Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
CES Medicina
versão impressa ISSN 0120-8705
CES Med. v.23 n.1 Medellín jan./jun. 2009
ARTÍCULOS DE INVESTIGACIÓN CIENTÍFICA O TECNOLÓGICA
General versus regional anesthesia for ambulatory arthroscopic knee surgery
Anestesia general versus regional para cirugía artroscópica ambulatoria de rodilla
MARÍA PATRICIA GONZÁLEZ O1, MARÍA ISABEL VÁSQUEZ S1, LUIS ANDRÉS HERRERA-MORALES1, ROBERTO CARLO RIVERA D1, MARIO ANDRÉS ARCILA L1, JUAN JOSÉ PUERTA M1, LIZA MARGOTH TRUJILLO H1, YOLANDA TORRES DE G2
1 Anesthesiologist Clinica CES. Anesthesiology Faculty Universidad CES, Medellin, Colombia.
2 Clinical Epidemiologist & Public Health Faculty Universidad CES, Medellin, Colombia. Grupo Observatorio de la Salud Pública Corresponding author: mariapgonzalez@hotmail.com
ABSTRACT
Background Arthroscopic surgical procedures on the knee are now frequently performed and there is still no agreement as to what is the best anesthesia technique for them. Any anesthetic technique used should bring fast and safe recovery, accompanied by good postoperative pain control and good patient satisfaction, all very important goals of ambulatory anesthesia.
Objective: The goal of the study was to compare general versus regional anesthesia (sciatic, femoral and obturator nerve blocks) in terms of pain control, time to discharge and overall patient satisfaction among others.
Methods: We conducted a randomized, non-blinded, clinical essay. The sample included all patients scheduled for arthroscopic knee surgery at Clinica CES that met inclusion criteria, during the period of time that the study was performed.
Results: There were no significant differences in demographic characteristics, or intraoperative time between groups. Time spent in post anesthesia care unit was significantly lower in the group where regional anesthesia was used (15 vs. 78 minutes, p<0.05). Patients in the regional anesthesia group also did not require supplemental analgesia and were discharged earlier. In fact, all the patients in regional anesthesia group had VAS Pain Scores less than 3 one hour after surgery, while 56 % of the patients in the general anesthesia group had pain scores above 5 and required supplemental analgesia. There were higher incidence of postoperative nausea and vomit and greater anesthesia-related costs in general anesthesia group. Regional anesthesia patients were more satisfied with the anesthetic technique used than the general anesthesia ones.
Conclusion: The results of this study suggest that regional anesthesia for ambulatory arthroscopy knee surgery provides better postoperative analgesia, earlier discharge and better patient satisfaction than general anesthesia. Regional anesthesia also seems to facilitate early rehabilitation and could provide good care at lower cost.
KEY WORDS
Arthroscopy, Nerve block, General anesthesia, Anesthesia recovery period, Patient satisfaction.
RESUMEN
Introducción: La cirugía artroscópica de rodilla realizada ambulatoriamente impone el reto de encontrar la técnica anestésica más adecuada para este tipo de procedimiento. La técnica usada debe conllevar a una rápida y segura recuperación, brindar buen control del dolor en el postoperatorio e incrementar la satisfacción del paciente.
Objetivo: Comparar la anestesia general versus anestesia regional (bloqueo de nervio periférico de los nervios ciático [abordaje posterior], femoral y obturador) en cirugía artroscópica de rodilla en términos de control del dolor, tiempo para el alta hospitalaria y satisfacción general del paciente, entre otros.
Métodos: Realizamos un estudio clínico, aleatorizado no cegado. La muestra incluyó todos los pacientes con cirugía artroscópica de rodilla ambulatoria efectuadas en la Clínica CES durante 2005.
Resultados: No hubo diferencia estadísticamente significativa en las características demográficas, ni en el tiempo intraoperatorio entre los grupos. El tiempo de estancia promedio en la unidad de cuidados postanestésicos fue significativamente menor en el grupo de anestesia regional (15 vs 78 min, p<0.05). El grupo de anestesia regional no requirió ningún suplemento analgésico. Todos los pacientes de este grupo tuvieron puntajes de dolor VAS menor a 3 una hora después de cirugía, mientras que el 56 % de los pacientes en el grupo de anestesia general tuvo puntajes de dolor VAS mayores de 5 y requirieron suplemento analgésico. En forma significativa, el grupo de anestesia regional manifestó un mayor grado de satisfacción con la técnica anestésica empleada, que el grupo de anestesia general. Hubo una mayor incidencia de nauseas y vómito postoperatorio y un costo anestésico más elevado en el grupo de anestesia general, pero dado el tamaño de la muestra, la diferencia no fue estadísticamente significativa para estas variables.
