Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
CES Medicina
Print version ISSN 0120-8705
CES Med. vol.23 no.2 Medellín July/Dec. 2009
REPORTE DE CASO
Terminal ileum perforation secondary to an impacted phytobezoar: case report and review of the literature
Perforación del ileon terminal por un fitobezoar impactado: reporte de caso
HEINZ GEORG HILLER1, MUSTAFAH RASHID ELAH ABDEL-HALIM,2 NICHOLAS RAUL FERNANDO LAGATOLLA3
1 Vascular surgeon at the Fundación Cardioinfantil, BogotáColombia. heinzhiller@gmail.com
2 Surgical registrar at Department of General and Vascular Surgery. Dorset County Hospital, UK
3 Consultant Vascular Surgeon at Department of General and Vascular Surgery Dorset County Hospital, UK
ABSTRACT
Bezoars are concretions of undigested food particles, medications, milk formulas and hair. The most common presentation of a bezoar is in the form of a phytobezoar, which is caused by precipitation of undigested particles of vegetables and seeds. Small bowel obstruction is mainly caused by adhesions from previous surgery. Of all causes of intestinal obstruction, phytobezoars are responsible for only 0.4-4 % of all causes. They are mainly precipitated by previous strictures caused by surgery, partial gastrectomy, Crohn's disease or intestinal tuberculosis. Symptoms can range from a vague abdominal discomfort to nausea, early satiety, vomiting, halitosis and weight loss. Perforation is a rare complication in an intact abdomen because patients seek early medical treatment before this occurs. We describe the case of an 85 year old male patient, who presented with perforation of the terminal ileum, caused by an impacted phytobezoar and caused a localised abscess that was successfully treated with surgery.
KEY WORDS
Bezoar, Enterolith, Enteric Perforation, Foreign Body, Intestinal Obstruction
RESUMEN
Los bezoares son concreciones de porciones de alimento no digerido, medicamentos, fórmulas de leche o cabello. La presentación más común del bezoar es en la forma de fitobezoar, el cual es causado por la acumulación de partículas sin digerir de verduras y semillas. La obstrucción del intestino delgado es causada principalmente por adherencias de anteriores cirugías. Los fitobezoares son responsables de sólo 0,4-4 % de todas las causas de obstrucción intestinal. Tales obstrucciones son principalmente provocadas por estenosis anteriores secundarias a cirugía, gastrectomía parcial, enfermedad de Crohn o tuberculosis intestinal. Los síntomas pueden variar desde una molestia abdominal vaga hasta náuseas, saciedad precoz, vómitos, mal aliento y pérdida de peso. La perforación es una complicación poco frecuente en un abdomen intacto, porque los pacientes buscan tratamiento médico temprano antes de que esto ocurra. Se describe el caso de un paciente de 85 años de edad, que se presentó con perforación del íleon terminal, causada por un fitobezoar impactado que le causó un absceso localizado, el cual fue tratado con éxito mediante cirugía.
PALABRAS CLAVE
Bezoar, Enterolito, Perforation intestinal, Cuerpo extraño, Obstrucción intestinal
INTRODUCTION
Bezoars are concretions of substances that can´t be digested by normal means and can occur in any segment of the gastrointestinal tract, most commonly in the stomach. They can be composed almost by any substance such as hair, pills, seeds and undigested vegetables. Bezoars form in the majority of cases in patients with altered intestinal motility and in patients with previous intestinal surgery and can be classified in four types depending on their origin and components: trichobezoar, phytobezoar, lactobezoar and lactobezoar (table 1) (1,2).
Phytobezoars are the most common form of bezoars in humans and are primarily formed in the ileum, especially in the presence of strictures caused by Crohn's disease, intestinal tuberculosis, previous surgery or even form inside diverticulae. They can also occur in the stomach by the concretion of poorly digested fruit and vegetable fiber predisposed by disturbed gastric motility and decreased acidity in patients after a gastrectomy or vagotomy, and by autonomic intestinal dysmotility in diabetic patients. They are mainly composed of cellulose, hemicellulose, tannins and lignin which can be found in foods such as celery, raisins, prunes, grape skins and most notably persimmons. In high concentrations these foods form a coagulum that upon exposure to and acidic environment begin the formation of a bezoar (4-6).
