INTRODUCTION
Hypertension or high blood pressure (HBP) is a disease in which blood flows through blood vessels, or arteries at higher than normal pressures 1. This condition is one of the main risk factors for the development of almost all cardiovascular diseases across the lifespan, including coronary disease, left ventricular hypertrophy and valvular heart diseases, cardiac arrhythmias, cerebral stroke and renal failure 2. Additionally, HBP is the result of the interaction of environmental and genetic factors 3. There are two types of HBP: primary or essential, generally asymptomatic and not related to another medical condition (approximately 95% of cases), and secondary, attributed to some underlying pathophysiological mechanism, such as renal artery stenosis or aortic coarctation 4.
The development of primary HBP is associated with behavioral (unhealthy diets, tobacco use, sedentary lifestyle, harmful use of alcohol) and metabolic (diabetes, high cholesterol, overweight and obesity) risk factors 5. A positive association between obesity and blood pressure has been reported 6,7 particularly between abdominal obesity and high systolic blood pressure 8. Like-wise, social determinants of health such as income, education level and living conditions may have an adverse impact on behavioral risk factors and influence HBP development 5.
Traditionally, hypertension has been considered a disease that affects old people. However, the increase of cardiovascular damage at early ages has encouraged the study of childhood blood pressure (BP). In this regard, different reports have confirmed an increased prevalence of HBP 9,10 associated with excess weight 6,11 family socioeconomic status (SES) and maternal education 11,12 in children and adolescents.
According to the World Health Organization (WHO), the prevalence of overweight and obesity among children and adolescents aged 5-19 years has risen dramatically from 4% in 1975 to over 18% in 2016 13. Even more, in some countries of Latin America like Chile, Colombia, Venezuela and Argentina, recent studies have reported that overweight and obesity rates in school-age boys and girls appreciably exceed those rates 14-18.
The identification, examination and treatment of children at risk of HBP is necessary to reduce the high burden of cardiovascular disease, particularly considering the well-established global epidemic of childhood obesity and the increased HBP prevalence in the young 19. Despite this trend, evidence of childhood HBP in Argentina is scarce 20. For instance, high overweight and obesity prevalence rates have been reported in children and adolescents from the city of La Plata, located a few kilometers away from the country capital city of Argentina 18,21, but information about BP in this population is still missing.
The aim of this study was to determine the prevalence of high blood pressure in schoolchildren aged 4-14 years from urban peripheral areas of the city of La Plata, and analyze variations in high blood pressure prevalence by sex, age, excess weight and family socioeconomic status.
MATERIALS AND METHODS
Study area and sample
La Plata is located in the northeast of Buenos Aires province (34°56'00"S, 57°57'00"W). It is the fourth most populated city in Argentina (799,523 inhabitants). The study was conducted in public schools (kindergarten and elementary school) that were selected on a non-random basis from convenience sampling. First, we considered all the public schools that were authorized to participate in the study by the "Dirección General de Cultura y Educación de Buenos Aires". Then, 24 schools located in the periphery of the city were selected, looking to achieve the representation of that area, which is characterized by the presence of rural and urban lands. Families in rural areas are engaged in vegetable and fruit production for self-consumption and for sale in local markets, whereas urban areas are occupied by industries, distribution and service points, residential neighborhoods and recreative centers 22.
A cross-sectional study was performed. The data were collected between years 2015 and 2017 and the assessment was carried out on each student only once. The eligible population included all students from 4 to 13.9 years of age. Sample selection was largely determined by the presence of the children in the school and the voluntary participation in the study. The study goals and procedures were explained during meetings held at each participating school with parents and teachers. Children that had a chronic disease; or pathological conditions at the moment of the study; as well as those who did not have parental/guardian written informed consent; or who refused to participate were excluded. A total of 3,492 schoolchildren were assessed.
Blood pressure and anthropometric measurements
Systolic (SBP) and diastolic (DBP) BP were recorded using automatic blood pressure monitors with appropriate cuff size (OMRON HEM-7200) by research team members specially trained in these techniques. The instrument was calibrated at the beginning of each session using other similar precision instruments. All students were instructed to rest for 10 minutes in a conditioned environment prior to BP assessment, following the recommendations of The National High Blood Pressure Education Program Working Group on Children and Adolescent 23. Measurements were taken twice, separated by 5-min intervals between records. The average of both readings was calculated and used for subsequent analysis. High Blood Pressure was defined as SBP and/or DBP >95th percentile for sex, age and height according to the international guidelines of The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents 23.
