Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
CES Medicina
Print version ISSN 0120-8705
CES Med. vol.29 no.2 Medellín July/Dec. 2015
Reporte de caso
3 cases of cocaine - levamisole syndrome in Medellín
Presentación de tres casos de síndrome cocaína - levamisol en Medellín
JOVANNY GARCÉS-MONTOYA1, MARIE CLAIRE BERROUET-MEJÍA2, MARÍA CAMILA VELÁSQUEZ-ESCOBAR3
1 Emergency Medicine Specialist, Clínica CES, Clínica Cardiovid. Medellín, Colombia.
2 Clinical Toxicologist at Hospital General de Medellín and Clínica SOMA. Teacher Universidad CES, Medellín, Colombia.
3 ER Physician at Clínica CES. Medellín, Colombia.
Forma de citar: Garcés-Montoya J, Berrouet-Mejía MC, Velásquez-Escobar MC. 3 Cases of cocaine - levamisole syndrome in Medellín. Rev CES Med 2015;29(2): 295-304
RESUMEN
El levamisol es un antihelmíntico de uso veterinario que ha sido utilizado como aditivo a la cocaína con el objetivo de aumentar los efectos psicotrópicos de dicha sustancia. Esta mezcla produce reacciones como agranulocitosis, vasculitis cutánea y modulación del sistema inmune. Solamente el reconocimiento, tratamiento adecuado y la suspensión del consumo de esta sustancia lleva a la desaparición de las lesiones y sugiere fuertemente el diagnóstico. Presentamos tres casos de síndrome cocaína/levamisol en Medellín y una revisión de la literatura con algunos conceptos de esta enfermedad.
PALABRAS CLAVE: Cocaína, Levamisol, Leucopenia, Anticuerpos anti citoplasma de neutrófilos, Agranulocitosis.
ABSTRACT
Levamisole, an anthelmintic veterinary product is known to be used as an additive to cocaine that enhances the psychotropic effects of this substance. This mixture leads to reactions such as agranulocytosis, skin vasculitis and modulation of the immune system. Only the proper recognition, treatment of this entity and discontinuation of this substance consumption, leads to the disappearance of lesions; strongly suggesting the diagnosis. We present three cases of cocaine/levamisole syndrome in the city of Medellin and a review of the literature with some concepts related to this pathology.
KEY WORDS: Cocaine, Levamisole, Leukopenia, Antineutrophil cytoplasmic antibodies, Agranulocytosis.
INTRODUCTION
Adulteration of cocaine with levamisole is an up growing problem. The neurostimulating properties of levamisole enhance the euphoric effects of cocaine, making it an attractive option for drug traffickers (1,2).
The main issue with this adulteration is due to the immunomodulating and immunostimulating effects of levamisole, associating it significantly to agranulocytosis and vasculitis, with skin lesions that are self-limiting when the substance use is stopped (2,3).
We present three case reports of patients who presented with a compatible cocaine - levamisole syndrome in the city of Medellín. These cases warn about the presence of adulterated cocaine circulating illegally in the city, something that is not far from what it is reported in the world literature (3).
Case 1
30 year old white male who presented to the emergency room because the appearance of a lesion in the left lower limb, ulcerated, with irregular edges, painful and with a necrotic center; the patient also complaint of subjective fever, asthenia and adynamia.
While reviewing the patient´s past medical history we discovered that he was a cocaine user since the age of 14, initially using 20 grams a day and subsequently it went down to 2 grams a day with periods of cessation of up to two months.
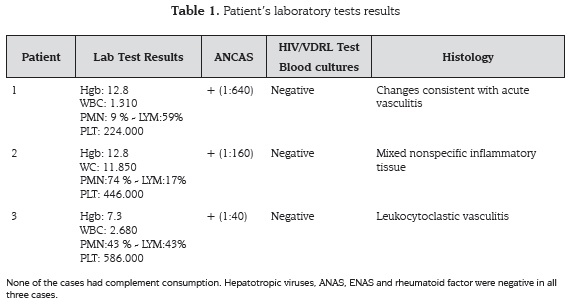
Initially we took a blood sample which showed an important leukopenia (table 1), therefore it was decided to admit the patient to perform more studies and rule out infectious, hematologic or rheumatologic causes. As positive founds we discovered a positive test for lupus anticoagulant and P-ANCA (Perinuclear Anti-Neutrophil Cytoplasmic Antibodies) of 1:640.