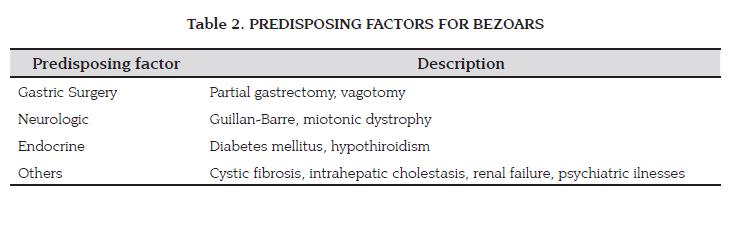
The most common factors predisposing to the formation of bezoars include previous surgery such as partial gastrectomy and vagotomy and previous small bowel surgery. Medical causes are also associated with this presentation such as hypothiroidism, Guillan -Barre syndrome, diabetes mellitus, cystic fibrosis and psychiatric illnesses with trichophagia (table 2) (7,8).
Clinical manifestations of phytobezoars include chronic indigestion and early satiety and chronic abdominal pain. The most common clinical presentation is a vague epigastric or lower abdominal discomfort. Other symptoms include dysphagia, anorexia, halitosis and weight loss. Of all causes of intestinal obstruction, of which the most common are adhesions. Phyotbezoars account only for 0.4-4 % of all causes and rarely cause perforation. Diagnosis of phytobezoars can be difficult at times, depending on the level of impaction. Clinical examination may reveal a mass at the site of impaction. Plain abdominal films may only show unspecified loops of dilated bowel, and barium studies may show a filling defect as the barium surrounds the bezoar. If the impaction occurs in the stomach, gastroscopy is the method of choice and can be used as a treatment strategy to either fragment or retrieve the bezoar. Abdominal CT scanning has proven useful especially to detect the presence of localised obstruction or perforation (9,10).
We present the case of an 85 year old male patient admitted to hospital with a diagnosis of peritonitis caused by a perforated intestine. During laparotomy the cause was found to be an impacted phytobezoar at the terminal ileum with perforation of the adjacent ileum and abscess formation.
CASE PRESENTATION
An 85 year old male patient was admitted to the emergency department with a three day history of progressive, severe right iliac fossa pain and partial constipation. Previously, he had been suffering of intermittent and self-limiting abdominal pain in the same region. The past medical history included non-insulin dependent diabetes mellitus, chronic atrial fibrillation, hypertension and aortic stenosis with an 80mmHg gradient.
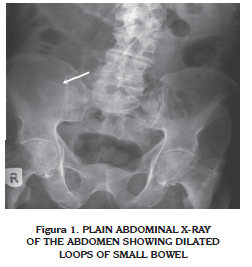
On clinical examination he was dehydrated, with an irregular tachycardia at 103 bpm and normotensive. His abdominal examination revealed a tender, immobile mass in the right iliac fossa. The rest of his examination revealed an ejection systolic murmur, normal respiratory findings and no neurological deterioration. Blood tests revealed a high C-Reactive Protein (313.9 mg/L) in the presence of normal leucocytic count, haemoglobin and serum electrolytes. A plain abdominal film was obtained, which showed small bowel loop dilation with collapsed large bowel and a rounded, radio-opaque shadow projected over the right ileum (Fig 1).
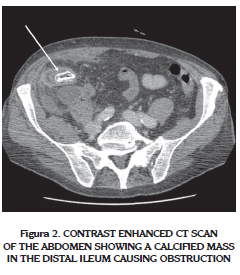
An abdominal CT scan revealed thickening of the terminal ileum, surrounding free peritoneal fluid and a calcified mass in the lumen. The rest of the abdomen was reported as normal. (Fig 2)
Conservative management was initiated with alimentary rest, intravenous fluids and antibiotics, but his signs developed into peritonitis of the abdomen. The patient was taken for a laparotomy, which revealed an abscess in the right paracolic gutter involving the caecum and the terminal ileum. On inspection of the lumen a 3 x 3 cm enterolith was found impacted in the ileocaecal valve causing perforation. A limited right hemicolectomy was performed and sutured with an end to end anastomosis. The patient recovered uneventfully and was discharged after seven days. Histological analysis revealed a phytobezoar, with chronic inflammation of the terminal ileum and caecum. No malignancy or other anatomical anomalies were found.