The anthropometric study was carried out based on standardized protocols 24. Body weight (kg) was measured on a 100-g accurate digital scale (TANITA UM-061) with the subjects lightly clothed (the weight of the clothes being subtracted). Height (cm) was estimated using a portable vertical anthropometer (accuracy, 1 mm) (SECA 213). Body mass index (BMI) was calculated as weight (kg) divided by squared height (m2). Nutritional status was assessed with the WHO reference 25. Accordingly, schoolchildren were classified as well-nourished, stunted, wasted, overweight and obese.
Stunted and/or wasted schoolchildren (n= 180) were not included in the statistical analysis. Thus, the final sample included 3,312 schoolchildren (1,594 boys and 1,718 girls) (Table 1).
Socioeconomic analysis
Parents or guardians completed a structured questionnaire designed and validated by our research group to assess family SES by measuring housing quality with variables regarding structural features and amenities 14,18,26. he questionnaire included the following items: house building material (high-quality, fired-brick masonry; low-quality, prefabricated, makeshift housing); critical crowding (more than three persons per room); health (care in public hospitals; Job Insurance, medical insurance at the expense of the employer; Insurance plan, medical insurance paid by the person; financial assistance (national or local programs from government agencies, non-governmental organizations or other entities to benefit poor families by providing cash relief to the heads of households); parental education (elementary, high school, university); parental job (formal worker: performing mostly temporary jobs; informal worker: performing occasional jobs; unemployed); access to consumer goods (car, computer, internet, cable television, air conditioning).
Statistical analysis
Mean and standard deviations of SBP and DBP were calculated. Sex and age factors were evaluated with analysis of variance (ANOVA) and Tukey post-hoc test. The prevalence of HBP was compared with sex, age and nutritional status using chi square test. Socioeconomic data were analyzed using principal component analysis (PCA) and the generalized linear model (logit link) against the variable HBP. In all cases, significance was set at p< 0,05.
Ethics statement
Research protocols followed the principles proclaimed in the Universal Declaration of Human Rights, the ethical standards instituted by the Nuremberg Code 27, the Helsinki Declaration 28 and successive modifications, as well as those of the Argentine Personal Data Protection Act N° 25326 29. This study was approved by the National University of La Plata (UNLP) and by the Bioethics Committee of the Latin American School of Bioethics (CELABE, for its acronym in Spanish; Resolution 0220/16, Record 76).
RESULTS
Results from the ANOVA showed that mean SBP and DBP values increased significantly with age (p<0.001) (Figure 1). On the other hand, differences by sex were not significant. Analysis with the Tukey test indicated significant SBP and DBP differences (negative values) in age groups 7-8 and 11-12 years. Thus, schoolchildren were further divided into Group 1 (G1, 4-7 years old), Group 2 (G2, 8-11 years old) and Group 3 (G3, 12-14 years old).
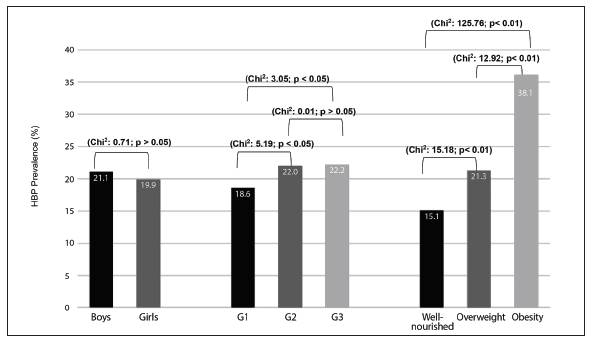
The prevalence of HBP in schoolchildren was 20.5%, distributed as follows: high SBP, 10.8%; high DBP, 4.1%; high SBP and DBP, 5.6%. Nutritional status was adequate in 57.1% of children, whereas 24.6% were overweight and 18.3% were obese. Despite HBP rates did not differ by sex, differences were significant when associated with age (G1 < G2 and G3) and nutritional status (well-nourished < overweight < obese) (Figure 2).
