Introduction
Cardiac tumors are rare and often unrecognized until autopsies are performed, before 1951 diagnosis was exclusively post-mortem1. Primary cardiac tumors are mostly benign (75 %), the most common type being myxoma in half of those cases1-4. Although myxomas’ incidence is rare (0.001-0.1 %)3-4, it is prevalent in all ages and appears in the left atrium in 60-85 % of the cases, rarely biatrial (5 %), with an average size of 5-6cm3-5. It is believed that myxomas arise at the cardiac septation from mesenquimal multipotent cells that persist as embryonal residues or from endocardial neural cells5.
Their clinical course varies depending on: attachment site, number of masses, comorbidities, recurrence, calcification and/or necrosis, and symptoms. Some can be completely asymptomatic (10 %)4, while others can have systemic symptoms (34-90 %)4-5 or valvular syndrome including sudden death6. A large percentage of patients debut with embolic complications (30-50 %)2-5.
The diagnosis is often incidental via non-invasive images such as echocardiography, computed tomography (CT) scan, or magnetic resonance imaging (MRI)6, often as a result of heart failure/angina (67 %) or constitutional symptoms (13-34 %)3. The main diagnostical tool and follow-up is the echocardiography3,4,6, either transthoracic or transesophageal, however often more extensive images are required to characterize the tumor.
Symptomatic patients require urgent surgical resection to prevent complications2,3,6, with a postoperative mortality of 1.7-7.5 %3,5, recurrence of 1-4 %3,4,6, and 5-year survival rate of 83 %2. Classically, in left atrium myxomas, a standard median sternotomy with a bicaval cardiopulmonary bypass has been performed, with resection through a right atriotomy and transseptal access. Interatrial septum defect is then corrected directly or with a pericardial (PTFE or Dacron) patch3. In complex tumors, a biatrial approach is often considered.
Recently, minithoracotomy with robotic and video-assisted resection has been performed, however the risk of incomplete resection is higher. Other accessible minimally invasive surgical alternatives such as a minithoracotomy with direct vision have been applied6-7.
Cases
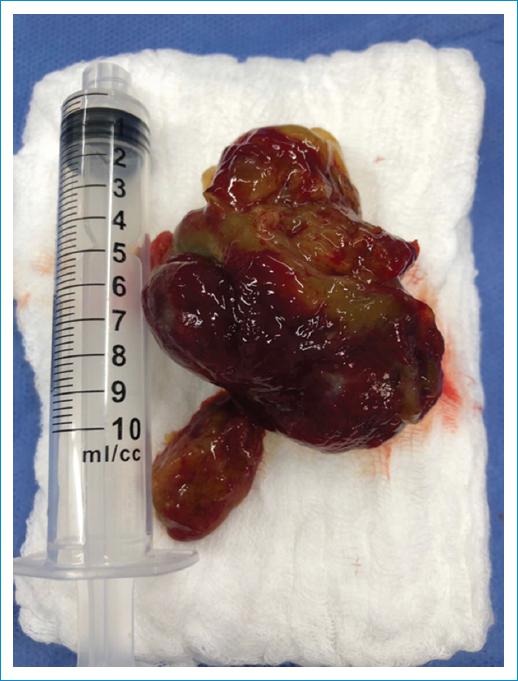
It is presented three cases of minimally invasive myxoma resection via the right lateral minithoracotomy. In all three cases, diagnosis was made via echocardiography (Fig. 1). Patient one is a 59-year-old female with a 1.5 cm myxoma, patient two is a 74-year-old male with a 6x4 cm myxoma (Fig. 2) and patient three is a 24-year-old female with a 3.8 cm x 3.3 cm myxoma.
