Clinical case
A 40-year-old female arrives at the emergency room presenting with palpitations and chest discomfort for the past 12 h; medical history of Ebstein malformation and 4 tricuspid valve surgical replacements, all due to thrombotic deterioration, especially fast with mechanical prosthesis. Last surgery was 15 years ago, using a biological Labcor # 25 prosthesis.
The patient reported a baseline functional status New Your Heart Association I, without additional symptoms; at physical examination, heart rate was 129 bpm, respiratory rate 18 bpm, blood pressure 109/67 mmHg, oxygen saturation 98%, no jugular vein distention, or lower extremity edema were present. Electrocardiogram showed atrial fibrillation with rapid ventricular response after treatment with intravenous (IV) metoprolol, lead to clinical deterioration, and immediate admission to the intensive care unit for IV amiodarone infusion for rhythm control, but pharmacological rhythm control strategy failed, finally requiring electrical cardioversion.
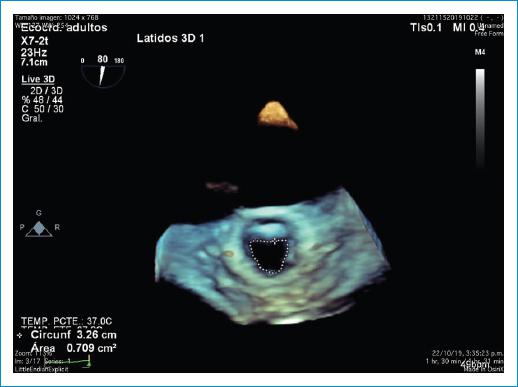
Transthoracic and transesophageal echocardiogram showed severe right atrial enlargement of 54 cm2, small right ventricle along with low tricuspid annular plane systolic excursion (Tricuspid annular systolic displacement 0.6) of biological prosthesis that presented signs of dysfunction: limited movement of the valves, annular sclerosis, diastolic turbulent flux, peak gradient 17 mmHg, mean gradient 5 mmHg, pressure half-time 113 ms and area 0.79 cm2 (Fig. 1), with mild-moderate central insufficiency (vena contracta 3.9), small paravalvular leak (vena contracta 2 mm), with no relevant morphological or functional alteration in the rest of the cardiac structures, and an LVEF of 60%.
The patient had no other relevant symptoms or signs, and complementary laboratories of renal, hematological, endocrine, and liver function were normal, and inflammatory markers were not elevated. Cardiac computed tomography scan imaging showed atrium enlargement and biological prosthesis in tricuspid position with criteria of dysfunctionality: diameter of the prosthetic ring calculated at 33 mm with an average valve diameter of 21.6 mm and 19.4 mm internal diameter with limited opening of the valves: area of 1.1 cm2 and a paravalvular leak.
The heart team evaluated the case discarding surgical options due to the multiple previous interventions resulting in severe chest adhesions that increased the surgical risk to a level that exceeded its benefit, so endovascular valve in valve implant with annular cracking was considered the only option for the failed stenotic valve.
Given the limited commercial availability of devices for this procedure, it was necessary the approval of compassionate off label use of mitral Edwards, and as no specific sized rigid balloons were commercially available a kissing balloon technique, usually used in coronary interventions which were proposed for the annular cracking.
As soon as the patient was stabilized, with ventricular rhythm controlled, the valve in valve procedure was performed through right femoral vein, the kissing balloon technique was used with two 14 × 20 mm ultra-non-compliant balloons under pacemaker arrest (Fig. 2) and transesophageal echocardiographic monitoring, successful rupture of the biological prosthesis ring was achieved, which allowed the successful placement of the Edwards XT # 26 implant, with a residual peak gradient of 3 mmHg and mean 1 mmHg without valvular or paravalvular insufficiency evaluated with echo-TE intraprocedural monitoring (Fig. 3).
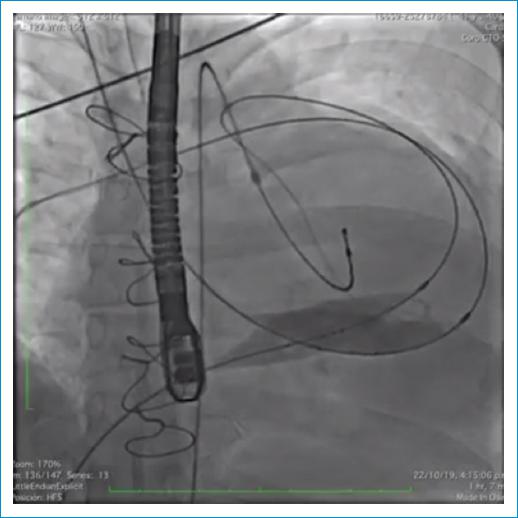
Figure 2 Angiographic image of kissing balloon technique using two 14 × 20 mm ultra-non-compliant balloons with successful annular cracking.
