Introduction
Acute kidney injury (AKI) is a frequent complication in children undergoing cardiac surgery for congenital cardiac disease1,2. Acute kidney injury network (AKI) can compromise clinical evolution and affect the prognosis of the patients. The number of days in mechanical ventilation, ICU stay and mortality increase up to 18%3-5 in patients with this complication. Even though this topic has been widely studied, most reports come from Europe, North America, and Australia, but there are a few studies in Latin America4,6 and no previous reports in Colombia.
The aims of this study were to determine the incidence, severity and risk factors of AKI in children undergoing cardiac surgery in a tertiary care center in Cali, Colombia and to evaluate its impact on mortality, duration of mechanical ventilation, ICU and total hospital length of stay.
Methods
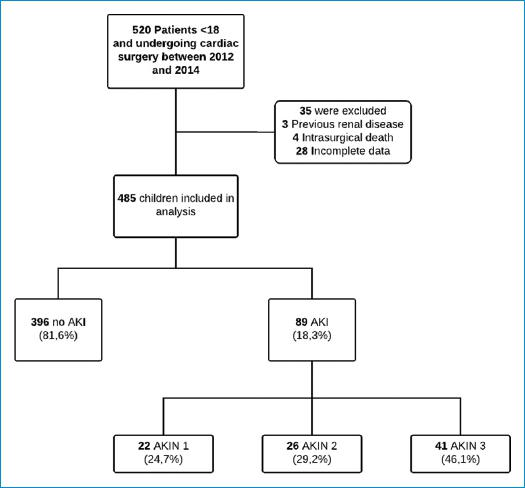
After approval of the Institutional Review Board of Centro Médico Imbanaco de Cali S.A, we performed a historical cohort of pediatric patients undergoing cardiac surgery. We reviewed the cardiac registry to identify children from newborn to 18 years of age who underwent this procedure for congenital heart defects between January 2012 and June 2014. Cases with incomplete data, previous renal disease, and those who died during surgery were excluded (Fig. 1).
Study variables
We performed a search of the electronic medical records, anesthesia and surgical charts and collected the following variables:
PRE-OPERATIVE VARIABLES
These included age, sex and pre-surgical creatinine. We used the RACHS scoring system to categorize the complexity of surgery7. This method is widely accepted for the evaluation of differences in outcomes of surgery for congenital heart disease. The score was determined for each patient by the cardiac surgery group and an anesthesiologist prior to surgery.
AKI definition
The Acute Kidney Injury Network (AKIN) definition8 was used to define AKI. Serum creatinine prior to surgery was used to calculate baseline renal function. Increased in serum creatinine of 0.3 mg / dl were classified AKIN 1, doble baseline serum creatinine AKIN 2 and triple base line serum creatinine AKIN 3. We classified AKIN stage using the highest serum creatinine concentration identified during the entire length of ICU stay after cardiac surgery. We did not use urine output since it could be influenced by diuretic use.
Statistical analysis
We performed univariate analysis with chi-square test or Fishers exact test for categorical variables. Continuous variables were compared using Student t test or Mann-Whitney U test. A logistic regression model was applied to determine risk factors associated with AKI. Model selection was performed using a backward selection methodology based on Akaikes Information Criteria. In the multivariable model we included variables that reported p < 0.20 in the crude analysis. The odds ratio (OR) was estimated with its 95% confidence interval (CI). Goodness-of-fit was evaluated with the likelihood ratio test and model deviance. We estimated crude OR and OR adjusted for age, time of CPB and RACHS scale to compare the clinical outcomes between groups. In the multivariable analysis, categories 4-6 of the RACHS scoring were combined due to the small number of children in these categories. All analyses were carried out using Stata 13 (STATA Corp, College Station, TX).
Results
Study population and AKI incidence
Table 1 shows the main characteristics of the patients who developed AKI compared to those without AKI. During the 30-month study period, 485 children who underwent cardiac surgery were included in the analysis: 84 (17.3%) were neonates and 238 (48.1%) were less than two years of age. Among the patients with AKI, 55.1% were male. According to the RACHS scale, 34.4% (167) of the procedures were at medium or high surgical risk (RACHS: 3-6). During the study period, the overall mortality rate was 14.4% (70/485), and the incidence of post-operative AKI was 18.3% (89 cases; 95% CI: 15.1%-22.0%). The most of these patients were classified as AKIN score 3 (41/89). The incidence of AKI decreased gradually from year 1 (23%) to year 3 (11%).
