INTRODUCTION
For over 35 years, Salud Uninorte has been a pioneer in expanding topics covered by a scientific publication. Authors and readers have consistently benefited from this dedication to covering a wide variety of topics related to the basic sciences, medicine, and public health. Through this editorial, the authors seek to challenge readers to, once again, expand their research topics and explore the under-acknowledged topic of unintentional injuries. Unintentional injuries contribute disproportionally to high morbidity and mortality rates around the world. Despite their impact on the productivity and health of populations around the world, not enough is being done to mitigate their impact. The purpose of this editorial is to explore strategies designed to mitigate unintentional injuries' impact on the well-being of individuals and societies. A literature review was conducted to determine the current impact of unintentional injuries in low- and middle-income countries.
More people are estimated to die from unintentional injuries yearly than from tuberculosis, malaria, and the human immunodeficiency virus (HIV) combined1. Furthermore, it is estimated that for every injury-related fatality, there are up to 50 non-fatal injuries, which have a detrimental impact on all aspects of society, including quality of life, productivity, and disability-adjusted life years (DALYs).
There are significant differences by region, regarding injuries. The data shows that over 75% of injuries occur in low- and middle-income countries 2-4. In Latin America, injuries resulting from traffic collisions, poisoning, falls, and burns, among others, accounted for almost 10% of all deaths in the region in 20155. The incidence of injuries varies from country to country, and it is also affected by gender, age, and income, among other demographic factors. According to a 2020 report by the World Bank, gender differences were highest in Venezuela, El Salvador, and Colombia, while Cuba and Bolivia had the least gender differences.
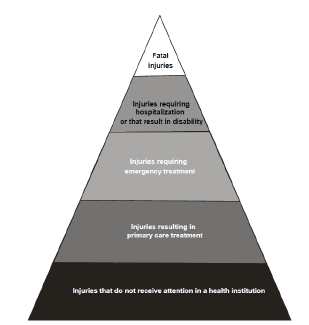
Given the impact of injuries on the health status of diverse populations, it is not surprising that addressing injuries is a high priority for public health and medical professionals worldwide. The injury pyramid illustrates the burden of injuries on health care systems, and it provides a visual representation of the scale and severity of injuries for any given region. It should be noted that the shape of the injury pyramid is determined by factors including the cause of injury, quality of data, and access to health care services (see Figure 1).
Defining injuries is not easy, despite their impact on morbidity and mortality rates. Unlike other medical conditions, the definition of injury/injuries must include the causative event or etiological agent and the resulting pathology. For this editorial, we will adopt the definition provided by Norton, Hyder, Bishai, and Peden 6, who describe injuries as the damage resulting from the "acute transfer of energy", or by the immediate absence of heat or oxygen. Injuries differ from diseases as injuries are more acute, and the appearance interval is much faster than chronic or infectious diseases. In addition, while the words "injury" and "accident" are generally considered synonyms, experts suggest that they are not the same, and the word "accident" should be avoided.
INTENTIONAL INJURIES
According to the WHO7, injuries are classified based upon "intentionality." Intentional injuries generally result from purposeful action directed at oneself or others, and they include acts of interpersonal violence (sexual assault, homicide, neglect), suicide, and collective violence, as in times of war. For our discussion, we will focus on unintentional injuries.
UNINTENTIONAL INJURIES
Unintentional injuries (UI) are a specific subset of injuries resulting from "the physical damage that results when a human body is suddenly subjected to energy in amounts that exceed the threshold of physiologic tolerance-or else the result of a lack of one or more vital elements, such as oxygen"8. The Maine Center for Disease Control & Prevention9 defines UI as "events in which the injury occurs in a short period of time - seconds or minutes, the harmful outcome was not sought, or the outcome was the result of one of the forms of physical energy in the environment or normal body functions being blocked by external means, e.g., drowning." Hence, UI can also result from exposure to external agents such as knives (mechanical), ultraviolet radiation (radiant), hot or cold environments (thermal), electrical shock (electrical), or poisons or drugs (chemical).
By definition, UI are unplanned and can be prevented through the implementation of safety mechanisms as well as modifications to environmental factors. The focus of this editorial is the need to avoid UI among adults in Latin America's low- and middle-income countries, and the need to promote multi-disciplinary approaches to achieve that goal. Since there are different causalities for UI around the world, we will attempt to incorporate lessons in high-income countries to accomplish that goal, keeping in mind that any efforts need to take the specific regional needs and cannot simply adopt what has been done to date10.
Data show that UI causes differ based on the country's income level. UI in low- and middle-income countries are related to factors such as fires, poor sanitation and safety in slums and squatter housing, children falling into open wells, workers falling from high trees, and people falling from transport vehicles. UI in high-income countries result from scalding hot tap water, children falling into swimming pools, adults falling down stairs, and young people falling from recreational all-terrain vehicles. However, differences are also found between countries, within countries, and even between rural and urban areas. Generally speaking, urban UI are commonly related to road or traffic issues, while rural UI are related to farming activities11-13,53.
