Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Acta Neurológica Colombiana
versión impresa ISSN 0120-8748
Acta Neurol Colomb. vol.26 no.4 Bogotá oct./dic. 2010
Atypical acute inflammatory demyelinating polyneuropathy in the setting of HIV infection: Report of two cases
Polineuropatia desmielinizante aguda en SIDA: presentación de dos casos
Francisco Bernal-Cano, MD; Jorge O Suárez, MD MSc; Carlos A Álvarez, MD MSc Ellen Lowenstein, MD; Sandra L Valderrama,
MD; Carlos H Gómez, M.D; Jose R Tamara, MD. Affiliation: Hospital Universitario de San Ignacio Division of Infectious Diseases.Correo electrónico: bernal.f@javeriana.edu.co
Recibido: 14/07/10. Revisado: 14/07/10. Aceptado: 30/07/10.
SUMMARY
Acute inflammatory demyelinating polyneuropathy AIDP is an immune mediated disorder that affects the peripheral nerve reflected in myelin damage and sometimes in axonal loss. Upper respiratory infection, gas- trointestinal infection or nonspecific febrile processes are clinical entities that usually precede neurological symptoms represented by progressive weakness of the extremities and attenuation of tendinous reflexes. In the setting of HIV infection AIDP is a peripheral nerve disorder that usually occurs shortly after seroconversion when the CD4 count is higher than 500 cells/µl. It is presumed to be immune mediated, although the offending antibody has not been identified yet. We report two clinical cases of atypical AIDP in the setting of HIV infection: The first with a T lymphocyte CD4 count lower than 100 cells /µl and the second in context of immunologic reconstitution inflammatory syndrome IRIS. Both entities are uncommon phenomena. The patients recovered satisfactorily after receiving intravenous immunoglobulin and temporary cessation of antiretroviral therapy respectively.
KEY WORDS. HIV, Polyneuropathies.
RESUMEN
La polineuropatia desmielinizante aguda (AIDP) es un desorden inmune que afecta el nervio periférico produciendo lesión axonal o mielínica. las infecciones respiratorias altas, gastrointestinales o los cuadros febriles inespecíficos usualmente preceden este caudro clínico caracterizado por debilidad progresiva y disminución de reflejos miotendinosos. En el paciente con infección VIH la AIDP usulamnete aparece en el periodo de seroconversión cuando el conteo de CD4 es mayor a 500 células/uL. Se presume origen infecciosos a pesar de no existir un anticuerpo específico. reportamos dos casos de paciente con VIH y ADPI con resentación atípica. El primero con un conteo de CD4 menos a 100 células/uL, el segundo en el contexto de síndrome de reconstitución inmunológica (IRIS). Ambos pacientes tuvieron recuperación satisfactoria luego de tratamiento con inmunoglobulina intravenosa y suspensión temporal del tratamiento antiretroviral respectivamente.
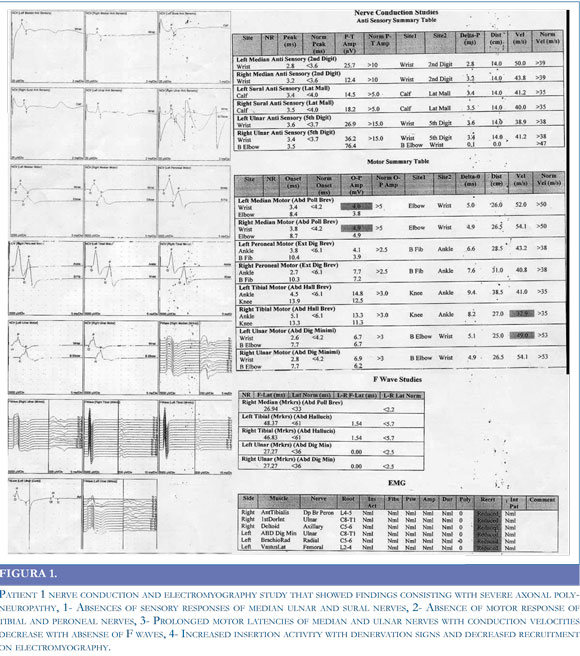
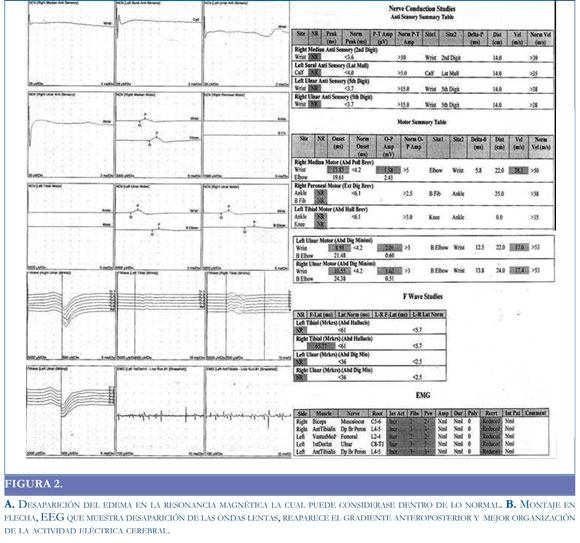
PALABRAS CLAVES. Síndrome de inmunodeficiencia adquirida, Polineuropatias. Case reports A 37 year old male diagnosed with human immunodeficiency virus (HIV) infection in september 2008 whose initial T lymphocyte CD4 count was 20 cells/µl on antiretroviral therapy with zidovudine, lamivudine and nevirapine started on mid october, presented in early february 2009 with a one week history of rapid progressive strength and sensory loss on lower extremities with further involvement of both hands. On admission to the hospital the neurological examination disclosed proximal and distal reduced strength which Medical Research Council (MRC) score was 3/5. In addition, tendinous reflexes were absent and severe sensory loss for all modalities was noted on stocking distribution. By this time his T lymphocyte CD4 count was 46 cells per micro liter and HIV viral load was lower than 40 copies/ ml. Other serum test included complete blood count (CBC), liver enzymes, renal and thyroid profile, vitamin B12, folic acid, lactate and creatin kinase (CK) determinations which results were reported as normal. Cerebrospinal fluid (CSF) analysis showed 0 cells, protein 231 mg/dl and glucose 66mg/dl. Cultures for bacteria, fungus and deoxyribonucleic acid (DNA) polymerase chain reaction (PCR) for cytomegalovirus (CMV) varicella zoster virus (VZV) and tuberculosis were negative. Additionally CSF venereal disease research laboratory (VDRL) was non reactive and CSF HIV viral load was lower than 200 copies/ml. A diagnosis of Guillain Barre syndrome was made further supported by nerve conduction study and electromyography of four limbs that demonstrated demyelination with reduced motor conduction velocities and prolonged distal motor latencies. Furthermore F wave responses were markedly reduced and EMG showed reduction in motor unit recruitment. (Figure 1) The patient was commenced on a five-day course of intravenous immunoglobulin (IVIG) in a dose of 0.4 g/kg body weight a day with no side effects. The patient started improving his neurological condition shortly after completion of IVIG administration, reaching complete recovery following two months. During all this time the patient continued his antiretroviral regimen with no changes. Patient 2 A 46 year old male with HIV infection diagnosed in February 25, 2008 in the setting of P. Jirovecci pneumonia, T lymphocyte CD4 count of 49 cells/µl and HIV viral load higher than 1000000 copies /ml, started antiretroviral therapy with zidovudine, lamivudine and efavirenz in the third week of March 08. He noted one month later a six days history of difficulty to walk due to loss of strength on both lower extremities with no sensory involvement. Other medications included trimethoprim sulfamethoxasole and fluconazol. On admission to the hospital his physical examination only showed mild quadriparesis with absent achillean and patellar reflexes. Workup laboratories included CBC, electrolytes, liver enzymes, renal function, thyroid profile, vitamin B12, folic acid, and lactate, all reported as normal. In addition his most recent T lymphocyte CD4 count was 221 cells/µl and the HIV viral load was lower than 50 copies /ml. CSF analysis showed 1 cell, protein 157 mg/dl and glucose 54 mg/dl, cultures were negative; VDRL non reactive and CMV/VZV DNA detection by PCR was negative. CSF HIV viral load was lower than 200 copies per ml. One week later nerve conduction studies plus EMG of lower extremities were done showing reduced F waves responses and motor conduction velocities. EMG showed only mild reduction in motor unit recruitment (Figure 2). A diagnosis of acute inflammatory demyelinating polyneuropathy (AIDP) in the setting of an immune reconstitution syndrome was made. Because the symptoms were not disabling the patient severely at all, it was decided to continue with his antiretroviral regimen without modification. No further worsening of symptoms was noted by the patient and his neurological examination showed a rapid improvement of the strength one month after starting an intensive program of physical therapy. Currently -June 2009- he has no neurological symptoms.
Patient 1
DISCUSSION
Cell-mediated immunity is known to play an important role in the pathogenesis of GBS. The cha- racteristic initial stage of this entity is associated with demyelinization related to the action of macrophages, with multifocal distribution in the nerves. The main action of T cells appears to be the impairment of the integrity of the blood-nerve barrier by the action of metalloproteinases, in addition to influence the recruitment of other immune cells o such as macrophages, Schwann cells and fibroblasts (1). Acute AIDP is an uncommon disorder in the setting of HIV infection that usually has been seen shortly after seroconversion when the T lymphocyte CD4 count is higher than 500 cells/µl (2), this disorder seems to be immune mediated depending on a possible over activity of T and B lymphocyte cell population. Biopsy and autopsy findings have been contradictory regarding the presence or absence of perivascular lymphocyte infiltration in GBS. The fact that no lymphocytes are detected in nerves suggests that the changes mediated by antibodies are important, in agreement with the pathogenetic mechanism proposed for the onset of GBS, which occurs after infections, as is the case or Campylobacter jejuni which is associated with antibodies to GM1 and GQ1b gangliosides. These gangliosides share epitopes with the lipopolysaccharide coat of some strains of this bacterium (3).
