INTRODUCTION.
Today's health care organizations are inserted in a complex environment that forces them to offer a wide range of products and services provided by multiple health professionals whose focus should be on quality and permanent result evaluation processes 1-3.
Being this how it is perceived, patient safety and quality improvement efforts focus on a complex environment with finite resources and results in increased public scrutiny over their use. Therefore, health care requires a better understanding of the implications in health economics from professionals; understanding it as a field of research whose object of study is the partial or complete analysis of cost-effectiveness elements involved in the use of human and material resources, and the organization of health services as structural elements of efficiency of health systems in their function of treating illness, working on health promotion, and prevention 4-7.
Health economics, in the words of Collazo et al., "integrates economic, social, clinical, and epidemiological theories in order to study the mechanisms and factors that determine, affect, and condition the production, distribution, consumption, and financing of health services, and it is applied for the development of policy instruments; health and its economic value; demand and supply of medical care; the equilibrium of the market; planning, regulation, and monitoring of sanitary actions; the comprehensive evaluation of the health system; economic evaluation of specific health technologies; and microeconomic evaluation" 8.
It is then, when, in the dynamics generated in health economy, the health team in general, and the nursing professional in particular, determine their relevance and become an indispensable political actor for health management, in terms of decision-making as to searching for efficient and rational strategies.
From this perspective, and in times of great socio-sanitary conjunctures, such as these, to identify the influence that the nursing discipline has on the dynamics generated in the health economy and the provision of health services is vital, showing the human capital that it has to prioritize the optimization of resources, the costs and benefits of the care management in the health organization; by virtue of improvements in the quality of people's health and continuity of care 9-15. On it, the role that the nursing professional has played in the current socio-sanitary crisis is highlighted, becoming a front-line player in health.
The purpose of this study is to know the influence of nursing on health economy, considered as a field of study that allows for the analysis of a wide range of decision-making strategies that guide efficient and rational possibilities for health management. This research project will use systematized literature review of recent years, in order to highlight or demonstrate the various observable and non-observable aspects that the Nursing profession entails, which could contribute to health management. In order to determine the implications of nursing on health economics, as seen in the literature.
MATERIALS AND METHODS.
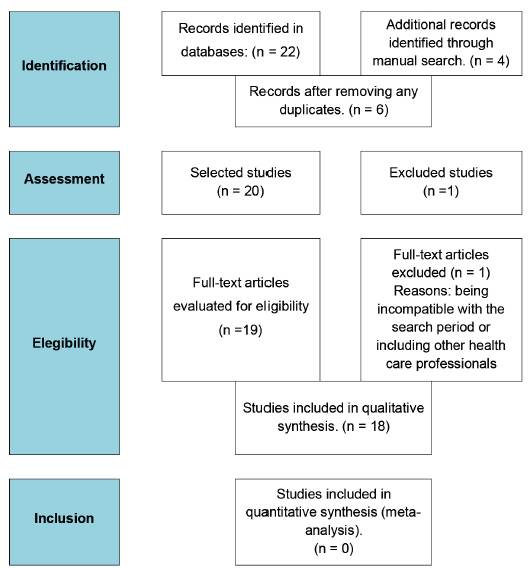
Type of study: integrative review of the qualitative type of literature 15,16,17, following a descriptive structure in the report, making use of the recommendations of the SALSA review method (Search, Assessment, Synthesis and Analysis) 15, and adjusting the PRISMA tool 18,19 to the purpose of the investigative process. The integrative review was guided by the questions: What is the role of nursing in the health economy? And how can we strengthen nursing work in the face of socio-sanitary scenarios of uncertainty?
Selection criteria
Inclusion criteria: quantitative and qualitative research, opinion articles, essays and reflections, structured searches of the literature, study population nurses; developed in any country; whose results report the relationship between political economy and nursing; in English, Spanish, and Portuguese languages.
Exclusion criteria: Research carried out outside the established period of time, study population that includes other health professionals.
Data collection: A search of the information was carried out between June 26, 2019 and November 26, 2019. The following key terms were used as a search strategy for this review: "nurses and health economics" and "health economics. nursing" in the OVID, Pubmed, Clinikal key, and Scielo databases. The following filters were used: years of publication (2000-2018), research area (nursing), type of document (article), language (English, Spanish or Portuguese), text availability (abstract and full text), species (humans), and the Boolean operator AND, to relate Health economics AND nursing; Nursing AND health economics AND nursing and their related key terms and the concatenator, in quotation marks to search for the exact term: "health economics"
Study population: Data were extracted from 18 selected studies after application of eligibility criteria, elimination of duplicates, and assessment of methodological quality. It is important to note that since different types of studies were included, it was considered as the only criterion that they fulfilled all the elements required according to the standards for each type of study. The details of the articles retrieved were 5 from OVID, 10 from Pubmed, none from Clinikal key, and 3 from Scielo. The different stages of the review are detailed in Figure 1.
