Introduction
Infective endocarditis is associated with a high mortality rate of 15-20% and a 1-year mortality approaching 40%1. Embolism is a major life-threatening complication of endocarditis and often involves major arterial beds, including the lungs, coronary arteries, spleen, bowel, and extremities. Up to 65% of embolic events may involve the central nervous system1,2. Multiple embolic events are rarely encountered, and no previously reported cases have addressed infective endocarditis complicated with iliac saddle and cerebral embolisms.
Case
A 48-year-old man presented at our internal medicine clinic with the complaints of fever, fatigue, and loss of weight and appetite and was transferred to cardiology clinic for an audible cardiac murmur. His medical history was unremarkable, except for hypertension. A physical examination revealed a blood pressure of 140/80 mmHg, pulse rate of 110 beats/min, and body temperature of 38.3°C. He had mild scleral icterus and hepatomegaly. Cardiac auscultation revealed a harsh systolic murmur at the mitral valve area. A transthoracic echocardiogram showed a vegetation (0.9 × 0.3 cm) attached to the anterior fibrotic mitral leaflet (Fig. 1A). No other valves were involved. Laboratory tests showed leukocytosis, an elevated C-reactive protein level of 120 (1-5) mg/dl, and an erythrocyte sedimentation rate of 63 (20-40) mm/h. Urine analysis revealed microscopic hematuria, but a chest radiograph did not reveal any abnormal findings. Three sets of blood culture samples were taken, and empirical antibiotic therapy with vancomycin (40 mg/kg 2 × 1 i.v.) and gentamicin (3 mg/kg 1 × 1 i.v.) was initiated with a diagnosis of native valve endocarditis. Three days after hospitalization, the patient suddenly developed dysphasia, and a brain magnetic resonance imaging revealed multiple embolic infarcts located at the right cerebral hemisphere and the left occipital, parietal, and temporal lobes. On day 5, the patient complained numbness and pain in his lower extremities, and a duplex ultrasonography revealed a saddle embolism at the iliac bifurcation (Fig. 1B).

Figure 1 A: transthoracic echocardiography showing the vegetation (arrow). B: ultrasonographic image of the iliac saddle emboli (arrow). C: the resected embolized material. LA: left atrium. LV: left ventricle.
The patient underwent an urgent operation. A bilateral femoral artery incision was made and the embolized material was resected by a bilateral femoral embolectomy (Fig. 1C). All surgical instruments were changed and a median sternotomy was performed. The fibrotic mitral valve was replaced with a 29 mm bioprosthetic valve after debridement of vegetations (Fig. 2A). The patient tolerated the surgery well.
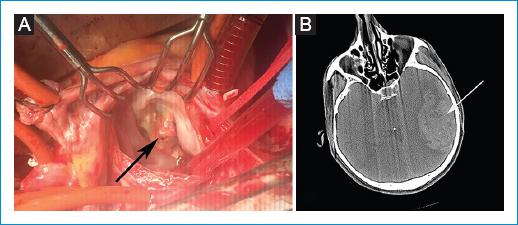
Figure 2 A: intraoperative image showing the vegetation (arrow). B: computed tomographic image showing intracerebral hemorrhage (arrow).
Blood cultures were positive for coagulase-negative Staphylococcus aureus. The patient was started on 1 mg/kg low-molecular-weight heparin after post-operative bleeding control and then on aspirin at post-operative day 10. A 6-week course of intravenous antibiotic treatment (daptomycin 10 mg/kg 1 × 1 i.v. and cloxacillin 2 g/4 h i.v.) was scheduled and continued according to the antibiogram. However, during the hospital stay, the patient developed an intracerebral hemorrhage (Fig. 2B). He underwent an operation in the neurosurgery clinic but, unfortunately, he died 5 days later.
Discussion
Despite diagnostic and therapeutic improvements, infective endocarditis remains associated with a high morbidity and mortality. Up to 90% of patients with infective endocarditis present with fever, often associated with systemic symptoms of chills, poor appetite, and weight loss1. Peripheral septic embolisms are an extremely prevalent phenomenon in infective endocarditis, being present in approximately 45-65% of the cases studied on autopsy. In contrast to posterior leaflet locations, vegetations located at the anterior mitral leaflet are more prone to peripheral embolism, as in the present case. Embolism is also more likely when the vegetations are large (more than 10 mm in length) and highly mobile1,2.
In infective endocarditis, a peripheral septic embolism typically cannot be identified because of the lack of a high index of suspicion2. In our patient, the symptoms and signs were initially attributed to a gastrointestinal malignancy, probably since the patient had no history of previous heart disease. Likewise, weight loss may be the initial clinical presentation of infective endocarditis and should be part of the differential diagnosis in patients who have weight loss of relatively sudden onset and a history of fever and fatigue. The diagnosis of infective endocarditis should not be excluded based on a clinical examination alone. Microbiological analysis and echocardiography are essential for diagnosis. Contrary to popular medical practice, bacteremia in infective endocarditis is continuous, so cultures do not need to be timed with peaks of fever3.
Infective endocarditis is complicated by stroke in 20-40% of cases4. Although the current guidelines recommend surgery to prevent recurrent embolus in patients with a persisting vegetation higher than 10 mm in size, this recommendation is mostly not considered alone in clinical practice. Mitral valve involvement with severe valvular regurgitation or stenosis, vegetation mobility, and S. aureus infection is the other risk factors for embolism2,4,5.
In cases with a high suspicion of infective endocarditis, empirical antibiotic treatment must be started at the earliest time possible, because delays have negative impacts on clinical outcomes. The early initiation of antimicrobial therapy (within 1 week) is associated with a 65% reduction in risk of stroke related to infective endocarditis5.
On the other hand, in a cohort of 1345 patients with infective endocarditis, S. aureus infection and anticoagulant therapy were significantly associated with a larger number of hemorrhagic strokes from hemorrhagic transformations of ischemic lesions even after 1 week of antimicrobial treatment6.
In cases of neurological complications, when cerebral hemorrhage has been excluded and neurological damage is not severe, cardiac surgery can be performed early. Conversely, in cases with large intracranial hemorrhage, the neurological prognosis is poor and surgery must be delayed for at least 1 month. However, if urgent cardiac surgery is needed, close cooperation with the neurosurgical team is essential. After an ischemic stroke, cardiac surgery is not contraindicated unless the neurological prognosis is judged as too poor2,5,7. However, note that surgery can lead to hemorrhagic transformation of ischemic stroke caused by the anticoagulation theraphy used for cardiopulmonary bypass.
The risk of neurological deterioration after valvular surgery has been reported to be low (0-6%), even when surgery is performed very early after the first appearance of neurological symptoms4,7. It has been previously shown that no apparent survival benefit was found in delaying surgery when indicated in infective endocarditis patients after ischemic stroke5,7.
Conclusion
Stroke and peripheral embolism remain one of the most common and often devastating complications of infective endocarditis. Although the clinical heterogeneity of infective endocarditis sometimes prevents early diagnosis and timely treatment, patients who present with fever and with non-specific symptoms such as loss of appetite and weight, as in the present case, should be evaluated for the presence of infective endocarditis.














