Introduction
With the increase of life expectancy, probability of occurrence of the chronic diseases and the need for medication increases1,2. In general, the term polypharmacy is defined simultaneous use of several drug molecules3. The results of a systematic review of 110 articles between 2000 and 2016 showed that the most common definition (in 51.5% of articles) is the consumption of five different drugs and more, at the same time4. The probability of poly pharmacy in cardiovascular diseases is higher than other chronic diseases5. The most common complications of polypharmacy include drug interactions, drug errors, adverse drug events and reactions, side effects, re-hospitalization, and also increased cost of treatment6. Along with normal aging, the cognitive abilities decrease, due to structural and functional changes in different parts of nervous system7. Annually, about 1-2% of the general population and 10-15% of people involved in mild cognitive impairment will develop dementia8. Although, it has been shown in many studies that polypharmacy has a significant statistical relationship with cognitive impairment9-13, such a relationship was not found in some other studies14-17. In our country, although the status of poly pharmacy in the elderly has been examined in several descriptive studies3,18-20, such a study has not been conducted, as far as the present researchers have examined the available information databases. Therefore, considering that the probability of polypharmacy is higher in people with cardiovascular diseases, the aim of this study was to determine the relationship between polypharmacy and cognitive status and its subdomains in the elderly referring to Sari Heart Center Clinic. Careful analysis of the medication regimen and the status of cognition of the elderly are two of the four main areas of age-friendly care systems21. The researchers hope that the results of this study be useful in reducing the inappropriate prescription of drugs and their consequences, providing educational programs for physicians and pharmacists; and raising the awareness of families.
Materials and method
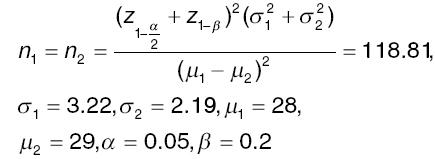
In this cohort study, 240 elderly people, referred to the Sari Heart Center Clinics, were selected, based on inclusion criteria. This study was approved by the Ethics committee of the Mazandaran University of Medical Sciences with Code IR.MAZUMS.REC.1398.6120. The sample size was calculated using the following formula and according to Oyarzun-Gonzalez study15, with 95% confidence, and 80% power.
Two groups of 120, and a total of 240 elderly people (120 poly-pharmacy and 120 non-polypharmacy) were selected. The inclusion criteria were as following: being 60 and over, no change in dose and type of medication for at least 3 months4, no record of stroke and no moderate to severe cognitive impairment (participants must have a cognitive score more than 20 or equal) and the exclusion criteria were the unwillingness of the participants to cooperate, and the presence of delirium symptoms.
Besides stating the goals of the study, the researcher identified eligible patients and started collecting the data after obtaining a written consent and assuring them about the confidentiality of their information.
Data collection tools included demographic-medical profile questionnaire (age, gender, education, income, living arrangement, type of chronic diseases, number of chronic diseases, risk factors for cardiovascular disease [hypertension, diabetes, hyperlipidemia, smoking, overweight, and regular physical activity], the number of medications being taken, and the category of medications being taken), Geriatric Oral Health Assessment Index, Geriatric Depression Scale, Cognitive Status Test (COST), and Anatomic Therapeutic Chemical (ATC) questionnaires.
The COST designed by Babacan Yildiz (2012)22. This questionnaire has 19 questions and examines areas of orientation (4 marks), registration memory (3 marks), attention (5 marks), recall memory (3 marks), abstraction and judgment (2 marks), verbal fluency (1 score), retrograde memory (3 marks), language (5 marks), agnosia (1 score), apraxia (2 marks), and visuo-spatial functions (1 score). This questionnaire has been validated in Iran by Lotfi23. Cronbachs alpha coefficient for the whole instrument is 0.82 and its sensitivity and specificity at the cutting point (25.5) are 94% and 86%, respectively.
To evaluate the drugs used, the classification system of ATC was considered, in which drugs are classified into 13 categories. Only those medications were recorded which the patient did no change their type and dose for at least 3 months.
To analyze the data, SPSS software version 21 and Statistical tests of χ2, independent t-test, and linear and logistic regression were used. Significant level was considered < 0.05.
