INTRODUCTION
Morbid obesity is a multifactorial chronic disease associated with physical and psychological complications which negatively affects the quality of life of the sufferer, increases comorbidity and reduces life expectancy 1. It is calculated that one billion adults worldwide are overweight and more than 300 million are obese; 42 million children are overweight with a high probability of being obese in adulthood 2. In Colombia, according to data from the survey 'Situación Nutricional en el 2010' (The Nutritional Situation in 2010'), one in every two Colombians between 18 and 64 years of age are overweight; the reason for which obesity is defined as a public health problem 3,4, a problem from which the city of Neiva is not exempted.
People with obesity, as well as suffering from a chronic disease, risk comorbidities and premature death, suffer from social stigma which affects quality of life in the personal, family, sentimental, educational and work domains as well as in less obvious spheres such as barriers in terms of access to transport, recreational activities and the purchasing of clothes 5. In order to confront this condition, losing weight is recommended, for which there are two main methods. Firstly, a change in lifestyle through behavioral treatment focused on self-monitoring, the control of stimuli for people who are overweight or obese 6-8 and physical activity 9 as part of a public health model and secondly, bariatric surgery and its various surgical techniques 10-12.
Surgical treatment is the last step in treating obesity. In certain patients whose medical treatment, modifying their lifestyle and various diets was unsuccessful, a therapeutic surgical approach becomes effective, taking into account the potential for successful treatment translated into weight loss, with the possibility of being sustained over time 13.
Patients who have been treated with bariatric surgery loose at least 50% of excess weight, associated with the reduction of the prevalence of comorbidities associated with obesity such as high blood pressure, diabetes mellitus, dyslipidemias and cardiovascular disease. This therefore, increases life expectancy 16, as well as improved mental 17,18, physical and social wellbeing of patients 19,10.
In the SF-36 quality of life measures in obese people are negatively affected; the morbidly obese (BMI>48) present impaired physical, social and role functions, poor perception of general health and greater bodily pain than those with mild obesity (BMI>29) or moderate to serious obesity (BMI>34.5), who are also affected by the emotional and social impact. 50% of obese people suffer from some type of bodily pain, above all lumbar pain, headaches, chest pain and pain in the lower limbs. These patients have a significantly lower score in all aspects of quality of life, the most striking being the effect on perceived physical, social and health functionality 10,20.
The importance of assessing changes in the perception of quality of life of patients before and after bariatric surgery is relevant, given that for the patients it allows them to recognize the lifestyle which leads them to obesity and the urgent need to change their previous behavioral patterns and continue reinforcing the benefits generated by the bariatric surgery. It also allows them to recognize the potential changes in their personal, family, work and social lives. For multidisciplinary health teams, quantifying the perception of the quality of life of these patients allows them to assess the effectiveness of the procedure, the degree of satisfaction and the appropriation of healthy behaviors and lifestyle, not only weight loss 21.
The aim of the investigation is to determine the perception of quality of life of patients with type I obesity with metabolic disorder and types II and III, six months after undergoing bariatric surgery in the Hernando Moncaleano Perdomo University Hospital between September 2011 and March 2015.
MATERIALS AND METHODS
The investigation methods involved quasi-experimental research, clinical series and before-and-after studies 22. The study comprised of 87 patients who had a body mass index greater than 36 kg/m2 or classified as type I obesity with metabolic disorder and types II and III who have undergone bariatric surgery, using the following surgical techniques: bypass in 76.6% of patients, sleeve in 20.8% and balloon in 2.6%.
The sample consisted of 77 patients who fulfilled the inclusion criteria. Patients were selected by the multidisciplinary team of Hernando Moncaleano Perdomo University Hospital. All met the requirements and characteristics to undergo bariatric surgery and accepted voluntarily to be a participant in this investigative process, as well as each participant accepting and signing the informed consent. Exclusion criteria covered patients with mental illnesses and of difficult geographic location. The sample consisted of 83% women and 17% men with an average age of 37 years with a standard deviation of 10 years. 73% of the patients resided in Neiva, 7% were from Pitalito, 7% from Garzón and the remainder from other municipalities in the state of Huila, Colombia. Regarding BMI after the surgery, the BMI of all patients was reduced by an average of 20 points, with a variation of 4.8. The project began in September 2011 with the bariatric surgery group of the Hernando Moncaleano Perdomo University Hospital and ran until 2015.
