Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
CES Medicina
versión impresa ISSN 0120-8705
CES Med. v.23 n.2 Medellín jul.(dic. 2009
ARTÍCULOS DE INVESTIGACIÓN CIENTÍFICA O TECNOLÓGICA
Association of severe malaria with ABO-blood group types in an endemic zone of Colombia
Asociación de malaria severa con tipo de grupo sanguíneo ABO en una zona endémica de Colombia
ANA MILENA HERRERA1, LILIANA PATRICIA MONTOYA2, MARGARITA ARBOLEDA3, LUISA FERNANDA ORTIZ4
1 Ph. D en Patología. Docente Facultad de Medicina – - - Universidad CES. Grupo de investigación Ciencias Básicas. Correo electrónico: aherrera@ces.edu.co
2 Magíster en Epidemiología. Docente Facultad de Medicina - Universidad CES. Grupo de investigación Observatorio de la Salud Pública.
3 Magíster en Medicina Tropical. Investigadora Instituto Colombiano de Medicina Tropical. Grupo de investigación Instituto Colombiano de Medicina Tropical.
4 Médico. Universidad CES.
ABSTRACT
Introduction: malaria is considered one of the most important tropical illnesses in public health causing millions of infections and deaths each year. Many studies have tried to establish an association between the severe form of the disease and the ABO-blood group type. In Colombia, a country with large endemic zones for malaria there are not enough studies or statistic data about this possible association.
Methods: a retrospective case-control study of patients with severe and uncomplicated malaria in the endemic zone of Apartadó, Colombia, was performed between January 2000 and June 2006. Only the clinical records with blood group ABO and Rh classification were included.
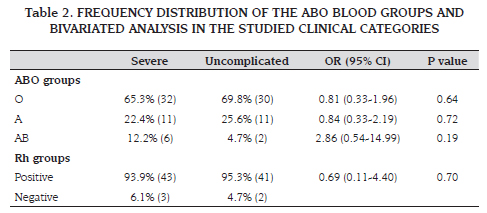
Results: a total sample of 92 patients was obtained: 49 with severe malaria and 43 with uncomplicated malaria. From the total sample, 68.5% were women and the median age of 21.5 years (min 1-max 80). Of the patients with diagnosis of severe malaria, 59.2 % were women. The more frequent parasite species was Plasmodium falciparum. Severe malaria was more frequent among patients classified with blood group O (65.3 %) and positive Rh (93.9 %), but this association was not statistically significant.
Conclusion: even though severe malaria was more frequent among patients classified with blood group O and positive Rh, an association between blood group and severe malaria could not be established. The controversial association of these variables previously found in other populations could be probably explained by the demographic distribution and characteristics of those.
KEY WORDS
Malaria, ABO blood Group system, Colombia
RESUMEN
Introducción: la malaria es considerada una de las más importantes enfermedades tropicales en salud pública, causando millones de infecciones y muertes cada año. Muchos estudios han tratado de establecer una asociación entre la forma grave de la enfermedad y la clasificación sanguínea ABO. En Colombia, un país con grandes zonas endémicas de malaria, no existen suficientes estudios y datos estadísticos acerca de esta posible asociación.
Objetivo: identificar pacientes con trastornos de la deglución, en una unidad de cuidados especiales y caracterizar las causas directas de dichos trastorno
Métodos: se realizó un estudio de casos y controles de pacientes con malaria severa y no complicada en la zona endémica de Apartadó, Colombia y ejecutado entre enero de 2000 y junio de 2006. Sólo las historias clínicas con información acerca de la clasificación sanguínea ABO o Rh fueron incluidas.
Resultados: la muestra total fue de 92 pacientes, 49 con malaria grave y 43 con malaria no complicada. De la muestra total, 68,5% eran mujeres y la edad media de 21,5 años (mínimo 1-máximo 80). De los pacientes con diagnóstico de malaria grave, 59,2 % eran mujeres. El parásito más frecuente fue la especie de P. falciparum. La malaria grave fue mas frecuente entre los pacientes clasificados con grupo sanguíneo O (65,3 %) y Rh positivo (93,9 %), pero esta asociación no fue estadísticamente significativa.
Conclusión: aunque la malaria severa fue mas frecuente en pacientes con grupo sanguíneo O y Rh positivo, una asociación entre la severidad de la malaria y la clasificación sanguínea no pudo ser establecida. La controvertida asociación entre estas variables previamente encontrada en otras poblaciones, probablemente puede ser explicada por la distribución y características demográficas de dichas poblaciones.