Source: own elaboration.
Figure 2 Prevalence of high blood pressure (HBP) by sex, age and nutritional status. Chi square (Chi2) comparison. Group 1 (G1, 4-7 years old schoolchildren), Group 2 (G2, 8-11 years old schoolchildren) and Group 3 (G3, 12-14 years old schoolchildren)
Table 2 presents the comparative analysis of HBP+overweight and HBP+obesity prevalence by sex and age. Higher HBP+obesity rates were observed in boys as compared with girls. The percentage of HBP+overweight schoolchildren was significantly higher from 12 years of age onwards and those of HBP+obese was significantly higher from 8 to 11 years of age.
Table 2 Prevalence (%) of high blood pressure (HBP)+overweight, and HBP+obesity in schoolchildren
Chi-square (Chi2) comparison between sexes and among age groups Group 1 (G1, 4-7 years old schoolchildren), Group 2 (G2, 8-11 years old schoolchildren) and Group 3 (G3, 12-14 years old schoolchildren).
Source: own elaboration.
Results of the PCA determined that component 1 explained 18.76% of variance (0.75 Cronbach alpha), showing that the original variables were properly represented for this component, whereas component 2 explained 8.35% of the variance (0.35 Cronbach alpha). The first component discriminated positive and negative values associated with the most and least favorable family SES, respectively (Figure 3). Positive values associated with higher parental education level, possession of material goods, fired-brick masonry housing, formal parental job and paid health insurance. On the other hand, negative values associated with financial assistance, poor housing conditions, father unemployment, overcrowding and free public healthcare.

Source: own elaboration.
Figura 3 Eigenvectors corresponding to socioeconomic characteristics. Dimension 1 positive values: 1-Health: Job Insurance. 2-Father's job (formal employment). 3-Mother's job (formal employment). 4-Health: Insurance plan. 5-Cable television. 6-Father's education. 7-Car. 8-Mother's education. 9-Internet. 10-Air conditioning. 11-Mother's work (unemployed). 12- High-quality house. Dimension 1 negative values: 13-Health: Care in Public hospital. 14-Father's job (unemployed). 15-Financial assistance. 16-Critical crowding. 17- Low-quality house.
Finally, the generalized linear model for HBP as a function of component 1 showed a higher probability of finding childhood HBP associated with adequate family SES (Beta, 0.085; Wald coefficient, 4.105; p=0.043).
DISCUSSION
Most population studies about HBP in children and adolescents from Argentina are based on information collected in urban areas 30-33. On the contrary, studies evaluating this issue are scarce in rural populations 34 and non-existent in periurban areas. The present study provides novel data about the prevalence of HBP in children and adolescents from the periphery of the city of La Plata and its variation by sex, age and nutritional status.
It is known that BP levels change during childhood and adolescence. Between 6 years of age and puberty onset and under non-pathological conditions, SBP and DBP increase by 1.2 and 0.5-1 mmHg, respectively, showing slight differences between boys and girls. Later, the increase of both SBP and DBP is more marked, particularly in boys due to their greater body mass 35. In agreement with the above mentioned, SBP and DBP values in our sample of schoolchildren showed a progressive increment with age, which was more noticeable in age groups 7-8 and 11-12 years. On the contrary, mean SBP and DBP values were similar between boys and girls, probably because our study included schoolchildren up to the age of 14 years, and differences are more pronounced above that age.
The fact that BP is strongly determined by height and therefore varies during growth and development 23 does not allow the use of fixed BP values to detect hypertensive children and adolescents, as it occurs in adults, who have stopped growing. Thus, in 1996, height was incorporated into the normative data and it is now recognized that BP levels should be interpreted on the basis of sex, age and height to avoid misclassification of children who are either extremely tall or extremely short 36. In our study, HBP rates were high, since 20.5% of schoolchildren had SBP and/ or DBP values > 95th percentile, as reported in The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents 23. This prevalence was above the HBP value informed in Argentina by Gotthelf and Fonseca 31; Pedrozo et al. 32, and Szer et al. 37 in schoolchildren from the provinces of Misiones (8%), Salta (12%) and Buenos Aires (10%), and similar to that reported by Poletti and Barrios 33 and González Calbano et al. 30 in schoolchildren from Corrientes (19%) and Córdoba (24%). Although there are some methodological differences between our study and those aforementioned, we consider that the comparison of results provide useful evidence to estimate the extent of the problem.