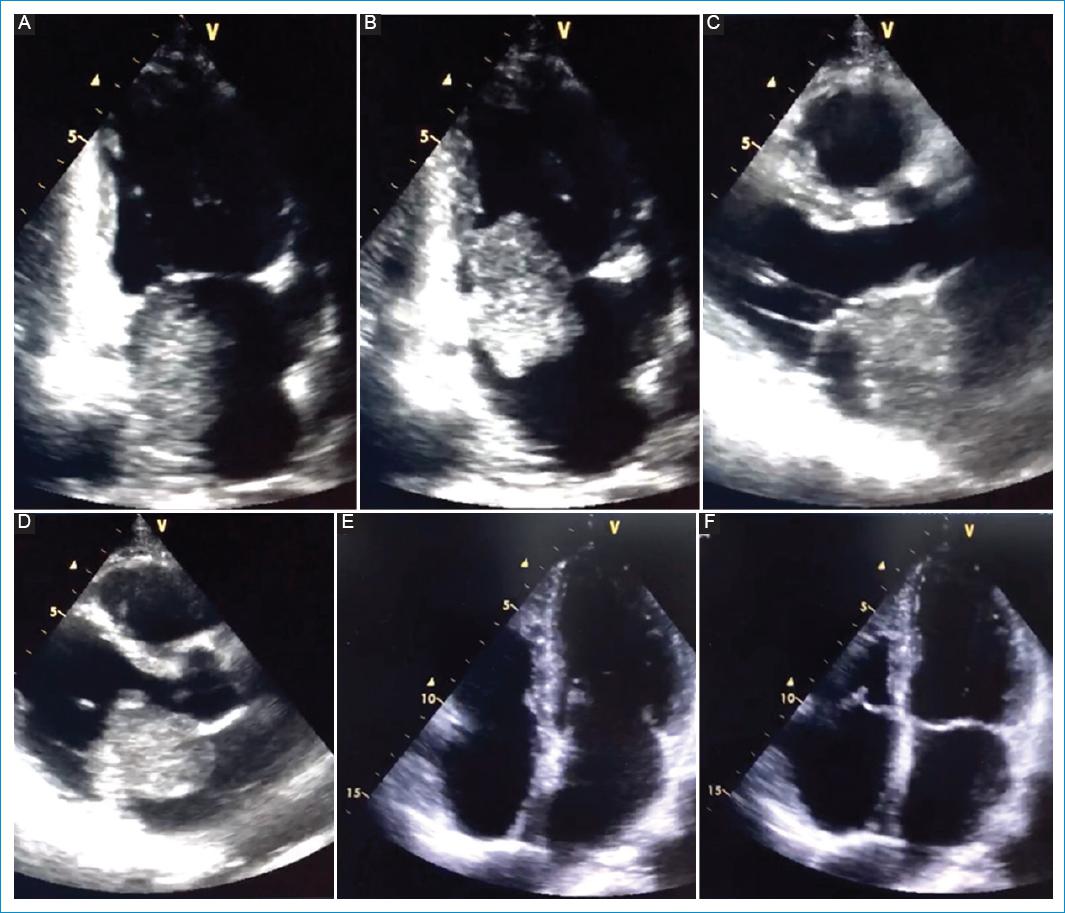
Figure 1 Echocardiography of patient 1 with the myxoma visible (A-D) as well as out-patient echocardiography posterior to resection (E-F).
Under general anesthesia, previously inserting a central venous access (internal jugular right vein) and arterial line (left radial artery), patient was heparinized at a dose of 3 mg/kg. The right lateral minithoracotomy incision was performed, dissection of femoral blood vessels with posterior distal and proximal repair (purse string suture with 5/0 prolene in right common femoral arterial and purse string suture with 5/0 prolene in right femoral vein with Seldinger technique for superior vena cava cannulation through the right jugular vein). Once the activated coagulation time was >500 ms, the canulation of the femoral artery was achieved with Bio-Medicus 17 fr (patient 3)/19 fr (patient 2)/21 fr (patient 1), the femoral vein with a multiperforated cannula 25 fr, and the jugular vein with 15 fr. The MiAR cardioplegia cannula was inserted in the aortic root, then the corporal temperature was reduced to 34°C to ensure an adequate pinching of the aortic root and posterior infusion of the high-potassium concentration crystalloid cardioplegic solution as well as cold topic saline solution until achieving complete cardioplegia. This allowed the extracorporeal circulation to be completed without any complications.
Once the myxoma resection was completed, the left atrium is closed with a continuous sutured with prolene with previous lavage to remove any thrombi. The corporal temperature was increased to 32°C to uncinch the aortic root and allow reperfusion. The heart regained electrical activity with a sinus rhythm, to posteriorly suspend the extracorporeal circulation pump at 37°C. In patient 2, the heart regained electrical activity with a ventricular fibrillation requiring 200 J discharge with reversion to sinus rhythm. Decannulation was then completed with suture reinforcement and once hemostasia was completed, an electrode was placed in the ventricular epicardium as well as mediastinal and pleural tubes to posteriorly close the thoracic cavity with one or two 1/0 vicryl sutures, fascia with 2/0 vicryl, and skin with 4/0 vicryl. Coagulation time control was completed using 5 cartridges in the Automated Coagulation Timer.
Results
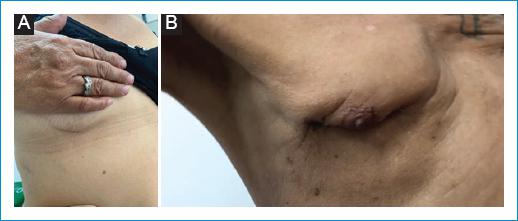
Resulting biopsies of all excisions confirmed complete resection of each mass as well as confirmation of a myxoma. All patients had an in-hospital stay without any complications reported, requiring ICU-stance as routine post-operatively cautionary follow-up (Table 1) and intravenous ionotropic drugs during the immediate post-op. The only slight intra-operative complication was with patient 2 whom presented ventricular fibrillation in the return of electrical activity, successfully reverted with one electrical discharge. In the out-patient follow-up, patients one and two had minimal scars post-surgically (Fig. 3). All interventions were performed successfully without any peri-operative complications or mortalities, with ICU stay Quality of life scale (SF-36) was applied 6 and 12 months postoperatively with scores above 90 %. Additionally, patient 1 had echocardiography immediately, 2 months and 28 months postoperatively; patient 2 had echocardiography at 1 month and 8 months postoperatively; patient 3 at 1 month and 16 months postoperatively; all reports with a conserved ejection fraction and without any masses visible.