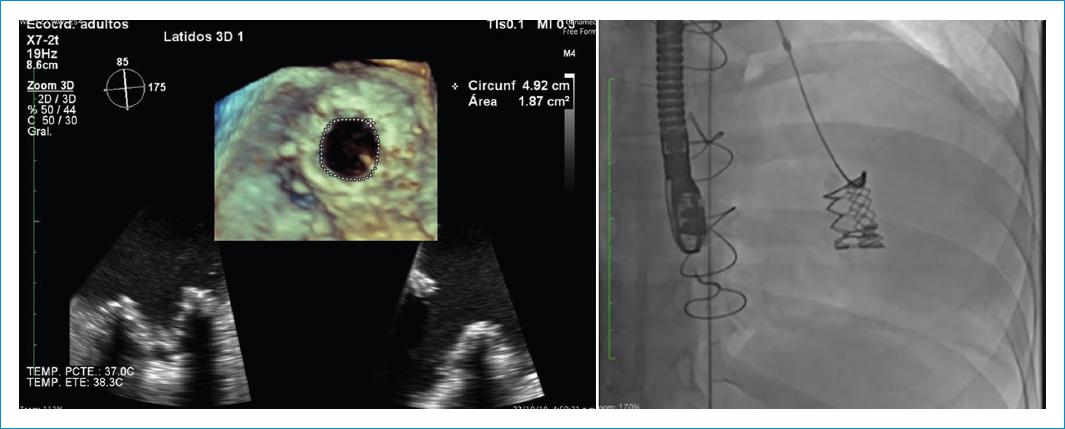
Figure 3 Final result: echocardiography and angiography image of percutaneous implant with new effective area of 1.87cm2.
The patient was considered at high risk of implant thrombosis; therefore, anti-aggregation therapy with clopidogrel during 3 months, along with permanent formal anticoagulation with warfarin, was set to achieve INR between 2 and 3 to preserve valvular integrity.
Soon after discharge, the patient was back to sinus rhythm, during a year of follow-up, the patient remained asymptomatic, with variable INR within 1.7-4 that required regular controls, echo at 1 year showed an implant with no signs of thrombosis, which preserved measures of functionality: peak gradient 6 mmHg, mean gradient 3 mmHg, and peak velocity 121 cm/s.
Discussion
Ebsteins anomaly is a rare malformation of the tricuspid valve and the right heart, with an incidence of approximately 1 in 20,000 newborns, in which tricuspid valve repair is the goal of operative intervention1. The surgical treatment of the patient at an early age with the use of mechanical prosthesis had stabilized her condition in terms of the right ventricle enlargement, myocardial dysfunction, and tricuspid valve regurgitation, but lead to numerous thrombotic complications with the resulting need of multiple interventions that ended up in a hostile inoperable chest and an early need for valve replacement due to valve deterioration, as an inevitable complication of tricuspid implants that have shown a durability of approximately 10 years, except in patients below 16 years of age, who present dysfunction within 5 years2.
Tricuspid endovascular valve in valve has been proposed as an alternative for patients with degenerated bioprosthesis who cannot go under surgery for any reason3, evidence from countries where this endovascular intervention has been taking place is promising is considered safe and effective4,5 depending on many factors, mainly, the pre-operative clinical status of the patient, influenced by age, anatomical conditions, and the degree of myopathy worsened by conditions such as chronic arrhythmias and ischemic disease. In addition, there are relevant technical factors, in this case, the limited commercial offers of tricuspid specific endovascular implants for valve in valve procedures, lead to the implant of a mitral prosthesis as an off-label indication supported as compassionate use given the mortal prognosis within the impossible surgical circumstance, and the completely functional patient condition at a considerable young age based on the previous successful reports6,7.
The main mechanism of prosthesis dysfunction is regurgitation, but in some cases, like this one, annular and leaflet fibrosis deteriorate the functionality of the prosthesis, the classical approach requires cracking of the prosthetic annulus to place an implant avoiding greater stenosis. The relevance of this case for the national endovascular practice is the overcome of the commercial limitations by the using the classical kissing balloon technique for coronary interventions, and occasionally used for valvular annular fracture with good results8,9.
Conclusion
Percutaneous off-label tricuspid valve in valve with a mitral prosthesis through venous femoral access using the kissing balloon technique resulted in a life-saving procedure for the patient. The off-label use of devices and adaptation of techniques is still a controversial topic, endovascular therapies are advancing way faster than agencies that can regulate and commercial distribution can cover, but patients still need solutions and off-label responsible, informed and evidence-supported use is part of the integral actual practice. This case aims to give practical technical adaptation of the literature for the Colombian experts within the commercial context for well-chosen, planned, and executed cases performed by highly qualified professionals.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.