The SF-36 questionnaire, the Medical Outcomes Study, validated in Colombia, was used to determine a profile of the physical and mental state of health of the patients 23, this instrument has been demonstrated to be useful in both clinical practice and scientific investigation. The SF-36 has an estimated Cronbach α coefficient of > 0.9 for the scales of Physical Function, Physical Role and Emotional Role24. Before applying this instrument clinical interviews and explanations were carried out and a signature of informed consent obtained. To reduce bias, the implementation of the questionnaire was carried out by a single person with previous training 25, social and demographic data were also collected.
The data collection for the study was carried out on two occasions; before the bariatric surgery and then six months after the surgery. The statistical analysis included; creation of a database, qualification of the SF-36 questionnaire, calculation of measures of central tendency, dispersion and comparison of averages with the respective p-value, with α=0.05, Ho = pre-test average = post-test average measures tabulated with the program Epiinfo Version 7.1 2015 (26) and Excel.
The ethical considerations were based on the Código Deontológico de la profesión Médica dictated by Law 23 of 1981 27 (Code of Conduct of the Medical Profession), respecting the ethical principles of beneficence, non-maleficence, autonomy and fidelity for its implementation. In accordance with Resolution 8430 of 1993, this investigation is considered 'minimal risk' given that it is a prospective study where data collected through an instrument applied before and after the surgical intervention was used. Furthermore, the investigative process was guided by the Declaration of Helsinki, where respect for the dignity of human beings, the protection of their rights and wellbeing prevails and life, health, integrity, the right to self-determination, privacy and confidentiality of the personal information of the participants is protected. These tenets will remain registered in the informed consent which is completed before collecting information, is properly explained and understood by the patient and validated by the ethics committee of Hernando Moncaleano Perdomo University Hospital.
RESULTS
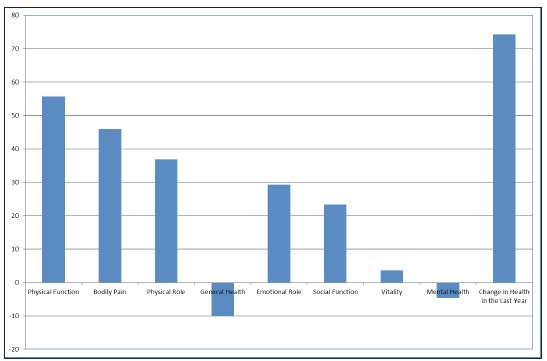
Table 1 and Graph 1 demonstrate that the physical function, six months after the bariatric surgery was significantly better compared to the previous situation of being limited in physical activity in daily life, in relation to personal care, walking, climbing stairs, carrying loads and undergoing moderate to intense physical effort.
Table 1 SF36 Evaluation of patients who underwent bariatric surgery
| Statistics | Physical Function | Bodily Pain | Physical Role | General Health | Emotional Role | Social Function | Vitality | Mental Health | Change in Health in the Last Year |
| BEFORE | |||||||||
| Mean | 30.6 | 36.5 | 58 | 50 | 61.4 | 48.3 | 46.4 | 47.3 | 15.0 |
| Standard Deviation | 15.3 | 21.7 | 13.5 | 13.8 | 16.2 | 20.5 | 11.8 | 10.2 | 22.8 |
| AFTER | |||||||||
| Mean | 86.3 | 82.4 | 94.9 | 39.9 | 90.6 | 71.6 | 50.1 | 42.6 | 89.3 |
| Standard Deviation | 14.4 | 22.3 | 13.6 | 10.6 | 15.5 | 25.8 | 15.2 | 12.3 | 22.0 |
| Difference | -55.7 | -46 | -36.8 | 10.1 | -29.2 | -23.3 | -3.6 | 4.7 | -74.3 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.093 | 0.010 | 0.000 |
Source: The Authors, 2015.
Source: The Authors, 2015.
Graph 1 Changein the quality of life in patients before and after bariatric surgery.
Similarly, after the surgery the intensity of bodily pain caused by excess weight reduced in intensity and there was a positive effect on work and home activities, leading to greater autonomy in the life of the patient.
