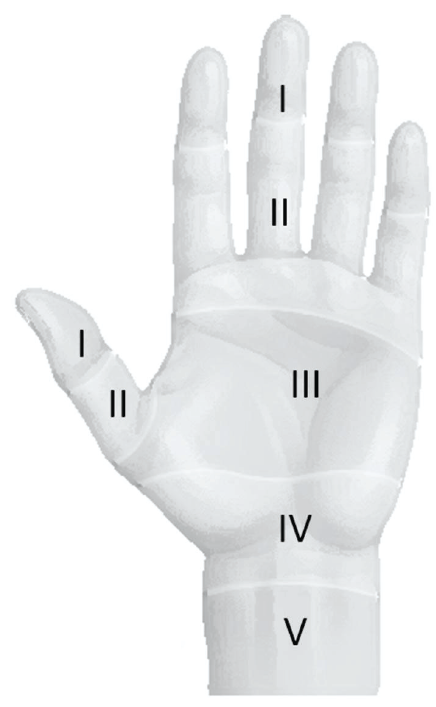
Flexors zones of the hand are the same in adults and children. Figures 1-2. 4.
The most affected flexor zone in this series was the V in eleven cases (52.3%). The biggest of these traumas were produced by a high-energy cutting mechanism, mainly accidentally broken pottery and glass. The zone II was the next most affected with a total of 8 patients (38%). In these there were also accidental injuries for broken glass or ceramic. The lesions in zone III corresponded to 14.2% of the population -three cases-, in zone I and in IV only a case of each (Table 1).
Injured flexors
There was a total of 65 documented lesions. More Injured tendons were the FDS and FDP. Regarding the FDS, there were 25 tendons injured in total (37%) in 12 patients. FDP was also injured 23 times in 11 patients. In 8 patients both tendons were found injured. Of the remaining patients who took only superficial or deep flexor tendon injury, these lesions were isolated or with other different injuries.
The most frequently injured tendon after previous was the FCU in 7 patients (10%). The other injured tendons PL-four cases-, FCR - three cases-, occurred sporadically. There were five cases of partial lesions (7.4%).
Primary repair of injured tendons was performed during admission. Lesions were repaired fully in 91% of patients. In one patient (case 19) only deep tendons were repaired due to age and the difficult reparation in the affected zone. In another patient (case 15) only muscle ADQ was repaired, leaving the superficial tendon injury unrepaired.
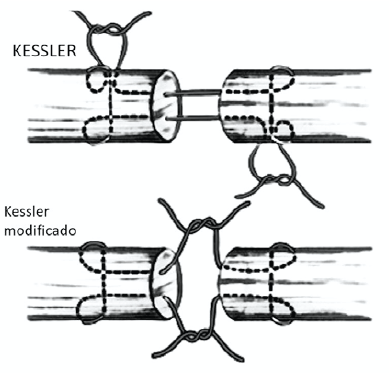
The most commonly used technique was Kessler knot in twelve patients (54%), followed by Adelaide knot in four patients (18%) and double Kessler in 4 cases (18%). Figure 3, 4.
With the remaining patients, in one case (4%) nonabsorbable polypropylene (Prolene) was used to repair a myotendinous injury with simple points 12; in another patient, a crossed suture was used to repair a intrinsic muscle injury of the hand (case 15), and in another a single point was used in a partial tendon injury (case 20). There were two cases (9%) of tendinous reinsertion: one with pull-out through bone tunnels with button (case 14) and another case with suture to the palmar plate (case 19).
Epitendinous continuous suture was used in 7 cases (32%).
The most commonly used suture was Prole-ne® in 17 cases (81%), polydioxanone (PDS) in three (14%) and Vicryl (polyglactin 910) in a case (4%). The size of the suture varied between 4-0 and 5-0, 5-0 being used in patients under 5 years with injuries in zone I-II.
Associated injuries
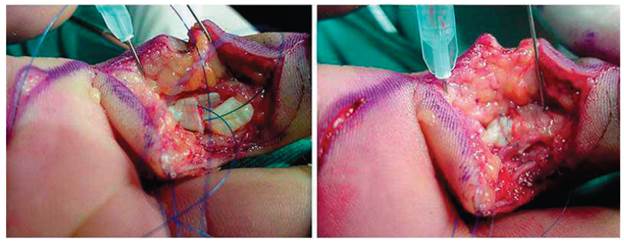
There were associated injuries in 19 patients (86%), most of them corresponding to nerve injury, followed by vascular lesions. There was a total of 27 nerve injuries, with ulnar nerve injury in 7 cases (26%), being complete in 6 cases (22%) in zones IV and V, and a case with partial injury of 80% in zone V. The median nerve had complete injury in 4 cases, all of them in zone V. There was a case of partial injury to the superficial branch of the radial nerve. The remaining fifteen nerve injuries were partial or complete digital collateral radial (case 9) and ulnar (case 6) injuries in zone I to the zone III. Figure 5, 6.

Figure 5 Flexor tendon injury in zone V in ulnar border of the wrist with ulnar artery and nerve injury
Nerve repair was done in all patients with epineural technique using suture size between 7- 0 and 9-0. Different types of suture were used: ethilon® in 20 cases and Prolene® in 7 cases. There were vascular injuries in 7 cases, six of them involving the ulnar artery. In four cases no vascular repair was done because there was found extensive arterial thrombosis and previous ligature of the artery. Arterial repair was performed in two cases with microsurgical techniques using Ethilon 8- 0 and vascular Prolene 7-0.
The remaining case presented a digital artery injury that was repaired.