Conclusión: Los resultados sugieren que la anestesia regional para cirugía artroscópica de rodilla provee mejor analgesia postoperatoria, un alta hospitalaria más temprana, y un mayor grado de satisfacción del paciente que la anestesia general. La anestesia regional también parece facilitar la rehabilitación temprana y podría proveer buen cuidado a un menor costo.
PALABRAS CLAVES
Artroscopia, Bloqueo de nervio periférico, Anestesia general, Periodo de recuperación anestésico, Satisfacción del paciente
INTRODUCTION
Ambulatory anesthesia history began with anesthesia history itself. In the 1840's, first anesthesia experiments were made using outpatient management. After this beginning ambulatory management became infrequent, few articles were published about it and medical community attention focused on intrahospitalary management of post surgery period (1).
It was not until 1959 that a paper denoting interest in ambulatory anesthesia was published; Webb and Graves described their experience in ambulatory patient management during a 10 year period (2). Following this article, use of ambulatory anesthesia and surgery has grown constantly along publications related to it. This has been more obvious since 1980's. In 1959 approximately 5 % of anesthesia patients were managed ambulatorily (2). During 1980 outpatient surgery represented 16 % of surgical procedures in the United States, in 1990 it represented 50 %, and by the year 2000, it had grown to represent 60 % of all surgical practice. The main factor influencing this growing tendency appears to be economic aspects (3). On the other hand aspects directly related with patient management, such as postoperative nausea and vomiting (PONV) incidence (4-6), and adequate pain management (7,8), have been the main variables influencing anesthetic technique choice.
In patients undergoing ambulatory surgery endpoints like postoperative pain, PONV, and early rehabilitation, are considered as the most important factors to evaluate (9,10). Nevertheless economic issues, intraoperative time (defined as surgical time plus anesthetic time), postanesthetic care unit (PACU) time and readmission rate have been studied as well. Patient and surgical team satisfaction are considered a result of previous factors combination (11).
In the last decade medical community has reinforced its interest in further development of ambulatory surgery and related anesthetic techniques. Now it looks obvious that ambulatory management of certain pathologies does not jeopardize patient welfare, increases patient and relatives' satisfaction due to earlier discharge and rehabilitation begin (12) and decreases medical attention associated cost. Being this a paramount goal for healthcare system.
Beside the wider use of minimally invasive surgery that allow procedures performance in less traumatic and faster way (like laparoscopy and arthroscopy), surges the anesthetic challenge of finding out the most appropriate technique that facilitates taking advantage of this surgical advances (13,14).
Clinica CES Anesthesiology division attends all types of patients for different surgical procedures. Among them there are arthroscopic knee surgery (AKS) procedures. During the whole 2004 year, there was 266 AKS and most of them were managed ambulatorily. This reality created the necessity of evaluation and comparison of anesthetic techniques commonly used at Clinica CES, using evidencebased medicine parameters.
METHODS
Hypothesis: Combination of sciatic nerve (posterior approach) plus femoral and obturator peripheral nerve blocks (PNB), in comparison to a general anesthesia (GA) protocol for AKS, results in better postoperative analgesia, earlier discharge, lower PONV incidence and good patient satisfaction.
Type of study: This is a non-blinded prospective randomized controlled trial. Sample size was calculated according to information published on several other studies in these topics, being the most related, given the objectives, the one by Hadzic et al (15). In this study they found that under their study conditions, the combination of lumbar plexus and sciatic blocks with 2-chloroprocaine 3 % was associated with a superior recovery profile compared with GA in patients having outpatient AKS. The difference of proportions of the variables evaluated in these studies was taken in a 1 to1 ratio for each group, according to the calculations on Epi info 6.0®, based on the JL. Fleiss formula (16). According to this calculation, for a power of 80 %, and a confidence level of 95 %, a minimum number of 40 patients was required, 20 in each group. Hoping to increase the study's power, 50 patients were included. For aleatorization purposes a randomized numbers table, provided by Epi info 6.0® was obtained.