Results
The results showed that the proportion of women in the polypharmacy group was significantly higher than in the group without polypharmacy. Polypharmacy, in terms of education, was significantly higher in people with low education. There was no significant difference between the two groups in terms of age, marriage, living arrangement, and income (Table 1).
Table 1 Comparison of demographic characteristics among two groups with (n = 120) and without poly-pharmacy (n = 120).
| Characteristics | Polypharmacy | Non-polypharmacy | p |
|---|---|---|---|
| Age (mean ± SD) | 67.63 ± 6.67 | 66.09 ± 6.21 | 0.065 |
| Gender (n, %) | 0.007 | ||
| Female | 55 (45.8) | 34 (28.3) | |
| Male | 65 (54.2) | 86 (71.7) | |
| Marriage (n, %) | 0.500 | ||
| Single | 1 (0.8) | 1 (0.8) | |
| Married | 113 (94.2) | 117 (97.5) | |
| Widow | 6 (5) | 2 (1.7) | |
| Living with (n, %) | 0.171 | ||
| Spouse | 70 (58.3) | 67 (55.8) | |
| Children | 14 (11.7) | 6 (5) | |
| Spouse and children | 35 (29.2) | 46 (38.4) | |
| None | 1 (0.8) | 1 (0.8) | |
| Education (n, %) | 0.007 | ||
| Illiterate | 56 (46.7) | 43 (35.8) | |
| Primary | 34 (28.3) | 37 (30.8) | |
| High school | 12 (10) | 4 (3.4) | |
| Diploma and higher | 18 (15) | 36 (30) | |
| Income (n, %) | 1 | ||
| Less than expenditure | 88 (73.3) | 89 (74.2) | |
| Equal to expenditure | 30 (25) | 29 (24.2) | |
| More than expenditure | 2 (1.7) | 2 (1.7) |
Most of the drugs used in the poly pharmacy group were respectively nonsteroidal anti-inflammatory drugs (84.2%), blood lipid lowering (71.7%), angiotensin converting enzyme inhibitor (67.5%), gastrointestinal drugs (41.7%), and diabetic drugs (36.7%) (Table 2).
Table 2 Comparison of medication classification among two groups with (n = 120) and without polypharmacy (n = 120).
| Medication classification | Polypharmacy | Non-polypharmacy | p |
|---|---|---|---|
| Alimentary tractsand metabolism (n, %) | |||
| Acid related disorders | 18 (15) | 2 (1.7) | < 0.001 |
| Peptic ulcer and reflux | 32 (26.7) | 10 (8.3) | < 0.001 |
| Antispasmodics | 6 (5) | 1 (0.8) | 0.120 |
| Drugs for constipation | 0 (0) | 2 (1.7) | 0.498 |
| Diabetes | 44 (36.7) | 11 (9.2) | < 0.001 |
| Vitamins | 32 (26.7) | 9 (7.5) | < 0.001 |
| Mineral supplements | 24 (20) | 5 (4.2) | < 0.001 |
| Blood and blood forming drugs (n, %) | |||
| Antithrombotic agents | 35 (29.2) | 11 (9.2) | < 0.001 |
| Anti-anemic preparations | 9 (7.5) | 8 (6.7) | 1 |
| Cardiovascular systems (n, %) | |||
| Antiarrhythmics | 5 (4/2) | 0 (0) | 0.060 |
| Nitrates | 6 (5) | 1 (0.8) | 0.120 |
| Beta-blockers | 78 (65) | 31 (25.8) | < 0.001 |
| Calcium-blockers | 16 (13.3) | 2 (1.7) | 0.001 |
| ACE inhibitors | 81 (67.5) | 48 (40) | < 0.001 |
| diuretics | 15 (12.5) | 3 (2.5) | 0.006 |
| Lipid lowering agents | 86 (71.7) | 39 (32.5) | < 0.001 |
| Hormones (n, %) | |||
| Thyroid hormone | 8 (6.7) | 9 (7.5) | 1 |
| Musculoskeletal system (n, %) | |||
| NSAID | 101 (84.2) | 79 (65.8) | 0.002 |
| Nervous system (n, %) | |||
| Analgesics | 29 (24.2) | 5 (4.2) | < 0.001 |
| Anti-epileptics | 23 (19.2) | 4 (3.3) | < 0.001 |
| Anxiolytics | 17 (14.2) | 3 (2.5) | 0.002 |
| Anti-depressant | 23 (19.2) | 5 (4.2) | < 0.001 |
| Sedatives | 9 (7.5) | 5 (4.2) | 0.410 |
| Anti-dementia | 2 (1.7) | 1 (0.8) | 1 |
| Respiratory system (n, %) | |||
| Anticholinergic/corticosteroid | 1 (0.8) | 1 (0.8) | 1 |
| Inhalants | 6 (5) | 0 (0) | 0.029 |
| Cough suppressants | 5 (4.2) | 1 (0.8) | 0.213 |
| Antihistamines | 4 (3.3) | 1 (0.8) | 0.370 |
| Bronchodilators |
Performance under the domains of orientation, registration memory, attention, recall memory, retrograde memory, ability to recognize objects, and spatial-visual function in the poly pharmacy group was significantly lower than the non-polypharmacy group (Table 3).