Tabla 1 Characteristics of the patients according to occurrence of AKI
| Variables | AKI (n = 89) | No AKI (n = 396) | p value |
|---|---|---|---|
| Age, n (%) | |||
| ≤ 30 days | 32 (35.9%) | 52 (13.1%) | <0.001 |
| > 30 days ≤ 2 years | 39 (43.8%) | 199 (50.2%) | |
| >2 years < 13 years | 14 (15.7%) | 122 (30.8%) | |
| ≥13 years < 18 years | 4 (4.5%) | 23 (5.8%) | |
| Sex, n (%) | |||
| Female | 40 (44.9%) | 188 (47.6%) | 0.590 |
| Male | 49 (55.1%) | 208 (52.5%) | |
| RACHS, n (%) | |||
| Median (IQR) | 3 (2-3) | 2 (1-3) | |
| 1 | 7 (7.9%) | 114 (28.8) | |
| 2 | 24 (26.9%) | 173 (43.7) | |
| 3 | 44 (49.4%) | 93 (23.5%) | |
| 4 | 10 (11.2%) | 12 (3.0%) | |
| 6 | 4 (4.5%) | 4 (1.0) | <0.001 |
| CPB, n (%) | 81 (91.0%) | 335 (84.6%) | 0.117 |
| CPB time, n (%) | |||
| 0-60 min | 23 (25.8%) | 225 (56.8%) | <0.001 |
| 61-120 min | 21 (23.6%) | 128 (32.3%) | |
| 121-180 min | 33 (37.1%) | 33 (8.3%) | |
| >180 min | 12 (13.5%) | 10 (2.5%) | |
| Ischemic, n (%) | 69 (77.5%) | 264 (66.7%) | 0.046 |
| Ischemic time, n (%) | |||
| 0-60 min | 42 (47.2%) | 293 (73.9%) | <0.001 |
| 61-120 min | 28 (31.5%) | 88 (22.2%) | |
| 121-180 min | 16 (17.9%) | 14 (3.5%) | |
| > 180 min | 3 (3.4%) | 1 (0.2%) | |
| DHCA, n (%) | 10 (11.2%) | 14 (3.5%) | 0.002 |
| MV duration, n (%) | |||
| > 2 days | 55 (63.9%) | 43 (10.9%) | <0.001 |
| Median (IQR) | 5 (2-9) | 1 (1-2) | |
| ICU length of stay | |||
| > 7 days | 60 (68.2%) | 142 (35.9%) | <0.001 |
| Median (IQR) | 12 (4-21) | 6 (4-9) | |
| Length of stay | |||
| >7 days | 70 (82.3%) | 221 (56.5%) | <0.001 |
| Median (IQR) | 8 (6-17) | 19 (10-33) | |
| Mortality, n (%) | 40 (44.9%) | 30 (7.6%) | <0.001 |
CPB: cardiopulmonary bypass; MV: mechanical ventilation; ICU: intensive care unit; DHCA: deep hypothermic circulatory arrest.
Risk factors for AKI development
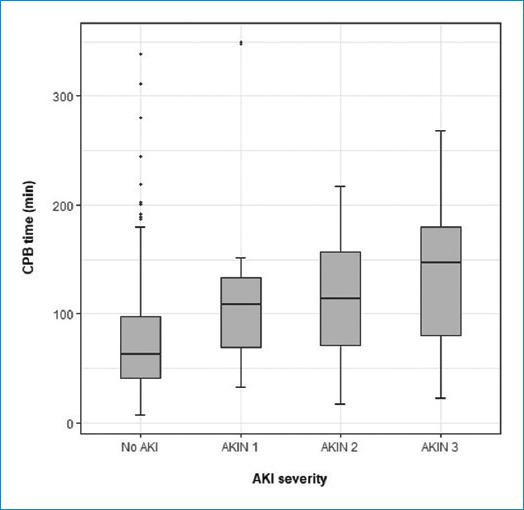
The univariate analysis showed that patients with AKI were younger (2.67 years ± 0.23) vs. the patients without AKI (3.65 years ± 0.22). The use of ischemia was higher among AKI cases (77.5% vs. 66.7%; p = 0.046), and a higher proportion of cases had an ischemia time >120 min (21.3% vs. 3.7%: p < 0.001). Proportion of patients undergoing CPB did no differ between the groups with and without AKI (91% vs. 84.6%; p = 0.117), but 50.6% of the cases with AKI were on CPB for more than 120 min vs. 10.8% without AKI (p < 0.001) (Table 1). Fig. 2 shows that there is a tendency to develop a more severe type of AKI among the patients with a longer CPB time. This difference was more notorious between the patients with AKI stage 3 compared to patients without AKI and stages 1 and 2.
