INTRODUCTION
Asthma is an inflammatory respiratory illness affecting between 5-16% of the population around the world; 1 it has also been on the rise since the second half of the 20th century, especially in industrialized countries. 2 The mechanism behind the illness and the reasons for its rise have not been completely specified. However, some risk factors have been identified, such as genetics, 3 taking certain medicines, 4 environmental factors, 5 and other lifestyle-related factors, such as nutrition. 6
In the traditions of several cultures and traditional health systems, the concepts of cold and heat are considered one of the most important factors for health, and they emphasize the importance of cold exposure as a cause or a risk factor of inflammatory respiratory processes, especially asthma. In the Afro-Colombian Pacific tradition, water and air exposure are causes of disease, due to their link to cold and humidity. 7) In the Bolivian plateau, Aymara medicine considers that illnesses caused by cold are counteracted by hot remedies and conversely. 8 Some authors in Colombia report medicinal plants that fall in the cold and hot categories in indigenous, 9 rural mestizo9 and even urban communities. 10
In Chinese traditional medicine, cold is a pathogenic factor, and a cold syndrome is considered to include all illnesses caused by cold pathogenic energy, or by a decrease in yang and an excess of yin. 11) In ancient Ayurveda traditional medicine, the concept of virya refers to the effect of heat and cold transmitted by substances that are ingested; the hot and cold properties give these substances a therapeutic quality.12 One of the transgressions in the cosmic rhythm that leads to disease is osha vata, which is cold and dry. 12
The concept of cold has endured in popular concepts and beliefs. In English, the word cold simultaneously refers to lower temperatures and to an illness, which points to the same meaning the word resfrío used to have in Spanish before the term gripe (flu) was introduced. In popular imagination, there is still a belief that cold causes or worsens respiratory illnesses.
Traditional care is a peripheral aspect and almost nonexistent in the management guidelines of respiratory diseases, 13-15 although the cultural dimension has significant impact on monitoring and treatment of asthma. 16
Several studies highlight the persistence and importance of classical concepts of cold and heat in traditional medicine and their role in explaining the occurrence of asthma, even in highly urbanized countries such as the United States. 17 For example, a study reports that 76% of Hispanic mothers in New York recognize the importance of keeping their children sheltered to prevent asthma attacks. Similarly, they attributed asthma attacks in school to exposure to cold air. 16 Other studies report that these concepts persist, and urban communities share the same concepts in countries such as Puerto Rico, Mexico, Guatemala, Singapore, Malaysia and China. 18,19
We have not found systematic review or meta-analysis studies, which explored the association between cold exposure and asthma. This study sought to conduct a systematic review and a me-ta-analysis of observational and experimental studies that explore the relation between asthma and cold exposure.
METHODS
Inclusion criteria
Systematic review with meta-analysis of observational and experimental studies among humans of all ages, published or non-published, based on the Cochrane Collaboration 20 and Centre for Reviews Dissemination guidelines. 21 We excluded studies that did not assess the association among individuals (ecological studies). For the meta-analysis, we included only the studies that reported sample size, characteristics of the exposition and the outcome, and frequency of asthma among exposed and non-exposed.
The protocol of this systematic review is available in the repository of the Universidad del Rosario's research fund under the registration number QDN_B0002 and is accessible from the Research Director of the Universidad del Rosario under reasonable request (direccion.investigacion@urosario.edu.co).
The outcome variable was asthma. We defined asthma occurrence as a clinical asthma diagnosis by a doctor 22, the mechanical spirometry test and positive reversibility with a bronchodilator, 22 bronchial stimulus testing with methacholine 23 or prostaglandins, 24 exercise-induced bronchoconstriction, 25 or prostaglandins, 24 exercise-induced bronchoconstriction, 25 IgE antibody levels for allergy patients, 26 questionnaires, genetics tests or a combination of two or more methods. We included any of the following possibilities: prevalence of asthma, asthma incidence (new cases and crisis or exacerbation), severity, emergency room visits due to asthma attacks, and hospitalization for asthma.