Table 3 Relationship between polypharmacy and cognition subdomains.
| Group | Polypharmacy | Non-polypharmacy | Z | p |
|---|---|---|---|---|
| Cognition subdomains | (Mean ± SD) | (Mean ± SD) | ||
| Orientation | 3.23 ± 0.719 | 3.88 ± 0.357 | -7.967 | < 0.001 |
| Registration memory | 2.65 ± 0.603 | 2.98 ± 0.129 | -5.784 | < 0.001 |
| Attention | 3.43 ± 1.186 | 4.54 ± 0.697 | -7.32 | < 0.001 |
| Recall memory | 2.01 ± 0.921 | 2.79 ± 0.533 | -7.664 | < 0.001 |
| Abstraction and judgment | 1.78 ± 0.488 | 1.90 ± 0.353 | -2.01 | 0.044 |
| Verbal fluency | 0.96 ± 0.201 | 0.99 ± 0.091 | -1.65 | 0.099 |
| Retrograde memory | 2.15 ± 0.904 | 2.88 ± 0.393 | -7.463 | < 0.001 |
| language | 4.93 ± 0.310 | 0.203 ± 4.98 | -1.429 | 0.153 |
| Agnosia | 0.91 ± 0.290 | 0 ± 1 | -3.388 | 0.01 |
| Apraxia | 1.98 ± 0.377 | 0 ± 2 | -1.65 | 0.29 |
| Visuo-spatial functions | 0.77 ± 0.425 | 0.250 ± 0.93 | -3.608 | < 0.001 |
All of the variables that had a significant relationship, along with the variables which had p < 0.3 (age, gender, living arrangement, education, income, diabetes, hypertension, hyperlipidemia, smoking, physical activity, CHF, and oral health, depression) were included in the regression model. Regression analysis demonstrated that most predictors of the cognitive status of the elderly referring to the cardiac clinic were poly pharmacy, income, hypertension, and gender, respectively. About 48.9% of the variance of the change in cognitive score was determined using this model (adjusted R square = 0.489) (Table 4).
Discussion
The results of the present study showed that there is no significant difference between the age of the elderly with or without poly pharmacy. In the study of Hosseini, Delshad and Dianati, the relationship between age and polypharmacy was not considerable16,18,19. But in Al Amins study, the relationship between age and polypharmacy was significant6. With aging, the rate of poly pharmacy increased, and the highest dose of the drug was related to the age group of between 51 and 60 years old. The reason could be related to two different age groups of patients in their studies and the present study.
The findings indicated that poly pharmacy was remarkably higher in women and people with low education, but was not significantly associated with income. These findings are consistent with the results of the Dianati18 study in terms of gender and income. But in Dianatis study, the relationship between education and poly pharmacy was not significant. Women, due to having higher life expectancy, may have higher levels of polypharmacy. Women also seem to be more concerned about their health than men and therefore refer to a physician. However, in the study of AL-Amin6, there was no significant difference between the mean of the drugs used by men and women. In a Cohort study of 349,689 elderly people in Italy, poly pharmacy was higher in men24,25. In the above study, the incidence of chronic diseases was higher in men. The findings of a study of 626,258 elderly people aged 75-89 in Sweden showed that the odds ratio (OR) of poly pharmacy in people with low education after eliminating the effects of age, gender, place of residence, and chronic diseases is 1.11 times higher than highly educated people (95% CI: 1.1-1.12)26. Health-care staff, especially nurses, can play an important role in warning against the consequences of unnecessary drug use to people with low education.
