Introduction
American Tegumentary Leishmaniasis (ATL) is an infectious disease caused by parasites of the genus Leishmania, which is transmitted in the New World through the bite of the females of sandflies belonging to the genus Lutzomya1. This disease has a diverse clinical presentation that can include a wide spectrum of cutaneous manifestations, ranging from localized to diffuse and disseminated cutaneous forms. In some individuals, ATL can compromise the mucous membranes of the oral cavity and the upper respiratory tract 2.
The epidemiology of ATL is between 600,000 and 1 Million annual cases reported worldwide 3. Less than 10% of these cases correspond to mucosal or mucocutaneous forms, which are usually reported in South America 4. The objective of this paper is to describe three rare cases of ATL treated at a tropical disease research center in Medellin, Colombia.
Case one
A 68-year-old male without a history of skin lesions or a previous episode of ATL. His chief complaint was nasal congestion and rhinorrhea beginning 5 years ago and progressively worsening. These symptoms were associated with epistaxis, edema, inflammation at the malar level, and perforation of the nasal septum.
Physical examination revealed no previous lesions or scars associated with cutaneous leishmaniasis. However, we observed bilateral malar erythema, thickening, hyperemia, drooping of the tip of the nose (tapir nose), inflammation of the nasal mucosa, as well as perforation, and destruction of the nasal septum. Therefore, these clinical manifestations were considered possible mucosal leishmaniasis and further testing was conducted.
The paraclinical tests that were carried out were 1a parasitological exam that was negative for Leishmania amastigotes;2a Montenegro test resulting in a positive report (25 mm); and (3) an RT-qPCR (Real Time-Polymerase Chain Reaction) amplification of the genetic material of Leishmania spp (Ct 20.76, indicative of abundant target nucleic acid). The patient underwent pharmacologic management with N-methyl-glucamine on a dose of 20 mg /kg/day for 28 days. Paraclinical on the seventh day during treatment showed an increase in pancreatic enzymes above five times their normal range. For this reason, N-methyl-glucamine was suspended and the patient was treated with ambulatory oralmiltefosine 2.5 mg/kg/day (Impavido 50 mg capsulesevery 8 hours) for 28 days. This treatment was adequately tolerated and the patient had a substantial reduction in edema and erythema at the easy level and in the nasal mucosa. (Figure 1 A-E).

Figure 1 A-E . (A-D) Day 0 (Before treatment): Bilateral malar erythema, thickening, hyperemia, drooping of the tip of the nose (tapir nose), inflammation of the nasal mucosa, perforation, and destruction of the nasal septum. (C-D) Treatment Day 28: A substantial reduction in edema and erythema can be seen at the easy level and the nasal mucosa.
Case two
A 43-year-old male presented with the chief complaint of two skin lesions in the genital area. The patient reported that the lesions were present for at least one month. The patient previously had non-treated cutaneous leishmaniasis while he was an active Colombian army soldier in 1998. Physical examination revealed two skin lesions in the genital area, with the first lesion in the left inguinal region (25x15 mm) and the second lesion at the level of the foreskin (15x8 mm). The direct examination using Giemsa-stained showed Leishmania amastigotes. Pharmacologic management of the patient was N-methyl-glucamine at a dose of 20 mg /kg/day for 20 days. Fifteen days after starting treatment, the lesions were healed and completed scarred. (Figure 2 A-G).
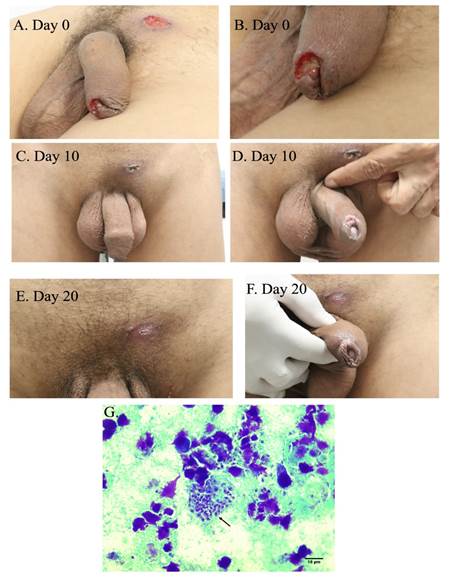
Figure 2 A-G (A-B) Day 0 (before treatment): Two skin lesions were present in the genital area. The first lesion in the left inguinal region measured (25x15 mm) and the second lesion at the level of the foreskin measured (15x8 mm). (C-D) At Day 10, the wound healing and scarring can be seen to be well underway. (E-F) At Day 20, the lesions were healed and completed scarred over. (G) Parasitological examen direct (Giemsa stain) that shows Leishmania amastigotes.
Case three
A 27-year-old male presented with the chief complaint of an erythematous papular lesion, similar to "wheal", located in the right mandibular region. The patient recalled in November 2021 a trip to Peru (Machu Picchu and the Tambopata National Reserve in Puerto Maldonado, region of Madre de Dios) and developed the lesion one month later (12/17/2021). The lesion progressively increased in size, with subsequent ulceration and formation of a thick meliceric crust, with raised edges (5x20 mm) associated to seropurulent secretion, pruritus, and non-painful adenopathies, located in the submental region and the right cervical region, without systemic symptoms.