A skin biopsy was performed which showed changes consistent with acute vasculitis and an initial diagnosis of antiphospholipid syndrome was made initiating anticoagulation therapy.
During his hospital stay, the patient improved drastically without a specific treatment and with the remainder workup without any significant finds. The above, plus the history of cocaine use and improvement due to the withdrawal of the substance made us suspect the diagnosis of cocaine-levamisole syndrome. The patient was discharged and out-patient studies were performed.
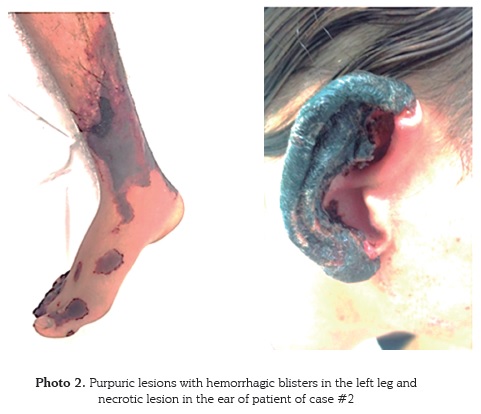
Nine months after he initially presented to the emergency room, the patient relapses on his cocaine use, with the appearance of a new ulcer on his left lower limb, with irregular edges, painful, with a clean background (photo 1) and leukopenia associated. With these findings he is again admitted to the hospital. Infectious and rheumatologic workup is done, once again PANCAS are positive (1:610) but the remainder of the studies showed no abnormality.
The relationship between the use of cocaine and the onset of this ulcerative lesion for the second time, plus a positive P-ANCA value without any other laboratory abnormalities, strongly suggests the diagnosis of cocaine-levamisole syndrome.
Case 2
27 year old Hispanic male who presented to the emergency room because the onset of purpuric lesions in both legs, the lesions were painful, non-ulcerated that became blister and bled with microtrauma. After the appearance of the lesions, the patient began with necrosis on both ears, which were not painful and were not associated to trauma (photo 2). The patient also referred painless cervical lymphadenopathy predominantly, arthralgias and malaise.
Reviewing the patient´s past medical history, it was discovered the current use of inhale cocaine and tetrahydrocannabinol since the age of 16 with a frequency of 3 - 4 cigars per day and 1 - 2 grams per day of cocaine in the last year.
The patient was admitted to the hospital, undergoing an infectious, hematologic and rheumatologic workup. Leukopenia was not found unlike the other two cases (table 1), but P-ANCAS were positive (1:610).
Skin and cervical lymph node biopsies were performed to try to clarify the diagnosis. Skin biopsy reported pseudovasculitis with coagulopathy and thrombosis of vessels. Lymph node biopsy was negative for malignancy (“diffuse inflammatory tissue”). Given that the patient improved with the withdrawal of cocaine use during his hospital stay and in the absence of other pathologic findings a diagnosis of pseudovasculitis due to cocaine-levamisole is made.
Case 3
31 year old Hispanic female who presented to the emergency room with a 15 day onset of a lesion in her right gluteus, ulcerated, painful, purpuric, measuring 3 x 4 centimeters approximately, and another one in the proximal right thigh, also purpuric, painful, non-ulcerated and with irregular edges (Photo 3).
The patient referred use of inhale cocaine up to five grams three times per week for the last two years, with prior intermittent use of 1 gram since the age of 20.
At the time she was admitted for inpatient treatment, leukopenia and microcytic anemia were found (Table 1), without any kind of blood loss or constitutionals symptoms. Once again blood test were run to rule out infectious, immunological or hematological causes. Given that initially the patient presents with bicytopenia, unlike the other two cases, complementary studies were performed like superior digestive endoscopy, colonoscopy, computed tomography of the abdomen, thorax, and brain; without finding any abnormality. The only positive result was a P-ANCA value of 1:40 (Table 1).
Just like the previous patients, a skin biopsy was performed showing ulcers with a nonspecific inflammatory process. IV steroid treatment was begun without any significant improvement, so it was decided to perform a second skin biopsy, this time showing leukocytoclastic vasculitis. The lesions resolve in 15 days despite the suspension of steroids.