Data analysis and statistical data treatment
The authors independently reviewed the abstracts of each selected study, applying the eligibility criteria and assessment of methodological quality. It is important to note that it was the only quality considered criterion was they met all the items required according to the standards for each type of study, considering that they were extracted from indexed journals having an editorial committee. Furthermore, there were no episodes of eligibility differences.
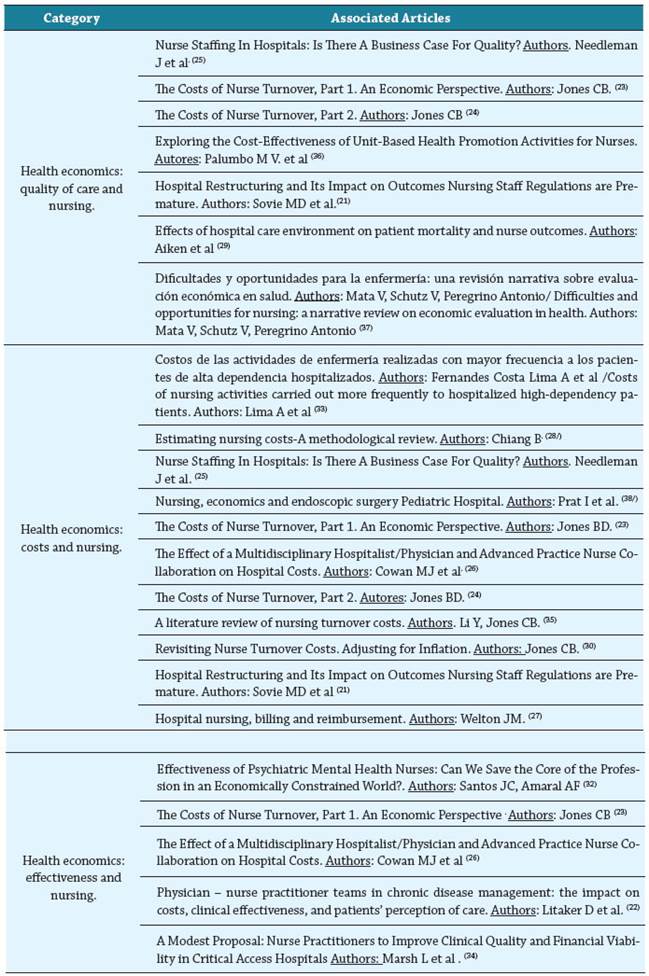
The data from the different studies was summarized using a narrative-qualitative synthesis. With the emerged data, a summary table was generated in order to characterize the studies, considering the following elements: article title / author (s); country / year, study design, and main findings which detail the implication of nursing in the health economy, a table that summarizes the qualitative-descriptive synthesis of the articles and finally a third table, with the description of articles by categories emerged from the review: a) health economics: quality of care and nursing; b) health economics: costs and nursing and c) health economics: effectiveness and nursing.
Ethical aspects. Given the study methodology, this article does not require approval from the ethics committee.
RESULTS
Out of a total of 26 articles, 18 studies were included in the qualitative analysis work. Information was systematized in Table 1, characterization of the studies; Table 2, qualitative - descriptive synthesis of the articles and Table 1, description of articles by categories. The descriptive analysis highlights 44% of the publications were made in the period between 2005 and 2009; 78% were carried out in the United States; 56% were obtained from PUBMED, and 44% are of quantitative research design. (See Table 2.). The categorical analysis of the results shows a clear trend in the literature to reveal the economic cost related to the impact of the nursing professionals' work in various areas, rather than considerations of quality of care or effectiveness of work. (See Table 3).
Table 1 Studies Characterization
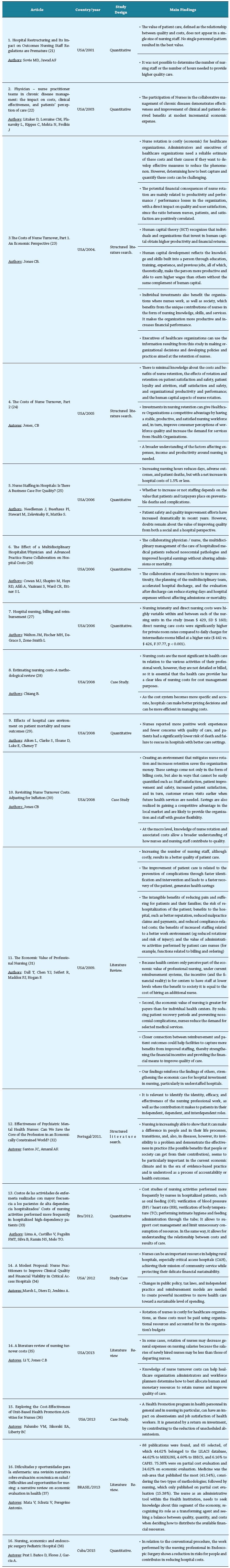
Source: own elaboration resource from the descriptive qualitative analysis of the included texts.
Table 2 Qualitative-descriptive synthesis of the articles
Source: own elaboration resource from the descriptive analysis of the included texts.