The multivariable logistic regression model identified age, RACHS score and CPB time as risk factors for AKI development. Neonates and children younger than two years of age had the highest cumulative risk of post-operative AKI (Table 2). The patients with RACHS category 3 had 3.74-fold the odds of developing AKI than those with RACHS category 1. Although, approximately half of the patients with RACHS category 4 to 6 developed AKI after cardiac intervention, evidence was insufficient to support differences between high-risk and low-risk procedures (p = 0.49) (Table 2).
Tabla 2 Risk factors and outcomes of acute kidney injury after cardiac surgery
| Risk Factors | |||
|---|---|---|---|
| Variables | Total (n = 485) | ||
| % (n) AKI | OR (CI 95%) | p value | |
| Age, n (%) | |||
| ≤ 30 days | 38.1% (32) | 1 | |
| > 30 days ≤ 2 years | 16.4% (39) | 0.36 (0.18-0.74) | 0.005 |
| > 2 years < 13 years | 10.3% (14) | 0.15 (0.06-0.36) | 0.000 |
| ≥ 13 years < 18 years | 14.8% (4) | 0.16 (0.04-0.65) | 0.010 |
| RACHS | |||
| 1 | 5.8% (7) | 1 | |
| 2 | 12.2% (24) | 1.71 (0.67-4.34) | 0.260 |
| 3 | 32.3% (44) | 3.74 (1.48-9.40) | 0.005 |
| 4,5,6 | 46.7% (14) | 1.55 (0.43-5.54) | 0.497 |
| CPB time, min | |||
| < 60 | 9.3% (23) | 1 | |
| 61-120 | 14.1% (21) | 1.55 (0.79-3.05) | 0.203 |
| 121-180 | 50.0% (33) | 6.98 (3.25-14.98) | <0.001 |
| >180 | 54.5% (12) | 10.87 (3.63-32.53) | <0.001 |
| Outcomes | |||
| Total (n = 485) | |||
| Variables | Crude OR [CI95%] | Adjusted OR [CI 95%]* | p value |
| MV duration | |||
| > 2 days | 14.44 [8.40; 24.84] | 14.69 [6.60-32.67] | <0.001 |
| PICU length of stay | |||
| > 7 days | 3.83 [2.34; 6.28] | 3.99 [1.83;8.71] | <0.001 |
| Length of stay | |||
| > 7 days | 3.59 [.98; 6.49] | 2.81 [1.10;7.17] | <0.001 |
| Mortality | 9.96 [5.69; 17.42] | 5.82 [2.24; 15.10] | <0.001 |
*Model adjusted for age, CPB time, RACHS scale.
CPB time was higher among the patients that developed AKI. 50% of patients with prolonged CPB time (>120 min) developed AKI postoperatively. The patients undergoing procedures with a CPB time between 121 and 180 min were 7 times more likely to develop AKI than those who underwent a CPB with a duration of <60 min (p < 0.001). The odds increased 10.9-fold in patients with a CPB time of >180 min (p < 0.001) (Table 2).
AKI associated outcomes
Children with AKI had increased time on MV. The median number of days on MV was greater for patients with AKI than for patients without it (5 vs. 1 day, p < 0.001). In the adjusted model, we found that the odds of requiring MV for 2 days after surgery was 14.69-fold in children with AKI compared to patients without post-operative AKI (CI 6.6-32.67, p < 0.001, Table 2).
The length of ICU stay was 12 days for patients with AKI and 6 days for patients without AKI (Table 1), and the odds of having an ICU stay >7 days was 3.99-fold in children with AKI when compared to the ones without it (CI 1.83-8.71, p < 0.001, Table 2).
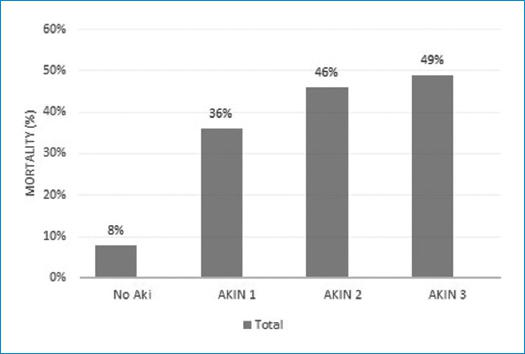
In-hospital, mortality was higher in patients who developed post-operative AKI (AKI: 44.9% (40/89) vs no AKI: 7.6% (30/396)), and increased gradually with the AKIN scale risk (Fig. 3). After model adjustment, the odds of death were 5.82-fold higher among patients with AKI (CI 2.24-15.1, p < 0.001) (Table 2).