Given the lack of improvement with steroids, immune profile with P-ANCA positive, no evidence of infectious disease and improvement with the withdrawal of cocaine use, a diagnosis of cocaine - levamisole syndrome is made. Eight months after discharge, the patient relapses in cocaine use, and again presents to the emergency room with lesions in her lower limbs, with the same characteristics, requiring to be re-admitted to the hospital with improvement of her symptoms with the cessation of cocaine use.
DISCUSSION
Cocaine - Levamisole synergism
Cocaine use is a major social problem, all around the globe the abuse of this alkaloid still occupies the top five places on the use of illicit drugs (1). Added to the problem of consumption, today different forms of manipulation or alteration the alkaloid composition are known, and among these, adulteration consisting of the voluntary addition of an active substance which reduces the purity of alkaloid without the user knowing (2).
The addition of levamisole as a cocaine adulterant has been reported in the literature since 2001. This contamination has grown at such an alarming rate, that in July 2009, the Drug Enforcement Administration (DEA) reported that 69% of the cocaine seized in the United States contained levamisole (3). Although we have no local reports on confiscations of cocaine contaminated with levamisole, the report of the three previous cases, alerts us of the presence of this substance in our environment.
Levamisole is a synthetic derivative of imidazothiazole used as veterinary anthelmintic medication for its stimulant properties on the acetylcholine receptor (4). In the 70’s its immunomodulatory and anti-inflammatory properties were discovered, therefore it was used in the treatment of rheumatoid arthritis and as an adjunct therapy with 5-fluorouracil in the treatment of colon cancer. However, because the occurrence of severe adverse effects such as agranulocytosis, it was withdrawal from the market (5).
Levamisole is a selective inhibitor of monoamine oxidase (MAO); inhibiting norepinephrine and biogenic amines degradation. This effect, in addition to catecholamine reuptake inhibition produced by cocaine or its derivatives, generates a potentiation synergism, that is used for the adulteration of this substance (6,7).
Besides this mechanism, levamisole has effects on nicotinic acetylcholine receptors in the central nervous system, which enhances the euphoric effect of cocaine; also it works in dopaminergic and glutamatergic receptors, stimulating the mesolimbic neurons, increasing the pleasant effects and acting in the reward system involved in the abuse of psychoactive substances (7,8).
Another metabolite found in the degradation process of levamisole is aminorex; an anorectic substance considered to be an “amphetaminelike” molecule, with effects on the monoamine transporter, favoring the stimulant action of cocaine (9).
Despite the use of levamisole as a cocaine adulterant to obtain the effects described above, detection of the substance for diagnostic purposes, it’s not cost effective, since levamisole has a very short half-life (only 5.2 hours), which hampers its detection, also the availability of the test in our country is very limited (10). Having said this, the diagnosis of our three patients was performed based on the signs and symptoms suggestive of the disease and performing laboratory tests that excluded other possible causes.
Cocaine - levamisole syndrome
This syndrome is characterized by the appearance of cutaneous lesions, vasculopathy, and reversible agranulocytosis and inflammatory leukoencephalopathy. Characteristically, there is a significant clinical improvement with stopping the use of the substance (11), as we have seen in our patients, and the reappearance of cutaneous vasculopathy with new consumer exposure (cases 1 and 3) was demonstrated.
For its similarity to other hematologic and rheumatology diseases, the vast majority of patients require multiple diagnostic tests for proper clinical approach (11-13). Larocque and Hoffman (13) made a compilation of 203 cases of levamisole contaminated cocaine users, describing as main findings: neutropenia (69% of cases) and skin lesions (41.3% of cases), information that correlates with the cases presented in this report, except for patient #2. The authors also describe the appearance of symptoms such as malaise and arthralgia in up to 16.7% of cases, especially at the beginning of the picture, as evidenced in patient #2.
Clinical effects produced by the cocaine - levamisole alteration
Cutaneous vasculopathy
Different types of skin eruptions have been reported, the most common include: lichenoid eruptions and cutaneous vasculitis, characterized by the appearance of purpuric plaques and painful hemorrhagic blisters, that suddenly appear anywhere on the body, but with predilection for the lower extremities , nose and ears, as those present in patient # 2 (12,14). The lesions may progress to necrosis or ulcerate and complicate with superinfection by germs commonly present in the skin.