The results of the present study showed that most of the drugs being used were non-steroidal anti-inflammatory drugs (84.2%), lipid lowering agents (71.7%), angiotensin converting enzyme inhibitor (67.5%), and gastrointestinal drugs (41.7%), and diabetic drugs (36.7%), respectively. In Delshads study19, the most widely used drugs were aspirin (30.4%), atenolol (28.7%), and ranitidine (24%). In the study of Slabaugh (2010) on 349,689 elderly people in Italy, the most commonly prescribed drugs, were anticoagulants, gastric ulcer and antireflux drugs, and angiotensin inhibitors25. In Haiders study27 on 621 elderly people in Sweden, anticoagulants (42.5%), p- blocking (anti neuroinflammation) (28.3%), and loop diuretics (28%) were the most prevalent drugs.
The research findings showed that the cognitive score in the poly-pharmacy group was significantly lower than the non-polypharmacy group. The OR of cognitive impairment in the poly-pharmacy group was 3.17 times more than that of the non-poly-pharmacy group (95% CI: 2.48-4.05). The findings are consistent with the results of other authors9-17.
According to Moon10, 2392 people aged 70-84 years were examined, of which 26.8% used more than five drugs and 4.1% more than ten drugs. Cognitive status was assessed using “word list recall test,” “Trail Making Test,” and “Korean version of the Frontal Assessment Battery.” The results showed that both poly-pharmacy (taking five drugs and more) and hyper-polypharmacy (taking ten drugs and more) had a significant relationship with cognitive impairment. The study included both prescription and over-the-counter medications for polypharmacy. After the elimination of confounding factors, including the severity of chronic diseases, cognitive impairment was significantly associated only with those polypharmacy which were related to physician-prescribed drugs. In the study of Khezrian11, 496 people, aged between 63 to 68 years old, who did not have dementia were examined. A complete neuropsychological and physical examination of the participants was performed. Cognitive status was assessed using different test such as “Auditory Verbal Learning Test,” “Digit Symbol Score,” “Block Design Score,” and “Spatial Ability Measurement.” After eliminating the confounding factors including chronic diseases, age, gender, education, and body mass index, poly-pharmacy (taking five drugs and more) was significantly associated with cognitive impairment.
In a study of 7.422 people over the age of 65 in Taiwan, Cheng, et al.12 examined the relationship between polypharmacy and mild cognitive impairment. Demographic and medical information, as well as habits and lifestyles, were collected through interviews. To assess the cognitive status, the Taiwanese version of the Mini Mental Status Examination (TMMSE) and the Clinical Dementia Rating (CDR) were used. The results showed that after eliminating the effects of age, gender, body mass index, education, chronic diseases, habits, and lifestyle, poly-pharmacy (taking five drugs and more) increased the chance of mild cognitive impairment by 1.75 times (p = 0.001). In addition, the adverse effects of polypharmacy on cognitive capacity were evident even in individuals without vascular disorders.
In Niikawa study13, a questionnaire containing demographic characteristics was sent to all elderly people over the age of 65 in Tokyo. Then 3.000 people were randomly selected from the study participants. Elderly people were interviewed at their homes. Of the 1.270 people who completed the interview, 1.152 were analyzed. Cognitive status was assessed using a “Mini Mental Status Exam.” The results showed that poly-pharmacy was present in 48.3% of people who had a cognitive score below 24 and 25.7% of people who had a cognition score above 24 (p < 0.001). After the elimination of the confounding factors, the relationship between polypharmacy and cognitive impairment was significant (OR: 1.83; 95% CI: 1.1-3.02; p = 0.019).