PALABRAS CLAVES
Malaria, Clasificación grupo sanguíneo ABO, Colombia
INTRODUCTION
Malaria is considered a worldwide major public health problem (1) as it is the most important parasite disease affecting humans and causing millions of deaths each year (2). In tropical and subtropical regions of the world, it is estimated that malaria is responsible for 300 to 500 millions of infections and 2 to 3 millions of deaths per year (3); being considered as one of the main health problems in regions like Africa, India, Southeast of Asia, and South America (4). Given the optimal environmental conditions for malaria transmission among different territories of Colombia, the country is considered as one of the endemic zones in the world (1,3). In the Colombian zones of Urabá and Bajo Cauca (1998), among the people affected by the disease, the reported parasite species prevalence is 66 % for P. vivax and 33 % for P. falciparum (1). The latest, is the parasite widely associated with a more severe presentation of the disease (1,2). However, besides the parasite species, the clinical presentation and severity of the disease are influenced by the geographic zone, demographic characteristics and host susceptibility (5).
Many pathophysiological mechanisms have been postulated to explain host susceptibility for parasite colonization and clinical presentation of the disease. Some studies have suggested that host susceptibility could be linked to the ABOblood group and/or Rh type due to the presence of different erythrocyte receptor systems that act as ligands to facilitate parasite adhesion (6).
Several authors have stated that while groups A, B, and O seem to be equally susceptible to the infection, group AB show less propensity to infections. Additionally, it is suggested that groups A and O exhibit less colonization by P. falciparum (7). In a systematic review published in 2007, it was reported that while in 7 different studies a significant association between P. falciparum malaria and ABO blood classification was found, this association could not be demonstrated in other seven studies (8). About Rh classification, many studies have found a protective association between negative Rh and the susceptibility to P. vivax malaria as this blood group get less infections (9,10).
In terms of the severity of the disease, it has been found that severe malaria frequency is in linear relation with parasite concentration and intra-erythrocyte rosettes formation mainly by P. falciparum that invades all type of erythrocytes involving complex physiopathological processes deriving in more severe effects (1,6). P. falciparum erythrocyte invasion and rosette formation is believed to be favored by erythrocyte surface antigens among the different ABO-blood group and Duffy types (6). Some studies have found that P. falciparum form rosettes with more frequency in those erythrocytes with A and B blood groups, but less frequently in those of group O, which could indicate some resistance of this group to the severe presentation of malaria (8,11-15).
At the epidemiological level and only considering the clinical studies, a clear association between severe malaria and blood group classification has not been established (16). Some comparative studies have demonstrated differences in terms of blood group types and the presence of severe malaria concluding that patients with group O could be more resistant to the infection by P. falciparum (14,15). However, other studies have failed to demonstrate this association (16,17). In a recent publication, Cserti and Dzik (2007) suggested that the controversial association between severe malaria and ABO blood groups is closely related to the geographic distribution of the different blood groups among the endemic zones (16). These studies have been performed in many tropical territories affected by malaria around the world, however, in Colombia, a country with large endemic zones; there are no many similar studies or statistic data about this alleged association.
MATERIALS AND METHODS
All the clinical records of hospitalized patients with malaria, in the regional hospital of the Apartadó town, an endemic zone of Urabá (Colombia) during the period of January 2000 and December 2005 were evaluated. The clinical records of patients with malaria and ABO blood group and Rh classification were included. A retrospective case-control study of patients diagnosed with severe malaria and uncomplicated malaria during this period was performed. Neonatal malaria was used as exclusion criteria.
The cases of severe malaria were defined by the presence of one or more of the following criteria based on the report published by the World Health Organization (WHO, 2000) (18) and adapted by the researchers keeping into account the criteria established in Colombia by the Ministry of Social Protection for malaria falciparum parasitemia and severe anemia (2007) (19), and for severe trombocitopenia according to the definition published by Tobon et al. 2006 (20): cerebral malaria (defined as unrousable coma not attributable to any other cause in a patient with falciparum malaria), severe normocytic anaemia (hemoglobin <7.0 mg/dL and hematocrite <20 % -adapted by the researchers-, hypoglycaemia (glucose <40 mg/dL), metabolic acidosis with respiratory distress, fluid and electrolyte disturbances, acute renal failure (creatinin >3.0 mg/dL), acute pulmonary oedema and adult respiratory distress syndrome (ARDS), circulatory collapse, shock, septicaemia, abnormal bleeding, jaundice (total bilirrubin TB >3.0 mg/dL),haemoglobinuria, hyperparasitaemia (>50,000 asexual parasites / µL* -adapted by the researchers-), severe thrombocytopenia (platelets <20.000/µL -adapted by the researchers-).