The exposure variable was cold. The operational definition for this term is not precise, especially if we consider that it is a physical-chemical characteristic that is not often considered in physiology, biochemistry and physiopathology. The search strategy included the following variables: environmental air (outdoor/indoor), inhaled air (controlled exposure), food and drink, lower body temperature (skin), and two or more of the above. We consider cold when studies explicitly contrast any of these variables with a group exposed to higher temperature and the other exposed to low temperature.
Search methods to identify studies
We carried out an electronic search of publications in English, Spanish and Portuguese without time restrictions, up to 11 August 2015, in the following databases: PubMed, Embase, Lilacs and the Cochrane Central Register of Controlled Trials. The search used standard descriptors (MeSH, Emtree and DeCS) and free text words. Additionally, we performed a manual search for potentially relevant articles among the bibliographic references of the selected articles.
Two independent researchers (IS and JP) reviewed the titles and abstracts of all the articles identified in the first stage of the search, to identify potentially relevant sources. Once the articles were identified, both researchers applied the inclusion criteria (Additional file 1) and data-extraction criteria separately (Additional file 2). Possible differences were solved by consensus. These two criteria were piloted in a random sample with 10% of the studies, which allowed the instrument to be fine-tuned.
Data collection and analysis
We performed a first analysis to identify general characteristics of the studies, including year of publication, country in which it was carried out, study type, asthma diagnosis method, asthma occurrence measurement, exposure measurement and covariates.
Quantitative information was analyzed using RevMan 5.3's meta-analysis module. 27 The statistical analysis was based on the random effects model, considering the diversity of criteria for exposure and reported categories of asthma among included studies.
For the general occurrence relation (any type of cold exposure and any asthma category), we obtained the summary weighted Odds Ratio (ORw) and its 95% confidence intervals (95%CI), including data collected from all the references which met the inclusion criteria, independently whether they were observational or experimental studies. We also performed a subgroup analysis by type of cold exposure, reported categories of asthma, and study design.
We performed the risk of bias assessment using the categories proposed by the Cochrane collaboration: sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting and other elements. 20 We used the RevMan 5.3's risk of bias form. 27 The risk of bias was assessed using a funnel plot, keeping in mind the small number of studies and the use of OR as a measure of association, which makes the results less reliable; we did not apply statistical tests for funnel plot asymmetry. 20
We carried out a sensitivity analysis to identify the influence of each study, replicating the meta-analysis and eliminating one of the included studies at each step. 28 The heterogeneity analysis for the studies used the 12 statistical test from the RevMan 5.3 software, which expresses the level of inconsistency, obtained through the formula that combines Q (statistical chi-squared) with the number of degrees of freedom. When 12 had a value above 50%, it is considered that there is substantial heterogeneity. 28
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, 29 both the flowchart and checklist, were followed during the preparation of this review (Additional file 4).
RESULTS
The search strategy yielded 2164 potential studies. The bibliographical references yielded other 43 studies. After removing duplicated records, we obtained a total of 2146 studies. After reviewing the titles and abstracts, we obtained 295 studies. Some 59.4% (116/295) had information related to the contrast between asthma occurrence and cold exposure, although they were excluded due to their ecologic designs. Applying the inclusion criteria yielded 86 studies (Additional file 3). Finally, the data-extraction criteria yielded 10 studies for meta-analysis, as seen in Figure 1.
