Introduction
In the era of primary percutaneous coronary intervention, mechanical complications after acute myocardial infarction (MI) such as post MI ventricular septal rupture (VSR) are pretty rare, with an incidence less than 0.5%. Nevertheless, despite its declining incidence, current mortality remains extremely high- 30-day mortality of 100% with medical treatment and 42.9%, mortality with surgical treatment in current series- and appears mostly unchanged over the last few decades.1,2
In relation to surgical repair the mortality varies significantly depending on timing of surgery with a 54.1% mortality in patients who underwent surgery within 7 days of presentation compared with 18.4% mortality if repair is delayed after 7 days.3 Patients who are at high risk of perioperative death include those with cardiogenic shock and multiorgan dysfunction. In this group a mechanical circulatory support such as an extracorporeal membrane oxygenation (ECMO) circuit could be used as bridge to surgical repair is feasible or heart transplantation, as it provides hemodynamic stability and the potential to correct multiorgan dysfunction.1
Case presentation
A 69-year-old man, current smoker, with previous medical history of systemic arterial hypertension was assisted in his home by the emergency medical service based on intermittent oppressive thoracic pain that had persisted for 48 hours. An electrocardiogram revealed sinus rhythm with ST segment elevation and significant Q waves in anterolateral leads - general treatment measures for ST segment elevation myocardial infarction including sublingual nitroglycerin, anticoagulant with unfractioned heparin and dual antiplatelet therapy-were initiated. He was immediately transferred to the cardiac catheterization laboratory for an emergent coronary angiogram. At his arrival to the hospital, the physical examination of the patient revealed a harsh, pansystolic murmur, as well as a palpable thrill without bibasilar pulmonary crackles. Due to the previous finding a VSR complicating MI was suspected. A transthoracic echocardiogram demonstrated drop out of the apical ventricular septum and the presence of flow across the septum using color Doppler confirming the diagnosis of VSR. Severe left ventricular (LV) dysfunction and apical thinning compatible with a pseudoaneurysm were also noted. The right ventricular function was preserved. The previous findings were confirmed by a transesophageal echocardiography (fig. 1A) (Video 1-3: available in on line supplementary material). Three vessel significant coronary artery disease was observed in the coronary angiogram and an intra-aortic balloon pump was implanted to decrease LV afterload with diminishing of the shunt volume and to improve the coronary blood flow. Suddenly, the patient became hemodynamically unstable with multiorgan dysfunction requiring treatment with vasopressors and invasive mechanical ventilation. An emergent cardiothoracic consultation was performed. The Heart Team discussed the case and the surgical option was dismissed because of the large extent of the VSR, possible pseudoaneurysm and coronary artery bypass surgery. A central veno-arterial ECMO was implanted as a bridge to candidacy for heart transplantation with initial hemodynamic improvement achieved (fig. 1B). Unfortunately, while on the waiting list for heart transplantation with maximum priority the patient had massive hemoptysis secondary to diffuse alveolar hemorrhage and died.
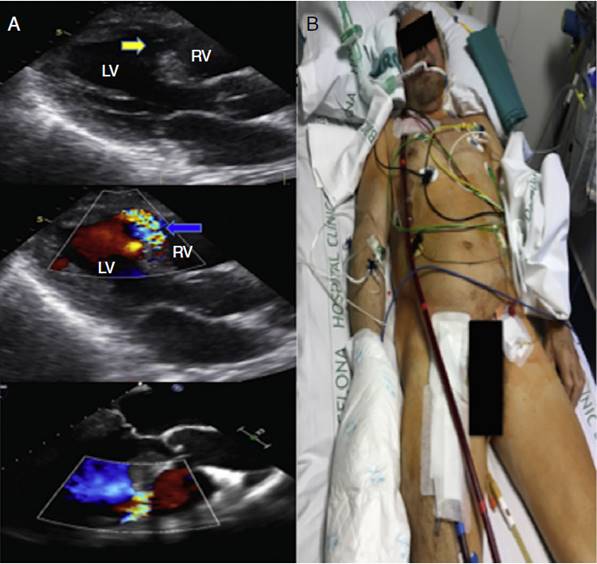
Figure 1 A transthoracic and transesophageal echocardiogram demonstrated drop out of the apical ventricular septum (Yellow arrow) and the presence of flow across the septum using color Doppler confirming the diagnosis of VSR. (Blue arrow) Severe left ventricular (LV) dysfunction and apical thinning compatible with a pseudoaneurysm were also noted. Figure 1 B A central veno-arterial ECMO was implanted as a bridge to emergent heart transplantation. The venous access was located at the right atrium and the arterial access at the right femoral artery.
Discussion and conclusion
The use of circulatory support in the form of an ECMO device in post infarction VSR is an adequate option to stabilize patients until surgery, when the cardiac function can be recovered with either primary repair or transplant, and medical treatment to stabilization is unsuccessful, and emergent surgery has prohibitive risk. Rozado et al.4 described a successful case of ECMO device use in post infarction VSR to stabilize patients suffering cardiogenic shock until favorable delayed surgical repair was performed. Pascual et al.5,6 reported the experience of ECMO device implantation as a bridge to successful heart transplantation in an unusual case with 2 mechanical complications of myocardial infarction-a post infarction VSR and LV pseudoaneurysm-considered surgically irreparable.
However, circulatory support in the form of an ECMO device is not free of complications, such as dreadful bleeding secondary to the anticoagulation required by the equipment like in our case or vascular and infectious complications.5
Oxigenación central por membrana extracorpórea, como puente hacia la decisión en un paciente con ruptura del septum ventricular, como complicación del infarto de miocardio