DISCUSIÓN
The prevalence of bezoars is largely unknown due to the vague clinical presentations especially for a high incidence of sub-diagnosis of the disease. From a surgical point of view, obstruction of any part of the gastrointestinal tract caused by a Bezoar is rare, accounting for only 0.4 to 4 % of all causes of abdominal obstruction. Perforation of the small bowel is even rare because patients usually seek medical advice early in the presentation before this complication occurs. This presentation and perforation of the terminal ileum secondary to a bezoar has been only reported in very few cases (1,2,8).
Typically, the presentation is of a small bowel obstruction that fails to resolve with conservative management. The most common site of obstruction and perforation described in the previous reports, in the absence of any other anatomical precipitants is at the ileo-caecal valve. From our review of articles as far behind a 1993, there are only 17 case reports of obstruction caused by bezoars precipitated by different causes. In one of the larger series of cases by Dirican et al (11) they describe the surgical management of 24 patients in a period of 10 years. The most common cause of obstruction was an impacted bezoar at the site of previous gastric surgery (83.3 %).
In this report, it was clear that CT scanning of the abdomen was able to identify the bezoar causing the obstruction in all patients. Other causes for precipitating obstruction have been described such as a bezoar impacted in strictures caused by Crohn’s disease, (10,12-14); there are two case reports of bezoars causing ileus and obstruction in a Meckel’s diverticulum and a Jejunal diverticulum (in 3 cases) (15-17), and more recently there is a case report by Wilhelmi MH et al. of a phytobezoar in a "healthy adult with a long year history of vegetarian lifestyle" (18).
Perforation of the small bowel caused by an obstructing bezoar is very rare, finding only three reports in the literature since 1993 (19-21). The most plausible explanation for this, is that patients usually seek early medical advice due to the obstructing symptoms, and these perforations occur more due to the impaction of the bezoar and perforation by erosion of the intestinal wall rather than directly through the pressure build up from the obstruction, which is the mechanism underlying the perforation in our case report.
Diagnostic modalities include clinical examination which may reveal a mass in the affected segment in about 30 % of cases, a plain abdominal film which shows only in half of the cases a radio-opaque shadow at the site of obstruction with proximal bowel dilatation. Ultrasound has been evaluated and can be a useful tool in detecting bezoars especially if they are calcified (22). This method, however, is subject to the expertise of the sonographer and the high index of suspicion for the differential diagnosis. More recently, CT scanning of the abdomen reveals more precisely the cause of bowel obstruction with a higher sensitivity and specificity in different case reports (11,23).
Details of the different treatment methods are beyond the scope of this case report but briefly, for bezoars located in the stomach, endoscopic fragmentation or retrieval is the standard treatment. In the cases presenting with distal bowel obstruction and perforation, a laparotomy or a laparoscopic enterotomy is the only available treatment method (10). At operation, patients should be thoroughly assessed for diverticulae and especially strictures associated to Crohn's disease, and tissue samples must be obtained for definitive diagnosis. In our case no anatomical cause was found for the perforation on laparotomy. The presence of the bezoar could only be explained by the patient's diabetes and gastric dismotility and simple impaction in the ileocaecal valve which unfortunately led to perforation of the small bowel. At present only dietary recommendations are made for the long term prevention of this disease.
CONCLUSIONS
Obstruction of the small intestine by a phytobezoar is a rare presentation of bezoars of the alimentary tract, but no uncommon, and should be part of the differential diagnosis especially in patients with known predisposing factors. CT scanning of the abdomen remains the most reliable method for diagnosing the presence of a phytobezoar in the digestive tract. At present, surgery remains the mainstay of treating effectively an impacted phytobezoar of the small bowel with or without perforation.