The most common findings in skin biopsy are isolated thrombotic vasculopathy, leukocytoclastic vasculitis and mixed signs of vasculitis and thrombosis, findings that were common in our cases, with improvement of symptoms when removing the substance use (12,14).
Agranulocytosis and immunological profile
As a frequent finding in these patients, agranulocytosis has been found, predominantly leucopenia and neutropenia with variable counts from 0 to 3000 mm3 leukocytes (5). This finding may or may not be associated with cutaneous vasculopathy, reporting the presence of both findings in 47.6% of cases (11,13). In patients # 1 and # 3 leukopenia was found, with white blood cells counts below 3000 mm3 associated with the presence of cutaneous vasculopathy.
One of the postulated mechanisms for developing this type of toxicity is the presence of 6-fenyl imidazole-2,3-dihydroxy (2,1-b) thiazole; one of the three products of levamisole metabolism, with direct effects on leukocytes production (15). Bone marrow biopsy may reveal hypercellularity with relative myeloid hypoplasia with or without megakaryocytic hyperplasia (16).
From an immunological point of view, both the vasculopathy and the leukopenia, have been associated with the appearance neutrophil cytoplasmic antibodies (ANCA’s), as well as the appearance of antiphospholipid antibodies with or without developing the clinical syndrome.
The characteristic feature is the presence of positive titers of p-ANCA’s, which were present in all three patients with negative ANA’s titers. Because the immunological profile, the differential diagnoses most frequently associated with this disease are polyangiitis, Churg-Strauss syndrome and Wegener’s granulomatosis (10, 17,18).
A genetic susceptibility has been suggested in patients with positive HLA B 27 (11). The development of these antibodies is due to long term exposure to this toxic, therefore its appearance is not expected with acute consumption. Just like the skin vasculopathy, it’s been described normalization of the antibodies in a period of 2 to 14 months after cessation of consumption (17).
Leukoencephalopathy
The appearance of reversible inflammatory multifocal leukoencephalopathy has also been described, embracing different neurological findings, from ataxia and dysphagia to hemiparesis and quadriplegia. As with other complications, the vast majority of the symptoms improved with the cessation of consumption, which is suggestive of this diagnosis; however, a very good response to steroid treatment has also been described. In our series, none of the patients had neurological symptoms that were suggestive of this complication during the follow-up (13, 19).
Other symptoms
With a lower frequency of occurrence, the adulteration of cocaine with levamisole has been associated with the onset of joint pain, fatigue and malaise, as occurred in patient #2, which can complicate the diagnosis because of its similitude with multiple diseases, including cocaine withdrawal, especially in the absence of cutaneous vascular disease (20).
Febrile episodes with pathological evidence of histamine release, degranulation of mast cells and deposits of IgG and C3 at the dermal-epidermal junction suggest that levamisole can trigger hypersensitivity reactions type I and type III (21).
Less frequently, but also have been described: focal pauci-immune necrotizing renal failure, pulmonary hemorrhage and hyponatremia; the pathophysiological mechanism involved is not yet known, but it may be related to a possible immune relationship by levamisole´s immunomodulatory effects described above (4, 22).
CONCLUSSION
Cocaine adulteration with levamisole, just as in international reports, is present in our city. The potentiating effect of levamisole in cocaine is a great attraction for traffickers. Cutaneous vasculopathy and neutropenia are the most frequently reported complications in the literature; however, we must always question the patient about the use of these substances, since they may have other life-threatening complications and recurrence of the symptoms and findings is evidenced by repeated exposure to the substance, as we saw in our three patients.
Because in this publication we don´t present personal information, this compilation of three cases was exempt from the ethics committee review.