Information about demographic variables, blood group classification, and parasite type and laboratory tests values was collected from each clinical record of both groups: uncomplicated malaria and severe malaria. Data was processed in the statistic software SPSS 10®. Bivariated analysis to evaluate differences between numeric variables between cases and controls was performed through the U Mann-Whitney test and to evaluate the association between categorical variables a Chi-square test was performed. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. A p value <0.05 was set for statistical significance.
RESULTS
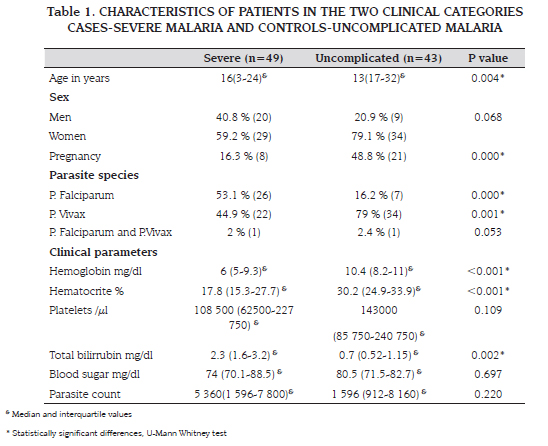
A total of 197 clinical records of hospitalized patients with malaria between January 2000 and December 2005 in the Hospital Antonio Roldán Betancur were initially evaluated, of those, 92 records fulfilled the inclusion criteria of having information about ABO or Rh blood classification. The sample was conformed by 49 patients in the group of cases and 43 in the control group. Median age of the total sample was 20 years (interquartile range 5.5-28 years) and 68.5 % (63/92) were women, from these, 46 % (n=29) were in the third trimester of pregnancy. The frequency distribution of the different ABO blood groups of the total sample was: group O (67.4 %), group A (23.9 %) and group AB (8.7 %). In terms of Rh classification, 94.6 % of patients of the total sample were classified as positive. The more frequent parasite in the total sample was P. vivax (61.5 %), followed by P. falciparum (36.3 %). Mixed malaria by both parasites was present in 2 patients (2.2 %). The demographic and clinical characteristics of patients of cases and control groups are displayed in table 1.
In the group of cases of severe malaria (n=49) the diagnosis was performed by the following criteria: severe anemia 69.4 % (34), ADRS in 22.4 % (11), hyperparasitemia in 16.7 % (8), hepatic failure 14.6 % (7), severe thrombocytopenia in 4.2 % (2), renal failure 2.1 % (1), and cerebral malaria 2.1 % (1). There were no cases diagnosed by severe hypoglycemia. There was one death caused by severe malaria.
The bivariated analysis to establish association between severity of the disease and the ABO and Rh blood group classification did not show statistical significance for any of the blood types.
Table 2 displays the calculated OR values with their respective 95 % CI for each of the groups with respect of severity of malaria.
With regard to the association of the rest of variables with the severity of malaria, a statistically significant association between this one and sex was found (OR 2.60, 95 % CI 1.03-6.60; p=0.044) being males 2.6 times more at risk of developing severe malaria than females. Examining the association of the severity of the disease and range of age, it was observed that severe malaria affects significantly more those patients between one and 12 years of age (OR 5.46, 95 % CI 1.78-17.51; p=0.0015). Also, there was significant association with the parasite species being P. falciparum as a risk factor (OR 5.65, 95 % CI 1.92-17.21; p=0.0003) and P. vivax as a protective factor (OR 0.19, 95 % CI 0.07-0.54; p=0.0004) for developing severe malaria. Pregnancy also presented a significant association with severe malaria (OR 0.24, 95 % CI 0.07-0.77; p=0.006). As in the rest of patients of the sample, in pregnant women, severe malaria did not show significant association with the ABO blood Group classification.
Evaluating parasite species and its possible association with any blood type, it was found that for infection with each of both parasites: P. falciparum and P. vivax, the most frequent blood type was O (75.8 % for P. falciparum and 62.5 % for P. vivax) without any significant association between this blood type and parasite species.