All patients were immobilized with a plaster splint with metacarpophalangeal (MCP) flexion and wrist in a neutral or slightly wrist flexion. One patient with a FPL injury was immobilized with a thumb spica. surgery.
Immobilization time averaged 4.7 weeks for all patients (3-7 weeks). Then physical therapy without immobilization was started. In two cases, children over 12 years old, the splint was continued night-only for 2 weeks more.
After removal of the splint emphasis was placed on improving the flexion and extension movement range with home therapy and physical therapy. No formal rehabilitation protocol was followed.
Functional results
TAM (Total Active Motion) score and the ASSH (American Society of Surgery of the Hand) were used to evaluate the functional outcome of the patients. The score considers the range of active mobility compared to contralateral -uninvolved side-, as a percentage. An excellent result is considered when equivalent to the contralateral, good if greater than 75% of the contralateral, fair between 50 and 75%, poor below 50% and appalling if worse postoperatively.
Only 17 patients were evaluated with the minimum follow-up. The remaining five did not return to control. There was a good result in 14 patients (82.3%). Of the remaining three cases: one had an excellent result, one had a poor one and another an appalling one.
The poor result corresponded to a patient with injury to the fifth finger FDP, with little adherence to the immobilization, and who presented an inability to flexion, with a movement of 43% compared to the contralateral during follow-up at six weeks. He was scheduled for surgical exploration, but did not return to control. The appalling result corresponded to a 7-year old patient with an FDP injury of the second finger of the right hand in zone I. At three months, he had a flexion contracture of 70 degrees of DIP and PIP joint and a hyper-trophic scar. Surgical exploration with likely tenolysis or graft tendon was decided, but the patient did not return to control.
DISCUSSION
Flexor tendon injuries in the pediatric population are produced generally by cutting instruments including glass separators used as doors 1,5. In our series, more cases were produced by broken glasses, and also broken ceramic sink was the cause of injury in three cases. There was no correlation between patient age and the predominant trauma mechanism. For example, in three patients injured by sharp mechanisms, the younger was a one-year old and the oldest was 14 years. Causes in these cases were unintentional or accidental activities.
In general, these patients had the classic signs of flexor tendon injury with loss of biotenode-sis in the affected region of the injured finger or hand. The diagnosis of associated injuries was made during the initial assessment, or suspicion as described by some authors 6, or during the surgical procedure.
In a patient with flexor injury in zone II only FDP was repaired. In the rest of the patients, all tendon injuries were repaired. Navali 7 reported that repair in zone II can be performed in both tendons regardless of age because, due to growth and rapid repair, adhesions and contractures are unlikely.
The repair technique used was double or single Kessler in most patients. One case with Adelaide knot was made. No direct relationship was found between the number of steps of the suture and increase of tendon rupture, which is consistent with other studies 7,8. However, Muradian 9 found an inverse relationship between the type of suture -double or triple-, and increase in rupture incidence.
Other authors recommend simple techniques and the number of strands depends mainly on the axial surface of the tendon subject to repair 10. The epitendinous suture was used in seven cases, out of which three were in the zone V, being its use low respect to the existing literature 1,5,10. Four other patients had injuries in zone II; not finding postoperative adherence in any of them. In literature, the use of epitendinous suture is recommended in all flexor tendon repair 5. However, in cases where epitendinous suture was not made, only one rupture occurred, which cannot be attributed to lack of suture and probably was associated with poor adhesion to immobilization and rehabilitation. In other literature reports, the epitendinous suture is used in less than 50% of the population 1,3,5. The importance of epitendinous repair in flexor zone 2 is extrapolated from adult injuries.
It is worth highlighting the high number of injuries found in this study. In other case series evaluated, the maximum found was a hundred injuries in 47 patients 5.
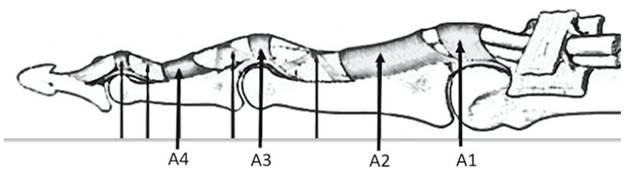
Associated lesions in all patients were repaired in the same surgical time. Thrombosed and poor-quality arterial injuries were not repaired. This work considered the associated injuries and they were repaired in most of the cases. In many cases, they go unnoticed and are not repaired 1. In this series we found a case of the A4 pulley repair without complications as rupture or tendinous adherence. Pulley repair is important because of its role in finger flexion biomechanics 11,12.
There was a good result in most of the patients. Two cases had poor outcomes, one with adherences and fibrosis postoperative and another who abandoned the immobilization. The overall results are consistent with the series published reporting good results in these patients 5,10.
The postoperative scheme used consisted of initial immobilization with subsequent withdrawal and mobilization therapy, where parents played a very important role. About the scheme used, it is consistent with other authors in immobilization for a minimum of four weeks 6 to avoid activities not supervised that may lead to new tendon rupture.
Loss in follow up is common and lack of an effective and regular physical therapy service in our environment makes it very difficult to establish early-mobilization protocols despite early success reported with these activities 13. A complete four-week immobilization protocol followed by rehabilitation is the most accepted and supported by the literature for pediatric patients 14.
CONCLUSION
Flexor tendon injuries in children require a high level of diagnostic suspicion. Surgical exploration under anesthesia and primary repair are recommended for a proper approach to these injuries. A non-absorbable and aged-sized suture is necessary for repair, and a 4 to 6 weeks of immobilization must be guaranteed. Rehabilitation can be started after immobilization and parents should be involved in this phase of the follow up. Good results are obtained in most patients.