Inclusion criteria: Patient scheduled for AKS, surgical procedures lasting more than 30 min, patient age: 17 to 62 years, ASA class I or II scheduled to outpatient procedures, patient treated according to the assigned protocol exclusively, patient who did not meet these criteria were excluded.
Anesthetic technique protocols: Patients assigned to regional anesthesia (RA) group were considered as experimental group, conversely those assigned to GA were referred as the control group. Both groups share: preanesthetic evaluation and received information about both anesthetic techniques, patient's agreement to participate in the study, and sign of informed consent. Patients were admitted to the preoperative room, 1 hour before surgery, and then they received Midazolam 7.5mg orally, a peripheral venous access was granted. Later they were assigned to a subgroup according to the random table.
General anesthesia protocol (Control group)
Basic ASA monitoring was used. Preoxygenation: 5 lt/min 100 % Oxygen during 3 min. Anesthetic induction: Dexametasone 8mg IV, Fentanyl 1-2mg/ kg intravenous (IV), Lidocaine 1-2mg/kg IV, Propofol 1-2mg/kg IV, Rocuronium 10mg IV. Airway management: Laryngeal airway mask # 3, 4 or 5. Anesthetic Maintenance: Isoflurane 1-2 MAC, Oxygen 100 % at 1 lt/min flow. Mechanical or spontaneous ventilation according to patient tolerance to ventilator. Intraoperative analgesia (17): Sodium Metamizol 30 - 50mg / kg IV. Diclofenac 75mg IV.
RA protocol (Experimental group)
Basic ASA monitoring was used. Sedation before PNB: Fentanyl 50-100mg IV and Midazolam 1-3mg IV. Oxygen by nasal cannula at 2lt/min.
Block technique: Sciatic nerve block, posterior approach: Patient position: Lateral decubitus with a slight forward tilt. Block technique: Sciatic nerve block with posterior approach, as described by Hadzic A et al (18). With aseptic technique a Stimuplex® # 100 needle was introduced at an angle perpendicular to the spherical skin plane, connected to a peripheral nerve stimulator (BRAUN Dig) that was initially set to deliver 1.0mA current (2Hz, 100 μsec) until visible or palpable twitches of the hamstrings, calf muscles, foot or toes was detected. After negative aspiration for blood 10 ml of Lidocaine 2 % plus 10 ml Levobupivacaine 0.75 % both without Epinephrine were injected.
Femoral nerve block: Patient position: Supine with ipsilateral extremity abducted 10-20 degrees. Block technique: Femoral nerve block, as described by Singelyn FJ (19). With aseptic technique the same Stimuplex® #100 needle connected to a nerve stimulator (BRAUN Dig) set a current intensity of 1.0mA, 0.2msec, 2Hz, was introduced in the inguinal area and advanced through the fascia lata until quadriceps muscle contractions (i.e. patellar twitch) were obtained. After a negative aspiration test for blood 10 ml of Lidocaine 1 % with Epinephrine plus 10 ml Levobupivacaine 0.75 % without Epinephrine were injected.
Obturator nerve block: Patient position: Supine, with the knee flexed and hip abduction. Block technique: Femoral nerve block, as described by Bouaziz H (20). With aseptic technique the same Stimuplex® #100 needle was advanced, connected to a peripheral nerve stimulator (BRAUN Dig) set a current intensity of 1.0mA, 0.2msec, 2Hz, until adduction of the leg was detected, then 5 ml of Lidocaine 1 % with Epinephrine plus 5 ml Levobupivacaine 0.75 % without Epinephrine were injected.
Intraoperative sedation: Fentanyl: Titration of dose up to 150mg, Midazolam: Titration of dose up to 3mg. Intraoperative analgesia: Sodium Metamizol 30-50mg/kg IV, Diclofenac 75mg IV.
Pain Evaluation: After surgical procedure patients were evaluated for complications, and pain. Pain was assessed with the Visual Analogue Scale (VAS) (21); this evaluation was performed immediately after procedure was finished (0 min post surgery), 5, 10, 15, 30, 60 min; and 24 hours after (Phone call).