DISCUSION:
Several reports in the literature establish association between the blood classification system ABO and malaria; specifically between group AB and severe malaria and refer that people with blood type O are relatively resistant to develop severe malaria by P. Faciparum (8,9,14,15). In the present study, an association between blood group and severe malaria was not found. These findings are similar to what was reported by Montoya et al. where no association could be established between the presence of ABO antigens and malaria by P. Falciparum or P.Vivax in 4 different ethnic groups in Colombia (9). Alike, Cavasin et al. found similar frequencies of ABO phenotype between blood donors and malaria patients in 4 areas of Brazilian Amazone (10). In another Amazonic area, Beiguelman et al. also failed to find such association arguing that it is probably due to the geographic distribution of the different ABO phenotypes in this region (21). In the present study, 65.3 % of the cases of severe malaria were blood type O, different from what was found by Pathirana et al (15) where the ratio was of 23.8 %; also, in that study, type A was the most frequent (32.5 %) and type B represented 27.5 %. In the present study no cases of severe malaria had blood type B. In uncomplicated malaria patients the predominant blood type was also O, while Pathirana's reported 47.9 % (15). These findings support more the idea that the alleged association between blood type and severity of malaria depends on the demographic distribution and characteristics of the studied population, as every region in the world seems to have different ABO phenotype distribution.
The demographic characteristics of the evaluated population in the present study suggest in general a higher frequency of the disease in women specially those in their third trimester of pregnancy. The bivariated analysis indicated that males are at more risk of developing severe malaria, however, there are not physiopatological mechanisms that could explain this association. This situation could be explained from the public health system point of view, as the strict prenatal assistance and control system of our country assures that women in fertile age and during pregnancy could be detected rapidly in the early phases of the disease avoiding the progression of malaria to a severe stage. Therefore, the ratio of 20 of 29 males affected by severe malaria contrast with the ratio of 29 of 63 females with the same diagnosis probably indicating that even though in this study malaria is more frequent among women, its progress to a severe stage is less frequent in those as well. Another explanation could be the fact that pregnant women with uncomplicated malaria are hospitalized and given special care due to their condition, therefore avoiding complications of their disease (22).
The median age of affected patients by the severe disease was constituted by young adults, but after performing the analysis by groups of age, a high frequency of severe malaria in the age group between 1-12 years was evident. This is possibly due to the susceptibility of children to experience a more severe form of the disease given the poor immunological and nutritional conditions of this population (23-25).
In agreement with the epidemiological data found in our country and previously described in the literature, in the total sample of this study, the most frequent parasite for non complicated malaria found in this endemic zone was P. vivax, and for severe malaria was P. falciparum being a risk factor for its development as has already been described for many dacades (1,20). Only 2 patients presented mixed infection by P. falciparum and P. vivax, one of them manifested the severe form of the disease.
The majority of severe cases of malaria were diagnosed by the presence of severe anemia given by highly compromised levels of hemoglobin and hematocrit. This contrast with the results obtained by Tobón et al. (2006) in two Colombian populations, where severe malaria diagnose was more frequently performed by hyerparasitemia and hepatic failure, and less frequently due to severe anemia (20). However, this finding is in agreement with other studies where severe anemia is reported as one of the most frequent parameters for the diagnose of severe malaria in other populations probably due to their geographic conditions (15-17). Coherent also with the reported in the literature, there were not cases of severe malaria diagnosed by severe hypoglycemia (15-17).
CONCLUSION
In the present study, although severe malaria was more frequent among patients classified with blood group O (65.3 %) and positive Rh (93.9 %), an association between blood group and severe malaria could not be established. These findings support more the idea that the alleged association between blood type and severity of malaria depends on the demographic distribution and characteristics of the studied population, as every region in the world seems to have different ABO phenotype distribution.