Table 1 Characteristics of the three patients who underwent minimally invasive myxoma resection via the right lateral minithoracotomy
| Patient | Gender | Age | Location and LVEF ( %) | Size (cm) | Symptoms | Pump time (min) | Clamp time (min) | Bleeding | Days hospitalized |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 59 | Posterior interatrial septum (0.9 x 0.7 cm) and LVEF 74% | 1.5 x 1.5 | Presyncope | 103 | 37 | Limited (< 300 ml) | Pre-Op: 10 ICU Post: 6 Floor: 3 Total: 19 |
| 2 | Male | 74 | Left atrium (4.9 x 4.6 cm) and LVEF 63% | 6 x 4 | Progressive dyspnea | 90 | 45 | Limited (< 300 ml) | Pre-Op: 6 ICU Post: 2 Floor: 2 Total: 10 |
| 3 | Female | 24 | Left atrium embedded in septum and LVEF 57% | 3.8 x 3.3 | 6 months of atypical chest pain, progressive dyspnea | 91 | 44 | Limited (< 300 ml) | Pre-Op: 1 ICU Post: 4 Floor: 1 Total: 6 |
Discussion
Compared to other cases series in the literature, reports in our study were consistent in the average clinical course. Although a small sample size, all three were diagnosed via echocardiography and none reported any complications or mortality peri-operatively. We describe the most relevant findings (Table 1), while comparing worldwide similar case series reports (n >17) albeit with a much larger sample size (Table 2). In this setting, our cases represent similar findings with respect to symptoms, bleeding, and peri-operative morbidity and mortality. Although other cases series usually do not report pump and clamp time, our time settings are within range of averages reported in other literature, as well as myxoma size and location3-5. Unfortunately given that in the three cases the in-hospital stay was very variable, we cannot ensure this as an advantage, a larger sample size is required.
Table 2 Characteristics of other case series reported in the literature (n>17) as comparison
| Authors | Patients | Symptoms | Mortality | Complications |
|---|---|---|---|---|
| Pinede et al. | 122 | Cardiac failure signs (43%). Syncope (14%). Palpitations and thoracic pain (30%). Fever (20%). Constitutional (18%). Embolic events (29%). |
3.5%. | Arrythmias 29%. Recurrence (5%). |
| Barnes et al. | 18 | Cardiac failure signs (44%). Embolic events (27%). Arrythmias (27%). | 0%. | Atrial fibrillation (5%). |
| Muthubaskaran et al. | 32 | Cardiac failure signs (47%). Embolic events (34%). Constitutional (32%). | 0%. | Recurrence (6%). Peripheral embolus (6%). Pulmonary embolism (3%). |
| Garatti et al. | 98 | Dyspnea (68%). Palpitations (38%). Cardiac failure signs (30%). Embolic events (35%). Constitutional (57%). |
3%. | Recurrence (1%). |
| Lee et al. | 93 | Dyspnea (38.7%). Thoracic pain (21.5%). Palpitations (8.6%). Embolic events (10.8%). Syncope (5.4%). |
3.2%. | Recurrence (2.1%). |
| Lin et al. | 68 | Dyspnea (57%). Palpitations (46%). Syncope (21%). Cardiac failure signs (21%). Constitutional (35%). Embolic events (24%). |
2.8%. | Pleural effusion (22%). Low output syndrome (7%). Atrial fibrillation (6%). Pericardial effusion (4%). Pneumothorax (3%). Pneumonia (3%). Respiratory failure (1.5%). |
| Jawad et al. | 269 | Dyspnea (34.9%). Arrhythmias (21.2%). Embolic events (13.4%). Thoracic pain (10.8%). |
1.9%. | Arrhythmias (28.3%). Syncope (10%). Respiratory insufficiency (3.3%). Pericardial effusion (3.3%). Peripheral embolus (1.1%). |
| Gandara et al. | 18 | Dyspnea (35%). Thoracic pain (28%). Constitutional symptoms (20-22%). Syncope (14%). |
17%. | Not reported. |
These results emphasize evidence that a minimally invasive myxoma resection via the right lateral minithoracotomy can be the ideal approach in myxoma resection, specifically in Colombia where open surgery is often chosen based on lack of expertise or equipment/personnel available. We believe we can promote the use of this alternative surgical approach, especially in Colombia, given the promising results shown worldwide and locally.
Conclusions
Cardiac tumors are rare and often unrecognized until autopsies are performed, the most common type being the myxoma. Although the surgical approach is varied depending on the expertise, cost and equipment available, recently a minimally invasive myxoma resection via the right lateral minithoracotomy has been proposed as an ideal approach. We believe the case reports in this manuscript provide an idea for future surgical techniques as the patient outcomes are promising compared to open surgeries. We hope these excellent results promote further research in Colombia as well as increase education to ensure it becomes the norm.