DISCUSSION
This study allowed us to know the implications of nursing on health economics as seen in the literature, considered as a field of study with broad edges that allows for the analysis of various decision-making strategies that guide towards efficient and rational possibilities for health management.
In this sense, the various observable and unobservable aspects that the Nursing profession has in these matters, should be of permanent analysis and consideration by decision-makers, due to its high representation in the total workforce in the world and the diversification of activities associated with people's health care 39,40,41, as ways of responding to access, quality of health care, and universal health coverage 42; in times when these variables become fundamental in the face of the diverse health needs of people 43,44.
Health economics: quality of care and nursing
In this regard, the evidence included in this research process suggests a relationship between healthcare quality and prominent components such as the development of human capital, which is considered a strategy that theoretically makes people more productive than others without the same development complement 23,25. In this sense, the studies suggest that individual investments benefit the organizations where the nursing professional works, as well as society in general, which in turn benefit from the unique contributions that these professionals make in the form of knowledge, skills, decision making, safety, and care of people 23,25,28. Likewise, this knowledge makes organizations more productive, increasing the financial performance of the organization, with a direct impact on quality and user satisfaction 23.
For this reason, hospital investment in nursing in terms of expenses, as well as income and productivity, need a broader knowledge 24, which incorporates, in the analysis of factors associated with the health economy, items such as: adequate care settings 29; health promotion in staff 36; increased staffing and professional working hours, incorporating new professional hiring 24; implications of the rotation and retention of nurses 23,24. However, the value of patient care, defined as the relationship between quality and costs 21, is one of the elements that is mainly or on some occasions only used to define these aspects.
Although it is true that human capital development, increased hours, professional rotation, and staff retention are costly factors for health organizations, translated into net increases in hospital costs 23,24,25. In any case, it is necessary to recognize the transforming role of nursing and seek a balance between quality, quantity, and costs when deciding how to distribute the available financial resources 37 to achieve a direct impact on quality and user satisfaction 23,29.
Health economics: costs and nursing
In relation to this topic, the different studies show the challenges posed by the significant nursing costs for health care 27,28,33. Which constitute at least a quarter of the operating budget of a hospital establishment and make up the individual workforce cost for hospitals 27,29. This means that the provider makes greater efforts to analyze them in detail, as Chiang 28 points out, in order to achieve "better pricing decisions", and being more efficient in cost management.
In this sense, the review showed that the net increase in hospital costs is related to an increase in nursing professional hours, an increase in staffing, 21,25 rotation and retention of the nursing professional in health organizations 23,24, in addition to investment in specialties for the care of people 23,38. All these factors should become a managerial priority given the impact on the value of quality and satisfaction in health, both from the social and hospital perspective 23, considering that investing in quality by incorporating these elements directly impacts costs 26, becoming a competitive advantage by having a stable, productive, and satisfied nursing workforce 24.
On the other hand, other elements that contribute to strengthening the financial management of clinical processes and that work in a recursive way are revealed: cost studies 33, safety and quality considerations 23,25,26, reduction of rotation 23,32,35, multidisciplinary management of patient care, collaboration between the doctor-nurse binomial, improvements to continuity, care planning 26, and work to minimize the hospital stay of patients 35
Health Economy: effectiveness and nursing
Finally, the literature shows that the nursing professional constitutes one of the main "cost management tools", since it is present in various clinical services and always close to its users, which facilitates the evaluation of their interventions and care 45. Considering that effectiveness has been conceptually defined as "the added value or impact that a product or service gives to a customer or user and that allows them to improve their quality of life or satisfy a need"45, added to the fact that it has a great relationship with the quality perceived by users. From these perspectives, the texts included in this category reveal a fundamental contribution of nursing to the health economy.
Therefore, it is important to ascertain the identity, efficacy, and effectiveness of the nursing professional work, identifying the contribution it makes to patients and clinical processes 32,46,47.
In addition to this, and in the broad sense of the conceptual definition of effectiveness that emphasizes the great importance of achieving goals or objectives 48, and the great relationship between effectiveness and the approach to quality 49, the review highlights collaborative work 22,26, investment in strategies for loyalty of nursing professionals 26,33, and recognition of the professional role 32, as structural elements to strengthen the effectiveness of health management.
That is why the nursing professional should be a concern for organizations, taking into account that meeting the needs of users, family members, and other interested parties is the "maximum expression of success" 49) in organizations, health being this case. Considering also, the evidence that relates the nursing professional, with the results for the patient 50, and the permanent importance given by the nursing professional to the quality of care in their commitment to patient safety and continuous improvement 51.
CONCLUSION
The present research process made it possible to describe the implications - as seen in the literature - of nursing on health economics. In this sense, different links were observed between nursing activities and health economics, in three main aspects: quality of care, costs, and effectiveness. In each of them, there is a wide range of related factors, which emphasize the recognition of the professional role of nursing, as a means to strengthen the effectiveness of health management and, in the same way, the quality of health care.
Although, it is true that the research process allowed for finding elements aiming at understanding the relationship between the nursing professional in matters of health management and health economics; it is necessary to deepen this, through new investigative strategies that demonstrate their real and significant impact on the efficient and effective management of resources.