BIBLIOGRAPHY
1. United Nations Office on Drugs and Crime. UNODC. World Drug Report 2014, V.14-03603. [Visited February 2015]. Available in: http://www.unodc.org/documents/wrd2014/V1403603. [ Links ]
2. Shannon M. Clinical toxicity of cocaine adulterants. Ann Emerg Med 1988; 17:1243- 1247. [ Links ]
3. Casale JF Corbeil EM, Patrick AH. Identification of levamisole impurities found in illicit cocaine exhibits. Microgram J. 2008; 6(3-4):82-89. [ Links ]
4. Lee KC, Ladizinski B and Federman DG. Complications associated with use of levamisole-contaminated cocaine: An emerging public health challenge. Mayo Clin Proc. 2012; 87(6):581-586. [ Links ]
5. Raber H, Takacs L, Vedrody K. Agranulocytosis due to levamisole. Lancet 1976; 2:1248. [ Links ]
6. Sahah KK, Gulati OD, Hemavathi KG. Investigation of some effects of levamisole on dog blood pressure. Indian J Physiol Pharmacol 1986; 30:55 - 62. [ Links ]
7. Raymon LP, Isenschmid DS. Letter to the editor: The possible role 124. Of levamisole in illicit cocaine preparations. J Anal Toxicol 2009; 33:620 - 622. [ Links ]
8. Hernando G, Bergé I, Rayes D, Bouzat C. Contribution of subunits to Caenorhabditis elegans levamisole-sensitive nicotinic receptor function. Mol. Pharmacol. 2012; 82: 550-560. [ Links ]
9. Lapachinske SF, Okai GG, Dos Santos A and et al. Analysis of cocaine and its adulterants in drugs for international trafficking seized by the Brazilian Federal Police. Forensic Sci Int. 2015 Feb; 247: 48-53. [ Links ]
10. Shea J L. Bioanalytical methods for quantitation of levamisole, a widespread cocaine adulterant. Clin Chem Lab Med 2013; 51(1):205-212. [ Links ]
11. Buchanan J A, Lavonas E J. Agranulocytosis and other consequences due to use of illicit cocaine contaminated with levamisole. Curr Opin Hematol 2012, 19:27-31. [ Links ]
12. Ching JA, Smith DJ Jr. Levamisole-induced necrosis of skin, soft tissue, and bone: case report and review of literature. J Burn Care Res 2012; 33:1-5. [ Links ]
13. Larocque A, Hoffman R. Levamisole in cocaine: Unexpected news from an old acquaintance. Clinical Toxicology (2012); 50:231-241. [ Links ]
14. Chung C, Tumeh P, Birnbaum R, Tan BH, Sharp L, McCoy E, and et al. Characteristic purpura of the ears, vasculitis, and neutropenia potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol 2011;65: 722-5. [ Links ]
15. Czuchlewski DR1, Brackney M, Ewers C, Manna J, Fekrazad MH, Martinez A, Nolte KB, Hjelle B, Rabinowitz I, Curtis BR, McFarland JG, Baumbach J, Foucar K. Clinicopathologic features of agranulocytosis in the setting of levamisole-tainted cocaine. Am J Clin Pathol. 2010 Mar;133(3): 466-72. [ Links ]
16. Buchanan JA1, Oyer RJ, Patel NR, Jacquet GA, Bornikova L, Thienelt C, Shriver DA, Shockley LW, Wilson ML, Hurlbut KM, Lavonas EJ. A confirmed case of agranulocytosis after use of cocaine contaminated with levamisole. J Med Toxicol. 2010 Jun;6(2):160-4. [ Links ]
17. McGrath MM, Isakova T, Rennke HG, Mottola AM, Laliberte KA, Niles JL. Contaminated cocaine and antineutrophil cytoplasmic antibody-associated disease. Clin J Am Soc Nephrol 2011; 6:2799-2805. [ Links ]
18. Walsh NM, Green PJ, Burlingame RW, Pasternak S, Hanly JG. Cocaine-related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol 2010; 37:1212-1219. [ Links ]
19. Wu VC, Huang JW, Lien HC, Hsieh ST, Liu HM, Yang CC, et al. Levamisole-induced multifocal inflammatory leukoencephalopathy: clinical characteristics, outcome, and impact of treatment in 31 patients. Medicine 2006; 85:203 - 213. [ Links ]
20. Lee KC, Culpepper K, Kessler M. Levamisole-induced thrombosis: literatura review and pertinent laboratory findings. J Am Acad Dermatol. 2011; 65(4): 128-129. [ Links ]
21. Cristiansen FT, Ng KC, Zilko PJ, Dawkins RL. Levamisole-induced hypersensitivity. Lancet 1977; 1:1112. [ Links ]
22. Friend K, Milone C, Perrone J. Hyponatremia Associated with Levamisole-adulterated cocaine use in emergency department patients. Ann Emerg Med. 2012; 60: 94-96. [ Links ]