REFERENCES
1. Botero D, Restrepo M. Malaria. En: Parasitosis Humanas. Tercera edición. Medellín, Colombia. 1998. p.158-201. [ Links ]
2. W hite JN, Breman GJ. Malaria and Babesiosis: Diseases caused by red blood cell parasites. En: Harrison's principles of internal medicine. Edición 16. Mc Graw Hill. 2005. p.1218-1233. [ Links ]
3. W orld Health Organization. Expert Committee on Malaria. WHO technical report series 892, i-v. World Health Organization, Geneva; 2000. [ Links ]
4. W orld Health Organization (2003) The African malaria report 2003. World Health Organization, Geneva [ Links ]
5. Thakur A, Verma IC. Malaria and ABO blood groups. Indian journal Malariol. 1992; 29 (4):241-4. [ Links ]
6. Daniels G. Blood group polymorphisms: molecular approach and biological significance. Transfus. Clin. Biol. 1997. 4:383-390. [ Links ]
7. Singh N, Shukla MM, Uniyal VP, Sharma VP. ABO blood groups among malaria cases from district Mandla, Madhya Pradesh. Indian Journal Malariol. 1995; 32 (2): 59-63. [ Links ]
8. Uneke CJ. Plasmodium falciparum malaria and ABO blood group: is there any relationship? Parasitol Res. 2007; 100(4):759-65. [ Links ]
9. Montoya FM, Restrepo AF. Blood groups and malaria. Rev. Inst. Med. Trop. São Paulo 1994; 36:33-38. [ Links ]
10. Cavasin CE, De Mattos LC, Tome Alves R, Couto AA, Pachiano VS, Bonin CR, Castilho L, et al. Frequencies of ABO, MNSs, and Duffy phenotypes among blood donors and malaria patients from four Brazilian Amazon areas. Human Biology. 2006; 78 (2):215-219. [ Links ]
11. Udomsangpetch R, Todd J, Carlson J, Greenwood B.M. The effects of hemoglobin genotype and ABO blood group on the formation of rosettes by Plasmodium Falciparum infected red blood cells. Am. J. Trop. Med. Hyg. 1993;48 (2): 149-153. [ Links ]
12. Barragan A, Kremsner P.Wahlgren M, Carlson J. Blood group A is a coreceptor in plasmodium falciparum roseting. Infection and Immunity. 2000; 68 (5): 2971-2975. [ Links ]
13. Rowe A, Obeiro J, Newbold C.I, Marsh K. Plasmodium Falciparum rosetting is associated with malaria severity in Kenya. Infection and Immunity. 1995; 63 (6): 2323-2326. [ Links ]
14. Rowe JA, Handel IG, Thera MA, Deans A-M, Lyke KE, Kone A, Diallo DA, et al. Blood group O protects against severe Plasmodium Falciparum malaria through the mechanism of reduced resetting. PNAS. 2007;104 (44): 17474-17476. [ Links ]
15. Pathirana SL, Alles HK, Bandara S, Phone- Kyaw M, Prerra MK, Wickremassinghe AR, Mendis KN, Handunnetti Sm. Abo-bloodgroup types and protection against severe, plasmodium falciparum malaria. Ann tropical Medicine Parasitol. 2005; 99 (2): 119-24. [ Links ]
16. Cserti C.M, Dzik W.H. The blood group system and Plasmodium Falciparum malaria. Blood. 2007;110: 2250-2258. [ Links ]
17. Fischer P, Boone P. Short report: severe malaria associates with blood group. Amer J Trop Med Hyg. 1998; 58 (1): 122-123. [ Links ]
18. W orld Health Organization. Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg 2000; 94 (Suppl 1):S1- 90. [ Links ]
19. Colombia, Ministerio de la Protección Social. Guías y Normas 412 - Tomo 3. Guías de promoción de la salud y prevención de enfermedades en la salud pública. Guía 19. Guía de Atención de la Malaria. 2007; p. 71-131. [ Links ]
20. Tobón A, Giraldo C, Pineros JG, Arboleda M, Blair S, Carmona-Fonseca J. The epidemiology of complicated falciparum malaria: case and controls study in Tumaco and Turbo, Colombia 2003. Rev. Bras. Epidemiol. 2006; 9(3):283-296. [ Links ]
21. Beiguelman B, Alves P.F, Moura M.M. Association of genetic markers and malaria infection in the Brazilian Western Amazonian region. Mem. Inst. Oswaldo Cruz. 2003;98 (4): 455-460 [ Links ]
22. Schantz-Dunn J, Nour NM. Malaria and pregnancy: a global health perspective. Rev Obstet Gynecol. 2009; Summer;2(3):186-92. [ Links ]
23. Crawley J, Nahlen B. Prevention and treatment of malaria in young african children. Semin Pediatr infect dis. 2004; 15 (3): 169-180. [ Links ] 24. Maitland K, Marsh K. Pathophysiology of severe malaria in children. Acta Trop. 2004; 90 (2): 131-140. [ Links ]
25. Dubos F, Dauriac A, El Mansouf L, Courouble C, Aurel M, Martinot A, the Hospital Network for Evaluating the Management of Common Childhood Diseases. Imported malaria in children: incidence and risk factors for severity. Diagn Microbiol Infect Dis. 2009 Sep 28. [Epub ahead of print] [ Links ]
Recibido: junio de 2009. Revisado: Julio de 2009. Aceptado: noviembre 20 de 2009
Forma de citar: Herrera AM, Montoya LM, Arboleda M, Ortiz LF. Asociación de la malaria severa con tipo de grupo sanguíneo ABO en una zona endémica de Colombia. Rev CES Med 2009;23(2):9-16.