REFERENCES
1. Andrus CH, Ponsky JL. Bezoars. classification, pathophysiology, and treatment. Am J Gastroenterol, 1988;83(5):476-478. [ Links ]
2. Pfau P, Ginsberg G. Foreign Bodies and Bezoars. In Feldman: Sleisenger and Fordtran's Gastrointestinal and Liver Diseases, 7th edition. 2002:395-397. [ Links ]
3. Holloway WD, Lee SP, Nicholson GI. The composition and dissolution of phytobezoars. Arch Pathol Lab Med, 1980;104:159- 161. [ Links ]
4. Matsuo T, Ito S. The chemical structure of kaki- tannin from immature fruit of the persimmon. Agric Biol Chem, 1978; 126:421- 424. [ Links ]
5. Izumi S, Isida K, Iwamoto M. The mechanism of the formation of phytobezoars, with special reference to the persimmon ball. Jpn J Med Biochem, 1933;2:21-35. [ Links ]
6. Bowden TA, Hooks VH, Mansberger AR. The stomach after surgery: An endoscopic perspective. Ann Surg, 1983;197:637- 644. [ Links ]
7. De Backer A, Van Nooten V, Vandenplas Y. Huge gastric trichobezoar in a 10-year-old girl: Case report with emphasis on endoscopy in diagnosis and therapy. J Pediatr Gastroenterol Nutr, 1999;28:513-515. [ Links ]
8. Kim JH, Ha HK, Sohn MJ, et al. CT findings of phytobezoar associated with small bowel obstruction. European Radiology, 2003;13:299-304. [ Links ]
9. Teng HC, Nawawi O, Ng KL, Yik YI. Phytobezoar: an unusual cause of intestinal obstruction. Biomed Imaging Interv J. 2005; 1-4(1) [ Links ]:
10. Jones MW, Koper B, Weatherhead WF. Crohn's disease with enterolith treated laparoscopically. JSLS. 2005; 9 (3): 339-41. [ Links ]
11. Dirican A, Unal B, Tatli F, Sofotli I, Ozgor D, Piskin T, Kayaalp C, Kirimlioglu V. Surgical treatment of phytobezoars causes acute small intestinal obstruction Bratisl Lek Listy. 2009;110(3):158-61. [ Links ]
12. Shah SR, Bhaduri A, Desai DC, Abraham P, Joshi A. Obstructing enterolith as presenting feature in Crohn's disease. Indian J Gastroenterol. 2003; 22 (1): 24. [ Links ]
13. Geoghegan T, Stunel H, Ridgeway P, Birido N, Geraghty J, Torreggiani WC. Small bowel obstruction secondary to a giant enterolith complicating Crohn's disease. Ir J Med Sci. 2005; 174 (2): 58-62 [ Links ]
14. Harrington S, Mohamed S, Bloch R. Small bowel obstruction by a primary phytobezoar in Crohn's disease. Am Surg. 2009 Jan;75(1):93-4 [ Links ]
15. Ozdemir S, Gülpinar K, Leventoglu S, Aydin S, Ozçay N. A case report of intestinal obstruction due to phytobezoar within Meckel's diverticulum. Turk J Gastroenterol. 2009 Mar;20(1):76-7 [ Links ]
16. Lough E, Richmond B, Maxwell D, Hayes JD. Obstructing phytobezoar arising from proximal jejunal diverticulum. Am J Surg. 2008 Jan;195(1):106-7. [ Links ]
17. Steenvorde P, Schaardenburgh P, Viersma JH. Enterolith ileus as a complication of jejunal diverticulosis: two case reports and a review of the literature. Dig Surg. 2003; 20 (1): 57-60. [ Links ]
18. W ilhelmi MH, Simanowski J, Aper T, Mlasowsky B, Jung D. Phytobezoars: case report and review of the literature. Zentralbl Chir. 2005 Feb;130(1):77-9. [ Links ]
19. McLaughlin SJ, Jones T. Calcific enterolith perforation: an unusual complication of small bowel anastomosis. Aust N Z J Surg. 1983; 53 (6): 583-5. [ Links ]
20. Karen M, Moralioglu S, Mentes BB. Intestinal perforation due to phytobezoar obstruction: a case report. Acta Chir Belg. 2008 May-Jun;108(3):360-1. [ Links ]
21. Ciçek Y, Ayan F, Carkman S, Gazioglu E, Pekmezci S, Tasçi H. Intestinal perforation due to phytobezoar obstruction. Acta Chir Belg. 1993 May-Jun;93(3):92-3. [ Links ]
22. Ko YT, Lim JH, Lee DH, Yoon Y. Small intestinal phytobezoars: sonographic detection. Abdom Imaging. 1993;18(3):271-3. Related Articles, [ Links ]
23. Yildirim T, Yildirim S, Barutcu O, Oguzkurt L, Noyan T. Small bowel obstruction due to phytobezoar: CT diagnosis. Eur Radiol. 2002 Nov;12(11):2659-61. [ Links ]
Recibido: abril de 2009. Revisado: mayo de 2009. Aceptado: septiembre 19 de 2009
Forma de citar: Hiller HG, Mustafah AH, Lagatolla NR. Terminal ileum perforation secondary to an impacted phytobezoar: case report and review of the literature. Rev CES Med 2009; vol232;55-62