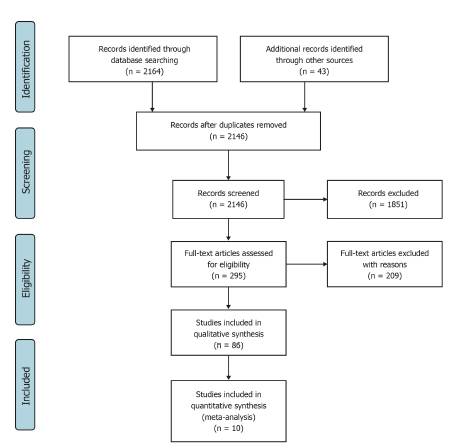
Fuente: Adapted from the freely available form at http://prisma-statement.org
Figure 1 Flowchart of the study selection process
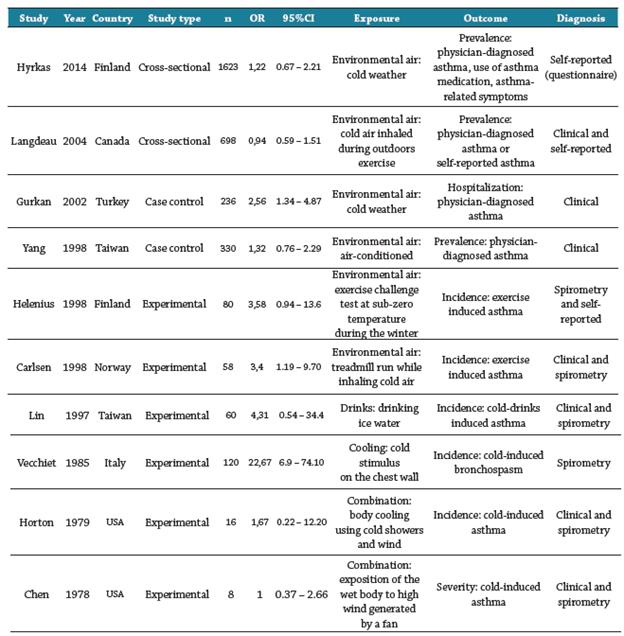
Characteristics of included studies for data extraction
Applying the data extraction criteria to 86 studies and 11 references (12.8%) yielded data about associations, although without providing details regarding the sample size or the frequency of exposed and non-exposed. We communicated with the authors via e-mail and received responses from two of them, who stated they did not have the data available; there was no reply from the rest. Of the 86 studies, 11.6% (10/86) met all the inclusion criteria for meta-analysis (Table 1 shows the characteristics of the 10 included studies). 30-39
Intervention effects
The summary measurement with the random effects model (Figure 2) shows that a subject exposed to cold is more likely to have asthma (ORw 2.0 95%CI 1.28-3.14). A quality assessment showed that the level of evidence has a high risk of bias (Figures 3 and 4).
Fuente: Created by the authors.
Figure 2 Forest plot of the association between cold and asthma: random effects model
Fuente: Created by the authors.
Figure 4 Risk of bias for studies included in meta-analysis - Summary
As seen in the funnel plot (Figure 5), the ten included studies have evident publication bias. Considering the low number of studies and the use of OR as a measure of effect, we did not carry out a statistical test.
The Revman 5.3 software yielded the 12 statistical heterogeneity: 63.1% (27%-81.4%). We carried out a sensitivity analysis, successively removing one study at a time. At no point did the summary measurement lose statistical significance (Table 2). The Hyrkas 30 study produced the highest increment of the summary measurement when removed, while the one by Vecchiet caused the highest reduction. 31
Subgroup meta-analysis
Regarding the study design, 6 of the 10 were experimental. Random effects model showed that a person exposed to cold is 3.8 times more likely to have asthma, compared to a person not exposed (ORp 3.8 95%CI 1.7-8.86) as shown in Figure 6.
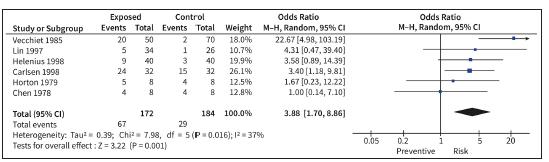
Fuente: Created by the authors.
Figure 6 Forest plot of the association between cold and asthma of experimental studies: random effects model
With regards to the exposure categories, 6 of the 10 studies contrasted environmental air (outdoor/indoor) and the random effects model showed that the asthma risk for a person exposed to cold environmental air was 1.6 times higher compared with a non-exposed person (ORw 1.59 95%CI 1.1-2.3). In relation to the outcome, 5 of the 10 studies contrasted cold with asthma incidence (new cases and crisis or exacerbation) and the random effects model showed that a person exposed to cold had 4.7 times the risk of asthma incidence, compared to a non-exposed person (ORw 4.73 95%CI 2.06-10.85). Also, 3 of the 10 studies contrasted cold with asthma prevalence and the random effects model showed that the association between cold and asthma prevalence could be explained by chance (ORw 1.12 95%CI 0.82-1.52).