RESULTS
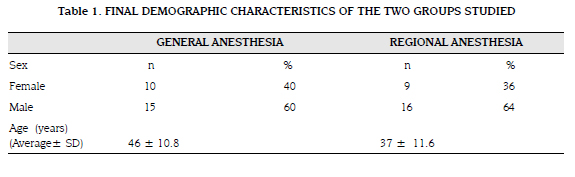
Fifty patients were included (25 patients each received RA or GA) and successfully completed the study; there were no failed blocks or breaches in protocols. There were no differences with statistic significance (p=0.770) between the 2 groups in demographic characteristics, ASA status, and types of surgical procedures performed (table 1).
Intraoperative average time in experimental group was 75 min ± 48.8 min, and in control group average time was 94 ± 46.54 min. This difference between average times had statistic significance, p< 0.000000. PACU average time in RA group was 15 ± 16.18 min. In control group PACU average time was 74 ± 47.7 min (p<0. 000000).
Postoperatory pain
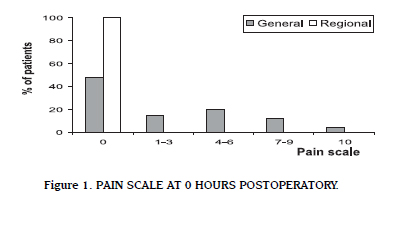
When VAS for pain was evaluated on experimental group at 0 hours postoperative, a value of 0 was found in the whole group. In control group, 48 % of patients had a value of 0, only 4 % had a maximum value of 10, the average value was 1 (SD: 3.1) (figure 1). Five minutes post surgery, 100 % of patient in RA group had a pain value of 0. In GA group at 5 minutes post surgery, 32 % of patient had a value of 0 for pain, 8 % had the maximum value (10), and average was 3 (SD: 3.2). Ten minutes after surgery, 100 % of patient in RA group still had no pain (value for pain: 0), whereas only 16 % of those in GA had the same value, also 4 % of them had a value of 8 (severe pain), and average value was 4 (SD: 2.4). Fifteen minutes post surgery all patients in RA group still had no pain (Value: 0), in GA group, only 8 % had a value of 0 for pain, 4 % had a value of 7, and mean value was 3 (SD: 1.9).
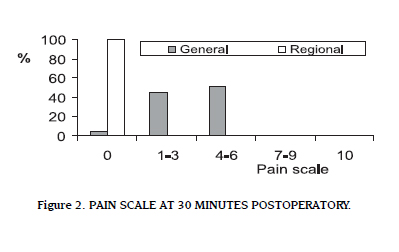
Thirty minutes post surgery (figure 2) no patient was found to have pain in RA group, whereas in GA group, only 4 % had no pain at all, 24 % had a value of 6, an their average value was 4 (SD: 1.9) .
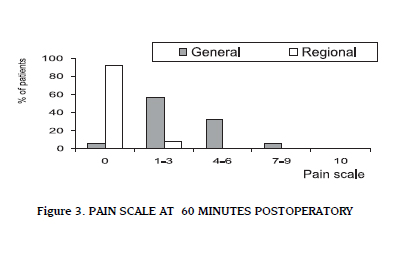
One hour after surgery (figure 3), over 90 % of patient in RA group still had a value of 0 for pain, and the maximum VAS value found in this group was 3; average value at time was 0 (SD: 0.7). Control group had a value of 0 in only 4 % of patients, and the maximum VAS value found was 8, average value was 3 (SD: 1.8).
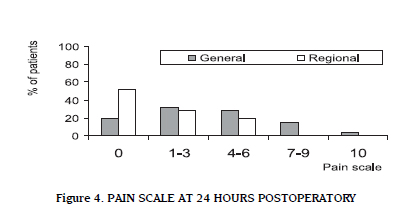
Half of RA group, reported no pain 24 hours post surgery, 30 % of patients reported only mild pain (VAS: 1-3), and 20 % reported moderate pain (VAS: 4-6). No patient reported severe pain (VAS= 7) in PNB group (Figure 4).
Summarizing, the whole RA group showed no pain at 30 minutes post surgery. After 60 minutes 82 % still had no pain, and after 24 hour of surgery 52 % of RA group had no pain at all.