In Panama City the patient was evaluated by Dermatology and Infectiology, where they performed a biopsy of the lesion a perform a PCR, and culture, these tests were positive for Leishmania spp. (03/04/2022). For this reason, the patient was diagnosed with cutaneous leishmaniasis and treated with N-methyl-glucamine using 15 cc daily for 20 days (02/25/2022 to 03/17/2022). However, 15 days post-treatment, the patient had a clinical relapse of his lesions, for which was a PCR-RFLP (PCR- Restriction fragment length polymorphism) was sought and identified the Leishmania species responsible for the infection as Leishmania brasiliensis (04/15/2022). The patient was managed with Amphotericin B deoxycholate 40 mg via IV intermittently for 26 days due to drug intolerance. The patient’s cutaneous lesions did not improve after the Amphotericin B deoxycholate treatment.
For this reason, the patient consulted at our institution where we observed that the meliceric crust not only included the submental region but also compromised the lower lip. The parasitological exam did not show Leishmania amastigotes. However, RT-qPCR of tissue from these lesions returned positive for Leishmania spp (Ct 17.32, indicating a abundant target nucleic acid). The patient was diagnosed with mucocutaneous leishmaniasis and received liposomal Amphotericin B at a dose of 3 mg /kg/day (240 mg daily) for 15 days. At the end of the treatment, there was an improvement in the patient’s mucocutaneous lesions and disappearance of meliceric crusted lesions and cervical and submandibular adenopathies. (Figure 3 A-E).
Discussion
American Tegumentary Leishmaniasis (ATL) is an underestimated and complex disease with a wide clinical spectrum that includes cutaneous, mucocutaneous, and mucosal forms 5. The clinical presentations of leishmaniasis are a consequence mainly of the host's immune response against this parasite 6. Regarding the cases that we described of mucocutaneous and mucosal leishmaniasis is important to mention that these clinical forms are related to a hyperergic immune response in the host associated with two effector immune patterns such as Th1 and Th17, which induce a greater release of proinflammatory cytokines (TNF-α, IFN-γ, Il-17) that limit the spread of Leishmania6. However, chronic release of these inflammatory mediators can induce inflammation and damage to the tissue. Mucocutaneous or mucosal leishmaniasis are oligoparasitic forms where the visualization of the parasite could not be carried out through a direct examination and the confirmation of the diagnosis requires molecular techniques (PCR), histopathological study, or culture for Leishmania spp7.
Another important point to discuss is the locations of the lesions. Under some occasions, these appear in areas not exposed to the vector of Leishmania. In one of our cases, the cutaneous lesions appeared in an infrequent area such as the genital area. The lesions in the genital area could be the consequence of direct sandfly bites in this area or hematogenous spread of the parasite in patients with untreated cutaneous leishmaniasis 8. Therefore, in endemic areas of leishmaniasis, the differential diagnosis for genital ulcers should include this disease mainly in patients with a previous history of cutaneous leishmaniasis 8. On the other hand, mucocutaneous leishmaniasis in the lip is very uncommon. In the case series described by Mohammadpour 9, this leishmaniasis form may result from direct extension of nearby skin lesions, as occurred in case three, or from hematogenous or lymphatic dissemination ofLeishmaniaamastigotes from the skin. Lip involvement for leishmaniasis in the New World is related mainly to L. Brasiliensis, which was the species identified in our patient 10.
The first-line treatment for this disease has been, for more than 70 years, pentavalent antimony salts such as sodium stibogluconate and N-methyl glucamine antimonate and the cure rate of these antimonial salts for ATL is still high (75%) 11. However, these drugs can cause cardiac, hepatic, renal, and pancreatic toxicity, mainly in older adults 12. In cases of toxicity to antimony salts, the alternative treatment is miltefosine, which is an analog of phosphatidylcholine and has shown a wide cure rate from 53% to 91% 13. While miltefosine is approved for the treatment of ATL in Colombia, there continue to be questions and evidence gaps about the efficacy of this treatment against some Leishmania species mainly related to L. Brasiliensis complex 14. For this reason, in some counties such as Brazil and Peru, where L. brasiliensis is one of the main species causing this infection, guidelines for the management of ATL do not include miltefosine as a therapeutic option for this infection 15. Therefore, the use of other drugs such as liposomal amphotericin B, which has an efficacy of 93% and a good safety profile, would be a better option for ATL treatment than antimonial salts and miltefosine 16. However, the high cost of liposomal amphotericin B limits its use for ATL treatment in the Americas.
While ATL is a neglected disease that is prevalent in some tropical counties, this infection remains unknown to a large number of health workers. Lack of awareness carries consequences for the health of the patients including multiple unnecessary treatments, resistance of antibiotics therapy, and late diagnosis leading to psychological, social, and economics problems. The description of these ATL cases visualizes this disease and shows that joint work between researchers, government entities, and the pharmaceutical industry is required to allow us to take a step towards true control of this disease.
