WHO routinely publishes data about the leading causes of unintentional injuries, which include road traffic injuries (RTI), poisonings, falls, burns, and drownings. Together, these conditions are ranked among the top five leading causes of UI, have a disproportionate impact on DALYs, and harm economic output.
Given their impact on the health and wellbeing of individuals, RTIs, poisonings, falls, burns, and drownings have been identified by researchers as a top priority for preventing unintentional injuries 13-15 and will, therefore, be the focus of our discussion.
ROAD TRAFFIC INJURIES (RTI)
According to WHO17, road injuries ranked eighth as a leading cause of death in 2016 worldwide, resulting in some 1.35 million fatalities annually. Approximately, 93% of fatalities come from low- and middle-income countries 16-18,53-54,56. Negrete19 reported that Latin America and the Caribbean lead the world in RTI deaths, with an estimated economic cost of 18.9 billion dollars per year, around 1.5% of the area's gross domestic product.
Young adults, especially males, report higher rates of RTIs, showing a clear need to develop interventions targeting that population group. Educational strategies, such as the promotion of mandatory seat belt use in all seats within the vehicle, the compulsory use of child seats, and the implementation of laws regarding driving under the influence, are among the efforts healthcare providrs can promote to address UI resulting from RTIs.
In addition, physicians and public health practitioners can increase secondary prevention efforts by discussing the need to adhere to speed limits with their patients. Moreover, promoting advocacy within professional organizations to re-design traffic patterns and increase the number of roundabouts, which have shown to decrease the number of accidents at intersections and improve the flow of traffic, may be helpful. Finally, the promotion of drinking laws, similar to those instituted in Chile60; motorcycle laws, such as those in Uruguay61; and blood alcohol limits, such as those in Brazil, can be promoted by medical personnel and public health practitioners.
POISONINGS
Poisoning occurs "when a person's exposure to a natural or manmade substance has an undesirable effect." The event may be classified as self-harm or suicide, homicide or assault, and unintentional20. The mortality rate for unintentional poisoning has been rising since the 1990s, with illegal and prescription drug overdose being the predominant cause. According to reports published in the United States, drug overdose is the leading cause of accidental death, and opioids are the most common drug 21-23. In contrast, medication overdoses are the most common type of poisoning in the United Kingdom24.
WHO figures indicate that the vast majority of poisoning cases (84%) occurred in low- and middle-income countries62. In Latin America and the Caribbean, poisonings are related to snake bites, especially in rural populations. Other sources of poisoning include mercury, which is used in artisanal gold mining and in hospital equipment, methanol ingestion, and food poisoning, some of which may be related to pesticide use 25-27.
The creation of poison control centers has been a good preventive measure to decrease morbidity and mortality from exposure to chemicals at home or work. Poison control centers provide access to experts who can advise and provide assistance with the prevention, diagnosis, and management of poisonings28.
Poison control centers are not the only option. Public health practitioners and primary care medical personnel can promote public education on chemical storage, child-proof drug packaging, warning labels aimed at low-literacy populations, and ensuring access to anti-venom where snake bites are prevalent.
Medical care providers can also promote community-based prevention strategies and public advocacy measures, such as the "Safe Drinking Water and Toxic Enforcement Act," commonly known as "Prop 65" in California, USA. In addition, prescription drug monitoring programs (PDMP) have been established in many parts of the United States, and the Drug Enforcement Agency (DEA) has been helpful with statewide registries regarding controlled substances that may help to track drug usage patterns of patients21.23.
FALLS
Falls are classified as fatal and non-fatal. In 2018, WHO reported that falls were the second leading cause of unintentional injury deaths worldwide, accounting for over 600,000 deaths51. Similarly, some 17 million DALYs are lost yearly due to non-fatal falls. It is important to note that, while children account for an estimated 40% of the total DALYs worldwide, the impact of disabilities related to falls for older adults may not be accurately counted. While everyone is at risk for falls, the risk for injury increases with age, and older adults (65 and older) are at the highest risk for severe injury or death. In individuals aged 70 or older, falls are the leading classification in fatalities related to injury29-30.
WHO31 has reported that over 80% of fatalities related to falls are in low- and middle-income countries, with the global areas of South-East Asia and the Western Pacific accounting for 60% of these fatalities29. Data for Latin America are challenging to locate; however, a few studies show that patterns are similar to those around the world32,49,58.