Anesthesia-related complications
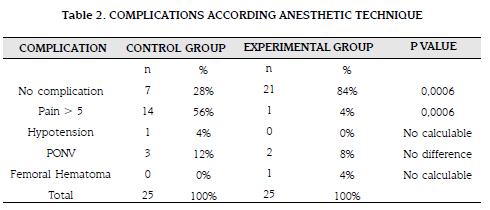
Most common complication in GA group was pain score > 5. PONV occurred in 12 % of GA group patients and in 8 % of RA group, although there was a difference, group's size were too small for comparing this variable. One patient in control group (4 %) had hypotension needing management, and a patient (4 %) in experimental group had a complication inherent to anesthetic technique (femoral hematoma), but it did not delay discharge, increase anesthetic costs, nor generate patient discomfort (table 2).
Anesthesia-related costs
At this time 1 USD is equal to $2.350 pesos (March 2009)
RA group average cost per case was $88.321 ± $29.886 (USD 37.58 ± 12.71). GA group average cost per case was $$117.501 ± $27.501 (USD 50 ± 11.70). Although RA group had anesthesia related lower cost, there was no statistic significance between values. It is important to mention that there was also a difference in post surgery analgesia cost which was principally needed in GA group, but these were not considered as part of anesthetic costs.
PACU average cost per case in GA group was $18.500 ± $11.990 (USD 7.71 ± 5.10). In RA group average cost per case was $3.750 ± $4.913 (USD 1.56 ± 2.05).
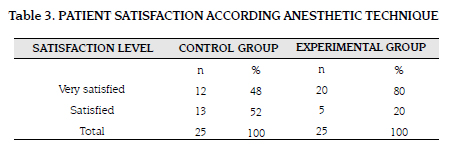
Eighty percent of individuals in RA group, felt very satisfied with the anesthetic technique, compared to 48 % of those who received GA. We consider this as the most important finding of our study due to our objective of research about different ways of giving better healthcare services to our patients (table 3).
PNBs are commonly used anesthetic techniques in orthopedic procedures; they help to optimize surgical conditions, post surgery analgesia and rehabilitation. Use of PNB has been associated to lower intensity and incidence of postoperative pain, PONV, and hospital readmissions, when compared to GA (4). Post surgery pain still is one of the most difficult obstacles to overcome in ambulatory anesthesia, inappropriate pain management is associated to higher opioid requirements, which increase PONV incidence, delay discharge, and increases hospital readmission rate (10,13).
We evaluated 50 patients, 25 were randomized to receive GA, and 25 to receive PNB as anesthetic technique for AKS. We demonstrated several advantages of PNB technique itself, as are lower incidence of postoperative pain, and no need of further analgesia in PACU. This result is consistent with the reported by Borgeat A. et al in 1200 patients (4).
A disadvantage observed with RA is the time spent in PNB performance. We applied PNB in a special place for it before taking patient into operation room, with that average intraoperative time was lower in this group (p=0,000000). These results are consistent with those found by Hadzic A. et al (15) who did not find differences in the intraoperative time between GA and PNB groups. This reinforced the necessity of create in surgical services a section specially designed for PNB placement.
PONV are determinant factors for patient satisfaction, and its incidence in ambulatory procedures is increased with the use of GA. We found a lower frequency of PONV in patients who received PNB but this difference was not significant, because the sample size was too small to evaluate this variable.
Average PACU time was lower in PNB group compared to GA group. This suggest that patients in the PNB group had better pain management, and lower PONV because this are the most common factors that would delay sign-off of patients. Similar data were found by Jankowski et al (22).
According to Avidan et al (11), patient satisfaction is a fundamental indicator of anesthetic technique quality. Satisfaction is higher if analgesia is provided using PNB rather than intravenous opioids. We found similar results because a higher percentage of patients in RA group were very satisfied than in GA group. With regard to anesthesia-related cost we found a little difference, being RA cheaper than GA but it was not of statistical significance. We believe that this is due to the protocol design employed and the simple size.
We conclude that this study suggest that regional anesthesia for ambulatory arthroscopic knee surgery provides better postoperative analgesia, earlier discharge and better patient satisfaction than general anesthesia. Regional anesthesia also seems to facilitate early rehabilitation and could provide good care at a lower cost.