DISCUSSION
The meta-analysis showed an association between cold exposure and asthma for experimental studies (ORw 3.8 95%CI 1.7-8.86) and for all the studies (ORw 2.0 95%CI 1.28-3.14). The sensitivity analysis showed that none of the 10 studies changed the statistical significance. The subgroup analysis showed that cold environment exposure is a risk factor for asthma (ORw 1.59 95%CI 1.12.3) and that cold exposure is a risk factor for asthma incidence (ORw 4.73 95%CI 2.06-10.85).
Cold exposure has been described by some clinical management guides as a precipitating or aggravating factor of asthma, without specifying the mechanism behind it 13,40. The 2014 Gina guide includes the word cold, defined as the common cold, for symptoms associated to respiratory infections and as an aggravating factor for coughs. It also defines cold air as a triggering factor and recommends that athletes avoid exercise in very cold climates.(22 Another study also concluded that cold air induces ventilation disturbances in asthma patients. 41
Despite probable evidence, asthma diagnosis, prevention and treatment guides do not suggest controlling cold exposure. We only found one study that recommends considering the role of climate in management plans: "It is important to understand how local weather patterns influence asthma attendance in general practice so that asthma management plans might include specific advice to adjust medication according to the local weather." 42
A working group composed of pediatricians and general practitioners in the Asia-Pacific region, stressed the importance of expanding the evidence on the practices of traditional medicine for the treatment of asthma in pediatric population, as part of one of the six challenges for primary care asthma in this region. 43
Quality of evidence and study limitations
Quality assessment in the 10 studies included in the meta-analysis showed a high risk of bias. We found no randomized trials or cohort studies. Six of the studies were experimental, all made in the past century, with little rigor in control and randomization.
We found a high level of heterogeneity among studies (12 test: 63.1%). The operational definition of asthma is not precise, and the means of diagnosing and including cases varied greatly between studies. Also, the operational definition of exposure also varied; it included diverse categories, such as body cooling by water or drinks and cooling by exposure to environmental air. The funnel chart showed an evident publication bias in all ten included studies.
We could not detect a specific association between asthma and exposure to cold food or drinks, lowering body temperatures, or cold-water showers. We were also unable to detect an association between cold exposure and other asthma related outcomes, such as prevalence, mortality, absence from school, seeking emergency healthcare services and hospitalization. The reason for this limitation was the absence of at least two studies that explored these associations.
Most studies were performed in first-world countries or in temperate countries, which makes it difficult to assess likely associations with geographic, economic and climatic conditions in equatorial countries. All the studies showed a weak covariance analysis to determine possible effect modifiers and confounders. There are few studies exploring the relation between asthma and altitude and other geo-climatic effects. 44 Most studies related to cold exposure and respiratory illnesses have been carried out in temperate countries, with a predominating measure of the seasonal variable, without taking into account, for example, that during the hotter months of late spring and summer respiratory illnesses can be associated to the presence of pollen 45 or to the use and abuse of air-conditioning, while during the colder months of late-autumn and winter the association is confounded by heating, 46 winter sports, 47 or higher concentrations of microbial agents in closed quarters. 5 Cold exposure can also be confounded by air contamination due to fine particles such as sulfur dioxide, 48,49 or by the presence of dust mites and mold. 50 Finally, research on cold exposure and respiratory illnesses has been predominantly done through ecological studies, which do not assess individual subject associations.
CONCLUSIONS
The systematic review and meta-analysis of the few available studies, which showed a high risk of bias and a high level of statistical heterogeneity, showed that cold exposure -particularly cold environments- is a risk factor for asthma. Although better evidence is needed, this study encourages to explore the concepts proposed by the traditional medicine to establish its benefits on the prevention and care of respiratory diseases, such as asthma.