Prevention strategies to address UI related to falls include fall risk screening, treatment of visual impairments, medication review and modification, prescription of appropriate assistive devices to address physical and sensory impairment, and prescription of hip protectors for those at risk of hip fractures. In addition, physicians can be proactive in prescribing calcium and vitamin D supplements and promoting prescribed balance training, muscle strengthening, fall prevention education, and exercise, such as Tai Chi, to strengthen balance29.
Additional strategies that public health professionals and medical personnel may promote include the distribution of easy-to-read patient information related to maintaining an orderly environment, removing objects that may be tripping hazards, adding shower/tub/toilet grab bars, adding railings on stairs, and providing adequate lighting, among others 33.
BURNS
Globally, WHO estimated that some 180,000 deaths every year result from burns36-37. WHO has also estimated that, in 2015, the vast majority (95%) of burns occurred in low- and middle-income countries. Unlike other unintentional injuries, females are at a higher risk for fatalities from burns35-36. Moreover, while burn death rates have been decreasing in many high-income countries, the rate of child deaths from burns is over seven times higher in low- and middle-income countries as opposed to high-income countries36.
Data show that most non-fatal thermal burns occur at home and in the workplace, making them highly preventable35-36. Efforts related to worker and patient education about proper safety measures may decrease burn risks at home and work. These efforts could include installing and maintaining smoke detectors, encouraging patients not to smoke in bed, distributing fire-retardant aprons, and assisting patients with medical conditions such as epilepsy, peripheral neuropathy, and physical and cognitive disabilities to handle household chores. Implementing WHO's "Plan for Burn Prevention and Care" can serve as the foundation for public health professional and medical professional providers to be actively engaged in burn prevention35-38.
DROWNINGS
Approximately 40 individuals die by drowning every hour of every day around the world39. WHO has estimated that some 320,000 individuals lost their lives to drowning in 2016, making it the third leading cause of unintentional injury death worldwide40. WHO data show that 90% of deaths occurred in low- and middle-income countries, with the highest mortality rates in Africa. Globally, the highest drowning rates occur in children one to four years of age, followed by children five to nine years of age, and males have twice the mortality rate of females due to drowning40.
According to WHO, flood disasters contribute to a large number of drowning deaths and are expected to increase in the next few years in low- and middle-income countries40. Given this imminent danger, public health professionals and medical personnel are responsible for reducing morbidity and mortality from these events. In addition to promoting the full implementation of WHO's "Preventing Drowning: An Implementation Guide" 41 (https://www.who.int/publica-tions/i/item/preventing-drowning -an-implementation-guide), public health professionals and medical personnel can promote the development of basic swimming skills by partnering with NGOs to provide free or low-cost swimming classes, improve the training of emergency personnel involved in water rescues, and develop curricula designed to promote water safety.
TAKING ACTION TO PREVENT UNINTENTIONAL INJURIES
While the incidence of injuries in general, and unintentional injuries in particular, seems to be decreasing worldwide, much work must be done to eliminate them2 Health care providers and public health care professionals are uniquely positioned to implement prevention strategies designed to mitigate their negative impact14,21,42-43, In addition to the recommendations for each of the areas discussed above, multiple best practices can be implemented in primary health care to decrease the negative impact of unintentional injuries. Specific recommendations are listed below:
ADVOCACY
The "Healthy People" initiative in the United States presents a national blueprint for addressing health issues in the country, and it establishes goals to be achieved by the end of each decade. Healthy People 2030 includes preventing unintentional injuries and violence as one of its goals44. Therefore, it is recommended that the following health promotion and disease prevention conference focuses its efforts on (1) acknowledging the clear and present danger UI represent to the wellbeing of low- and middle-income countries, and (2) developing a region-by-region plan designed to eliminate morbidity and mortality resulting from UI.
ADAPT PROVEN FRAMEWORKS FOR UNINTENTIONAL INJURY PREVENTION
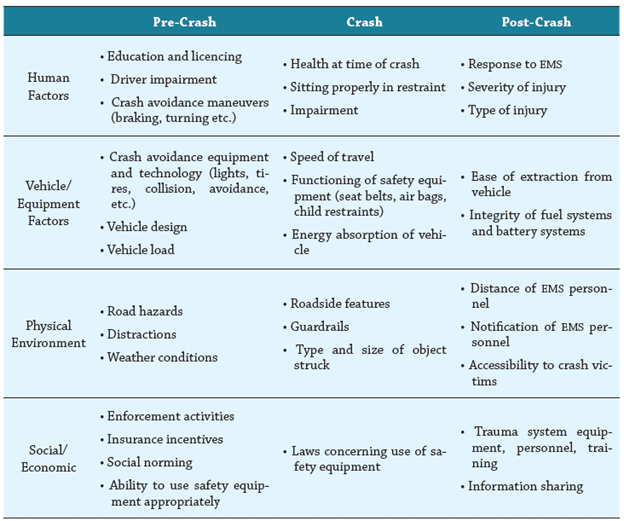
The Haddon Matrix has been proposed as a best practice to understand unintentional injury prevention and other public health issues 45-46. In addition to integrating a host-agent-environment approach, it also looks at events from pre-injury, injury, and post-injury phases and adds decision criteria to the equation.