Regarding the physical role, it was demonstrated that six months after the bariatric surgery the capacity to work and carry out daily activities was strengthened leading to an improvement in the desired output and overcoming limitations in activities as a product of the reduction in body weight.
After the surgery, an increase in the patients' usual social lives was seen. This is related to increased bodily autonomy, patients interacting more with their families and beginning to plan their futures in terms of education and work.
Table 2 Evaluation of patients who underwent bariatric surgery
| Statistics | Physical Health | Mental Health |
| BEFORE | ||
| Mean | 46.22 | 47.99 |
| Standard Deviation | 9.81 | 8.79 |
| AFTER | ||
| Mean | 73.69 | 67.47 |
| Standard Deviation | 10.24 | 8.92 |
| Difference | -27.5 | -19.5 |
| P value | 0.0000 | 0.0000 |
Source: The Authors, 2015.
Six months after the surgery the patients saw a reduction in their emotional problems, positively affecting both work and daily life as the amount of time dedicated to these activities increased with greater output and care placed on them.
DISCUSSION OF RESULTS
The 87 patients who underwent bariatric surgery who had a body mass index greater than 36 kg/m2 classified as type I obesity with metabolic disorder and types II and III saw changes in the perception of quality of life six months after the surgery.
It is also demonstrated that there is no association between the sociodemographic variables and showing physical and mental health problems related to obesity.
The subjective assessment of the patient on their state of health, future prospects and resistance to illness substantially decreased. This negative subjective assessment is probably explained by a greater probability of becoming unwell from viral diseases caused by immunosuppression such as flu, acute diarrheal disease and other viruses as well as other factors such as a poor body image and a feeling of physical exhaustion, eating disorders associated with the surgery such as bulimia and a loss of energy and a cold sensation. It is worth noting that this is a temporary sensation whilst homeostasis is reestablished.
Before and after the surgery, the patient has a reduced sense of vitality. They feel tired and exhausted at all times, probably because in the first months after the surgery, the weight loss has implied significant changes in diets and food consumption as well as the fact that bodily changes indicate an accelerated form of weight loss, implying a dynamic state in general.
Although the emotional aspect showed a significant improvement, mental health, as evaluated through depressive events, anxiety, loss of control of impulses and loss of wellbeing in general declined slightly. This is attributed to the physical changes produced by the surgery. Previously, these patients calmed anxiety through compulsive eating whereas this is no longer possible after the surgery given that the body can no longer receive the quantity of food it was previously accustomed to.
Changes to health in the last year, including surgical intervention and bariatric surgery are reported as being a significant change which positively affects the quality of life of patients.
In the area of physical health, it is shown that physical function, the physical role, the reduction in bodily pain and the assessment of bodily pain were positively affected after the bariatric surgery. Similarly, mental health had a positive change of 20% in terms of vitality, social function, emotional role, mental health and changes to health in the last year. This suggests significant changes in both physical and mental health, however not always in a positive direction. Negative effects associated with the radical body change and diet restrictions were also demonstrated.
Concerning the perception of an improvement in general health there were no significant changes. This could correspond to the fact that the instrument used did not evaluate other important changes and adverse effects which patients who underwent bariatric surgery also experienced.
The study succeeded in demonstrating that, in general, patients had a better perception of the quality of life in the various roles of daily life six months after undergoing surgery. A time period of six months between the surgery and the second assessment was chosen after taking into account that in previous studies this was the time period in which definitive results following the procedure can be seen, including the collateral effects.
The Hernando Moncaleano Perdomo University Hospital is a state institution in the city of Neiva which treats patients form a heterogeneous population in terms of their socioeconomic level. These characteristics allow the results to be extrapolated for the entire geographic region.
CONCLUSIONS
Based on the data collected in the study it was demonstrated that the change in the perception of an improvement in quality of life in patients who underwent bariatric surgery six months after the procedure is favorable with regard to both the physical role and the emotional role, as well as an improvement in bodily pain, vitality and general health.
Contradictions in the perception of physical and mental health are caused by the adjustment process to the surgery six months after the operation; given that it also includes the substantial adaptive changes in the body which reduce body mass index by 20 points.