Discussion
The results of this study showed that the incidence of AKI after cardiac surgery using the AKIN definition was 18.3%, and morbidity and mortality increased with AKI severity. Neonates had higher risk of developing AKI when compared to older children.
The incidence of AKI using the AKIN scale was 18.3%, compared with 11% reported prior to AKI definitions1. Later reports using the pRIFLE scale to define AKI reported 36%9 and 20%3. In a study comparing systems for identification of post-operative AKI in pediatric cardiac patients, the AKIN scale was more specific compared with the pRIFLE and KDIGO and detected mostly high-risk patients across all age groups10. Multiples studies have proven that the AKI scales allow for classification of AKI severity and also determines prognosis and mortality3,4,11. The AKIN scale in the present study was able to classify the severity of AKI and it correlated with prognosis. Of note, for AKI staging we only used increasing creatinine sincef urine output could be influenced by the use of diuretics12.
The incidence of AKI in our study was lower than estimates in previous studies5. This difference might be related to improvements in cardiac surgery techniques over the past decade. As reported in other studies, the AKI incidence decreased through the years of the program, from 23% in the first year to 11% in the third one, however the CPB duration has remained similar over the years13,14. Adjustment in anesthesia protocols, the use of pre-operative checklists, and recognition of high-risk patients are some of the changes that could explain this difference. Compared to other studies in Latin America, AKI incidence in the present study was somewhat lower when compared to studies done in Brasil (25%)4 and Mexico (34%)6.
In our study, CPB time and younger age were the main factors in the development of AKI after cardiac surgery for congenital heart disease. The previous reports have shown that CPB is a risk factor for developing AKI3-5,11,13. We found that CPB use, by itself, did not influence significantly the AKI risk (p 0.117), but time of CPB did, the longer the CBP time, the greater the risk of developing AKI and a higher AKIN stage.
Neonates were at higher risk of AKI, in this age group the incidence of AKI has previously been reported to be as high as 60.9% using the pRIFLE criteria15 and 64%16 and 62%5 using the AKIN score definition. The higher incidence of AKI in neonates can be explained by body size, renal development related to gestational age, and birth weight.
The development of AKI increased mortality. There is a progressively higher mortality rate at each AKIN severity stage. Similar findings were reported by Alabbas et al.5 in a study of 76 neonates performed in Canada who developed AKI after cardiac surgery. In that study, the mortality rate was 14% compared with 4% in neonates without AKI; increments in mortality rate were found in the AKIN 3 score.
The recent studies have shown that differences in mortality rate can extend beyond the immediate post-operative period in patients with AKI, especially in those with stage AKIN 3 or pRIFLE failure stage17. In a study of 418 patients with AKI after cardiac surgery, 22% died during the 2-year follow-up period18. The TRIBE-AKI study19 found that in 131 children who had AKI after cardiac surgery, 17% had hypertension, 8% had microalbuminuria, and 14% had a glomerular filtration rate less than 90 mL/min/1.73 m2 at 5-year follow-up. These data emphasize the importance of long-term follow-up of renal function and blood pressure in patients with AKI after cardiac surgery.
Knowing the risk factors for post-surgical AKI may contribute to take preventive measures such as placement of peritoneal catheter during surgery in patients with prolonged CPB time and higher RACHS, in fact this has showed to improve early management of AKI20.
Among the limitations of this study, it was retrospective with the subsequent problems of insufficient data in the medical registries. It was a single center study with high proportion of neonates who are the ones with higher risk for AKI. Multicenter studies with a longer follow-up would be necessary to evaluate more the long term outcomes of these patients
AKI definitions have improved the diagnosis and treatment of AKI after cardiac surgery. New biomarkers, such as neutrophil gelatinase–associated lipocalin, kidney injury molecule 1, and cystatin C, have been investigated and soon will guide the early detection and severity of AKI after cardiac surgery21,22. Serum cystatin C concentration has been shown to predict AKI as early as 8 hours after CPB23. Earlier recognition and intervention of AKI can improve management and prognosis. Future studies using these biomarkers will help to guide earlier clinical interventions in the management of AKI.
Conclusions
AKI is a frequent complication after cardiac surgery. Risk factors for AKI are younger age, higher RACHS score, and time of CPB greater than 120 min. AKI increases mortality, days on MV, and ICU and total hospital stay. In the present study, the AKIN scale allowed us to classify the severity of AKI and it correlated with prognosis after cardiac surgery.