There are few HIV/AIDP cases published in the literature whose CD4 count is lower than 50 cells and co infection especially by cytomegalovirus has been ruled out either by CSF DNA detection by PCR or clinical course.2, 4 The exact mechanism of thiphenomenon is unknown since it could be assumed that patients with not enough T lymphocyte CD4 count are unable to mount a competent immune response. However it is hypothesized that alteration of T cell homeostasis induced lymphopenia could be permissive for the disruption of self tolerance and autoimmune disease may occur in lymphopenic patients (4).
The first case is an example of this scenario which clinical outcome behaved similar to Guillain Barre syndrome in HIV seronegative patients that usually respond to IVIG or lasmapheresis (5). Some authors promote performing plasmapheresis followed by IVIG in the setting of HIV infection but cases where the CD4 count is lower than 100 cells /µl administration of gancyclovir or foscarnet should be considered until CMV polyradiculopathy is excluded (6).
The second case displays an immune reconstitution syndrome (7) that elicited AIDP in context of recent onset of antiretroviral therapy with a CD4 count lower than 100 cells/µl. In this situation an autoimmune disorder can promotes damage of peripheral nerves explained by the role of T cells contributing to the selection of natural self-reactive antibody repertories whose expression of immuoglobulin M (IgM) and immunoglobulin G (IgG) toward some self-antigens depends on the number of T CD4 lymphocytes (8).
The course of HIV is characterised by a decreasing CD4 count and a rising viral load. There is loss of lymphocytes to a level where secondary immune responses are lost to both primary and recall antigens.9 On commencement of HAART viral suppression is sufficient to allow regeneration, by clonal expansion of the remaining clones, of these immune responses.10 This has resulted in an immunological response to self or pathogen, where there was previously anergy, the aptly named immune reconstitution syndrome.11,12. To our knowledge there are no more than 10 case reports published of AIDP associated to immunologic reconstitution inflammatory syndrome (IRIS) in the setting of HIV infection (9-12). Therapeutic approaches include conservative measures, steroids plasmapheresis or temporary suspension of antiretroviral therapy (12).
Acknowledgments
Special thanks are given to to Pontificia Universidad Javeriana school of Medicine, Dr Joe Fernando Muñoz for his clinical work and editorial assistance and Dr Julio Cesar Castellanos, for supporting Infectious Diseases Unit at Hospital Universitario de San Ignacio in Bogota Colombia South America.
REFERENCES:
1. PITHADIA AB, KAKADIA N. Guillain-Barré syndrome (GBS). Pharmacol Rep. 2010; 62: 220-32. [ Links ]
2. BRANNAGAN TH 3RD, ZHOU Y. HIV-associated Guillain-Barre syndrome. J Neurol Sci. 2003: 15; 208: 39-42. [ Links ]
3. QURESHI AI, COOK AA, MISHU H, KREN DEL DA. Guillain- Barre´ syndrome in immunocompromised patients: a report of three patients and review of the literature. Muscle Nerve. 1997; 20: 1002-1007. [ Links ]
4. MISHRA BB, SOMMERS W, KOSKI CL, GREENSTEIN JI. Acute inflammatory demyelinating polyneuropathy in the acquired immune deficiency syndrome. Ann Neurol. 1985; 18: 131-132. [ Links ]
5. KRUPICA JR T, FRY TJ, MACKALL CL. Autoimmunity during lymphopenia: a two-hit model. Clin Immunol. 2006; 2: 121-128. [ Links ]
6. BURNS TM. Guillain-Barre syndrome. Semin Neurol. 2008; 28: 152-67. [ Links ]
7. MARKARIAN Y, WULFF EA, SIMPSON DM. Peripheral neuropathy in HIV disease. AIDS Clin Care. 1998;10:89-91, 93, 98. [ Links ]
8. SHELBURNE SA 3RD, HAMILL RJ. The immune reconstitution inflammatory syndrome. AIDS Rev. 2003; 5: 67-79. [ Links ]
9. STAHL D, LACROIX-DESMAZES S, MISRA N, KARMOCHKINE M, KAVERI SV, COSTAGLIOLA D, ET AL. Alterations of self-reactive antibody repertoires in HIV disease: an insight into the role of T cells in the selection of autoreactive B cells. Immunol Lett. 2005; 99: 198-208. [ Links ]
10. TEO EC, AZWRA A, JONES RL, GAZZARD BG, NELSON M. Guillain--Barre syndrome following immune reconstitution after antiretroviral therapy for primary HIV infection. J HIV Ther. 2007; 12: 62-63. [ Links ]
11. FUJISAKI G, KAMI M, MURASHIGE N, KISHI Y, HORI A, CHIZUKA A. Guillain-Barre syndrome associated with rapid immune reconstitution following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2006; 37: 617-619. [ Links ]
12. PILIERO PJ, FISH DG, PRESTON S, CUNNINGHAM D, KINCHELOW T, SALGO M, ET AL. Guillain-Barré syndrome associated with immune reconstitution. Clin Infect Dis. 2003; 36: e1111-114. [ Links ]