On the other hand, In Langeard study9, 113 people over the age of 55 who had a record of falls, with or without injuries in the past year, were examined through some tests, including the “Time-Up and Go.” The tool for studying cognitive status was the Montreal Cognitive Assessment. The findings show that taking five different drugs or more is associated with an increased risk of motor impairment as well as general cognitive impairment. Researchers have suggested that both the health-care team and patients should be more cautious about taking multiple medications simultaneously, especially when a patient is being treated by several therapists or multiple prescriptions.
In the study of Hosseini16, which was performed on 1616 elderly people over 60 years of age living in Amirkola, Babol community, drug information was collected through interview. The average age of the participants was 69.37 years and 54.6% of them were men. The OR of polypharmacy was 1.51 times higher in women than that in men (95% CI: 1.1-1.93). Most of the drugs used in both genders were cardiovascular drugs. Cognitive status was assessed using a Mini Mental Status Examination Test. The results showed that there was no significant relationship between poly-pharmacy (taking five drugs and more) and cognitive impairment.
A study by Oyarzun Gonzalez15 looked at data from 572 seniors surveyed in New Mexico, the Mini-Mental status Examination test was used to examine cognitive impairment, and Multivariate linear regression was used for statistical analysis. Most of the participants (63.6%) were women and married (88.5%). The education level of most of them (83%) was diploma or higher. The findings showed that after eliminating the effect of age, gender, severity of chronic diseases (Charlson index), APOE4 gene, body mass index, and hypertension, the relationship between poly-pharmacy (consumption of five different drugs and more) and mild cognitive impairment was not significant (p = 0.23). Although this relationship was not significant, poly-pharmacy was associated with a decrease of 0.11 ± 0.99 in cognitive score.
Worth17 looked at data from 13869 elderly people over the age of 65 who were interviewed at home in the National Survey of Nutrition and Health between 1988 and 2010. In the above study, the drugs which were used last month were the criteria and the over-the-counter drugs were not considered. No screening tools were used to assess the state of cognition, and only troubles in remembering, or experience periods of confusion were questioned. The rate of polypharmacy (five drugs or more) tripled in the above years. These increases were mainly related to cardio-protective and antidepressant medications. Although the increase in the number of drugs was associated with decreased performance, limited daily life activities, and memory problems, it was not significant after eliminating the confounding factors.
The Gnjidic study14 was conducted on 1705 men aged 70 and over, living in the community, who had participated in a health and aging project. In the above study, in addition to the status of cognition, several other consequences were also studied. Cognitive status was assessed using the “Mini-Mental Status Examination Test” and the “Informant Questionnaire on Cognitive Decline,” and approved by two geriatricians, a neurologist and a neuropsychologist. Drug status was interviewed over the past month (both prescription and over-the-counter). For each increase in the number of medications, the adjusted OR were 1.13 (95% CI: 1.06-1.21) for frailty, 1.08 (95% CI: 1.1-1.15) for disability; 1.09 (95% CI: 1.04-1.15) for mortality, and 1.07 (95% CI: 1.03-1.12) for falls. However, there was no relationship between increasing the number of medications and cognitive impairment.
Various factors may contribute to the inconsistency of the findings of the present study with the above studies14-17, such as the different demographic characteristics of the participants in the study (age, gender, education, and income) or clinical characteristics (chronic diseases and the complexity of the medication regimen) or psychosocial characteristics (symptoms of anxiety and depression, and social support), study design and cognitive status assessment tools, or different inclusion and exclusion criteria (e.g., in the present study and the use of drug for at least 3 months was the criterion).
Conclusion
In general, based on the results of this study, poly-pharmacy increases the chances of developing cognitive impairment. The relationship between polypharmacy and some areas of cognition, such as speech fluency, language, and the ability to perform purposeful movements, was not significant. Most predictors of cognitive status were polypharmacy, income, blood pressure, and gender, respectively. Therefore, further studies and appropriate interventions are recommended.
One of the limitations of the research was that most of the participants in the study were illiterate and had trouble understanding some of the concepts and questions of the tools. Therefore, it was attempted to ask the questions in a simple and understandable language, and if there was any ambiguity in their answers, the researcher would ask for more explanations to clarify the matter. Another limitation was fatigue during the interview due to old age of the participants. The solution for filling out the questionnaires, therefore, was to pause and give a break between interviews.