REFERENCES
1. Pregler JL, Kapur PA. The development of ambulatory anesthesia and future challenges. Anesthesiol Clin N Am 2003; 21:207-228. [ Links ]
2. Webb E, Graves H. Anesthesia for the ambulatory patient. Anesth Analg 1959; 38:359-363. [ Links ]
3. Pastor PN, Makuc DM, Reuben C, Xia H. Chartbook on Trends in the Health of Americans. Health, United States, 2002. Hyattsville, Maryland: National Center for Health Statistics, 2002. [ Links ]
4. Borgeat A, Ekatodramis G, Schenker CA, Warltier DC. Postoperative nausea and vomiting in regional anesthesia: A review. Anesthesiology 2003; 98:530-547. [ Links ]
5. Trame'r MR. Strategies for postoperative nausea and vomiting. Best Pract Res Clin Anaesthesiol 2004; 18:693-701. [ Links ]
6. Gan TJ, Meyer T, Apfel CC, Chung F, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg 2003; 97:62-71. [ Links ]
7. Rosenquist RW, Rosenberg J. Postoperative Pain Guidelines. Reg Anesth Pain Med 2003; 28:279-288. [ Links ]
8. McGrath B, Chung F. Postoperative recovery and discharge. Anesthesiol Clin N Am 2003; 21:367-386. [ Links ]
9. Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg 1999; 89:652-658. [ Links ]
10. Deutsch N, Wu CL. Patient outcomes following ambulatory anesthesia. Anesthesiology Clin N Am 2003; 21:403-415. [ Links ]
11. Avidan A, Drenger B, Ginosar Y. Peripheral nerve block for ambulatory surgery and postoperative analgesia. Curr Opin Anesthesiol 2003; 16:567- 573. [ Links ]
12. Jenkis K, Grady D, Wong J, et al. Post-operative recovery: day surgery patients' preferences. Br J Anaesth 2001; 86:272-274. [ Links ]
13. Mulroy MF, McDonald SB. Regional anesthesia for outpatient surgery. Anesth Clin N Am 2003; 21:289-303. [ Links ]
14. Enneking FK, Chan V, Greger J. Lower-Extremity peripheral nerve blockade: Essential of our current understanding. Reg Anesth Pain Med 2005; 30:4-35. [ Links ]
15. Hadzic A, Karaka PE, Hobeika P, et al. Peripheral nerve blocks result in superior recovery profile compared with general anesthesia in outpatient knee arthroscopy. Anesth Analg 2005; 100:976-981. [ Links ]
16. Fleiss JL. Statistical methods for rates and proportions. John Miley and Sons Company. Second edition. 1981. [ Links ]
17. Brown AK, Christo PJ, Wu CL. Strategies for postoperative pain management. Best Pract Res Clin Anaesthesiol 2004; 18:703-717. [ Links ]
18. Hadzic A, et al. Textbook of regional anesthesia and acute pain management. 1st ed, Chapter 37 p 517-532. New York: McGraw-Hill Companies; 2007. [ Links ]
19. Singelyn FJ. Textbook of regional anesthesia and acute pain management. 1st ed, Chapter 35 p 499- 508. New York: McGraw-Hill Companies; 2007. [ Links ]
20. Bouaziz H. Textbook of regional anesthesia and acute pain management. 1st ed, Chapter 34 p 489- 498. New York: McGraw-Hill Companies; 2007. [ Links ]
21. Kittelberger KP, Lebel AA, Borsook D. Valoración del dolor. Massachussets General Hospital tratamiento del dolor 26-30. 1999 [ Links ]
22. Jawkosi CJ, Hebe JR, Stuart MJ, et al. A comparison of psoas compartment block and spinal and general anesthesia for outpatient knee arthroscopy. Anesth Analg 2003, 97; 1003-9. [ Links ]
Recibido: marzo 10 de 2009. Revisado: abril 25 de 2009. Aceptado: mayo 4 de 2009
Forma de citar: González Obregón MP, Vásquez Sadder MI, Herrera-Morales LA, Rivera Diaz RC, Arcila Lotero MA, Puerta Martínez JJ, Trujillo Hinestroza LM, Torres Y. General versus regional anesthesia for ambulatory arthroscopic knee surgery. Rev CES Med 2009; 23(1):7-16