In addition to the high prevalence of HBP, 43% of schoolchildren were overweight/obese. Excess weight has increased notably in recent years in children and adolescents, as evidenced by national and international reports 16,18,38,39. In line with those studies, our research group reported a 20% increase in overweight/obesity prevalence in children and adolescents from La Plata in the past ten years 21. The association between overweight/obesity and HBP in children and adolescents has been reported in numerous studies and different populations 6,11,40. All studies reported higher HBP prevalence in overweight/obese children compared with lean individuals. Likewise, obese and overweight schoolchildren from La Plata were more likely to present HBP than well-nourished peers. In this regard, to explain why obesity was associated with hypertension, Brady 6 focused on the role of the dysfunctional adipocyte and the increment of sympathetic nervous system activity, which leads to elevated BP by increasing renin-angiotensin-aldosterone system activity.
In accordance with other studies, our results further showed that both childhood HBP+overweigh and HBP+obesity prevalence was higher from 8 years of age onwards 41,42. Children and adolescents are a particular interest groups for public health. It is known that many characteristics of adult life are acquired or consolidated in those age groups, making it important to evaluate determinant factors such as dietary habits and/or the physical exercise practices. In this context, are particularly important the food stalls at the schools called "kioskos" that offer snacks, sweets and soft drinks, among other highly caloric, low-nutrition and addictive foods which could partly explain the continuous increase in adiposity in children and adolescents. However, we did not analyze the food habits of this schoolchildren population and we consider that these aspects should be investigated in future research.
On the other hand, despite HBP prevalence was similar in both sexes, it was higher in boys than girls when associated with obesity. In this sense, de Moraes et al. 43 reported that sex differences in HBP could be related to sex differences in body fat distribution. These authors also suggested that android fat distribution (more frequent in boys) would induce increased sympathetic activity, which would in turn increase sodium absorption, thus leading to increased peripheral vascular resistance and, consequently, higher BP. However, knowledge of the incidence of sex on HBP associated with excess weight is still scarce 44,45.
In general, populations of lower SES are likely to present chronic diseases and higher disease burden at earlier ages 46. In the case of HBP, results are controversial. Some authors suggest that low SES increases the chances of having HBP 12 while others have reported opposite results. For instance, Bloch et al. 41 found that HBP rates in 73,399 schoolchildren from Brazil were lower in those living in the northeast (a region with high poverty rates) as compared with those living in southern districts. In our study, favorable family SES was not a protective factor. Rather, HBP prevalence was higher in schoolchildren with higher family SES, whose parents had formal employment, high educational level, lived in good housing conditions and had access to private health insurance. However, further studies are needed to determine whether this association was due to any particular socioeconomic factor.
The association of high HBP rates with overweight and obesity detected in our study of schoolchildren from La Plata reveal a complex health scenario and give an account of the need to implement immediate actions for improving the current and future healthcare of the study population. Since the benefits of weight loss in reducing BP in children have been demonstrated 6 interventions should address the main components of energy balance, focusing on improvement of eating habits and physical activity through education and counseling.
Finally, despite some limitation of this study, such as the cross-sectional design which did not allow to establish causality and the fact that BP measurements were obtained at one single visit overstretching HBP prevalence 47, we consider that the size of the sample and the representative nature of the data led to the reliability of the outcomes. Also, the findings provide new age-stratified evidence on an important health problem in pediatric population.
CONCLUSIONS
Schoolchildren living in urban peripheral areas of the city of La Plata, Argentina, presented higher HBP prevalence. While HBP prevalence was higher among overweight/obese children, those aged >8 years and those of more favorable family SES, sex did not affect HBP development. However, when HBP was analyzed associated with nutritional status, obese boys were more likely to have HBP than girls.

