The Haddon Matrix also incorporates all three levels of prevention, ranging from passive restraint systems in vehicles, such as airbags, to adequate response time by emergency medical technicians (EMTs). The United States National Transportation Safety Administration provides an example of this approach as related to motor vehicles (see Table 2).
IMPLEMENTATION OF PRE-HOSPITAL CARE SYSTEMS (EMS)
Robust pre-hospitalization systems have increased positive health outcomes from unintentional injuries. Decreased response rates, access to modern and working safety equipment, and anti-venom availability should be priorities for governments, public health practitioners, and medical providers to reduce morbidity and mortality indicators resulting from UI. Similarly, hospital-based trauma centers will go a long way in facilitating the treatment of UI victims63.
IMPROVEMENTS TO GLOBAL BURDEN OF INJURY SURVEILLANCE SYSTEMS
Despite their similarity with infectious and chronic diseases, unintentional injuries have characteristics that must be considered in surveillance systems. The " Steps to Develop and Maintain an Injury Surveillance System" proposed by Espitia-Hardeman & Paulozzi 47 provide a recommended structure for its implementation (See Table 3).
Table 3 Steps to Develop and Maintain an Injury Surveillance System
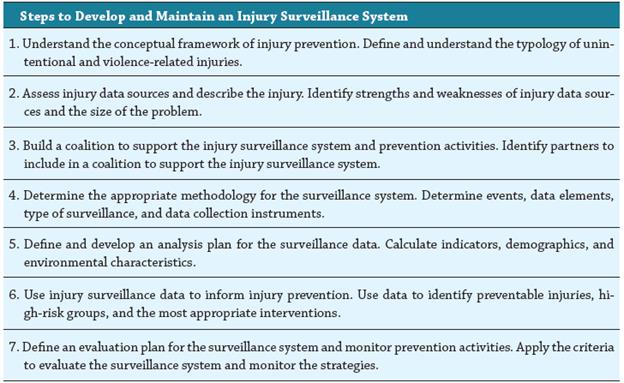
Source: Espitia-Hardeman & Paulozzi 47
In Latin American and Caribbean countries, these efforts should include specific steps to improve data sharing and quality, including data integrity and validity and the standardization of data collection and presentation methods. Furthermore, the data should include morbidity and mortality rates, economic costs, and long-term disability data. Participants in the surveillance system should consist of ministries of health, hospitals, health care centers, epidemiologists, general practitioners, health promoters, and paramedics, to name a few.
The scope of issues falling under unintentional injuries can be daunting to any surveillance system. Therefore, any system will require prioritizing health events, quantifying the magnitude of the problem, enumerating the impact on DALYs, documenting the trend of events, identifying local interest in the issues, and cost. Finally, any surveillance system must have strong privacy and confidentiality measures,48.
CONCLUSION
Injuries can be classified based upon intentionality, whereby intentional injuries are generally a result of purposeful action, while unintentional injuries are unplanned and unintended. Injuries differ from diseases as injuries are more acute, and the appearance interval is much faster than chronic or infectious diseases. While the words "injury" and "accident" may be considered synonyms, experts suggest that they are not the same, and the word "accident" should be avoided.
It should be noted that injury-related costs include monetary expenditures related to emergency services, hospital inpatient and outpatient costs, office-based services provided by medical providers, rehabilitation, long-term care, and administrative costs. Additional costs may include legal and court fees, human services (including welfare), and funeral and medical examiner costs.
Researchers have identified preventing unintentional injuries, including road traffic injuries (RTIs), poisonings, falls, burns, and drownings, as a top priority in positively impacting the health and wellbeing of individuals in low- and middle-income countries. Environmental modifications world-wide are recommended to decrease negative impacts from unintentional injuries. Safer cooking environments, the enclosure of open water areas (e.g., ponds), safer roads, and law enforcement have been successfully implemented worldwide as strategies to decrease UI.
The prevention of UI will require emphasizing primary prevention efforts (e.g., the use of seat belts) and the implementation of a multidiscipline approach to prevention, which is why we have focused on recommending partnerships between public health and medicine to jointly develop and implement science-based interventions. These strategies will require a national commitment to decreasing unintentional injuries, modifying environmental factors, advocating for regulatory measures, and taking steps to change behavioral pathogens at the individual level. In addition, community-based interventions, like those successfully implemented in high-income countries to decrease injury rates, will need to be implemented in low- and middle-income countries.