INTRODUCTION
Central Pontine Myelinolysis (CPM) is a demyelinating disease affecting the central pons. It presents in some patients with chronic alcoholism, sodium disturbances and liver transplantation among others conditions 1. Its physiopathology is unknown, although many hypotheses related to osmotic and electrolytic disturbances and effects of immunosuppressant have been settled. Clinical manifestations are mainly motor and consciousness involvement, but other symptoms may be present. The rising number of patients undergoing transplant surgery especially of liver, the complexity of critical patients, the elaborated vital support and the increasing of patients with potent immunosuppressive drugs, are risk factor to CPM and must be considered as potentials factors to increased the incidence of CPM in patients after transplant. Clinical diagnosis requires confirmation through neuroimaging, especially brain Magnetic Resonance (MR). CPM has poor prognosis, therefore prevention and sensitization of medical community are very important. The case of a patient with neurological deterioration after liver transplantation and multiple risk factors is analyzed and reported.
Case presentation
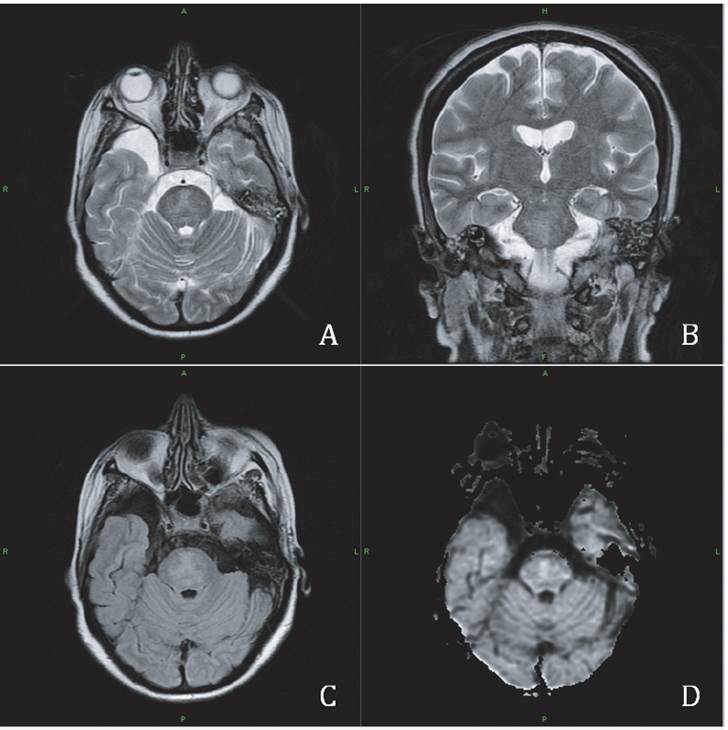
40-year-old female patient hospitalized with diagnosis of biliary cirrhosis secondary to autoimmune hepatitis and chronic hepatic encephalopathy; she had renal failure too. Underwent liver transplantation without any complications. During the first day after surgery the patient had low cardiac output and required inotropic support. At the second day immunosuppression was initiated with tacrolimus 3 mg every 12 hours, inotropic was suspended and the patient was extubated, with a normal awakening, oriented with adequate person to person interaction and fluent language; she was hypokalemic for several days (Fig. 1). At sixth day, the patient became confused with bradypsychia and disorientation. The eighth day after surgery, she had a generalized tonic-clonic seizure, with subsequent normal awareness recovery but bradypsychia and disorientation persisted. Computed Tomography (CT) of the brain was normal. Anticonvulsant treatment with levetiracetam 500 mg every 12 hours was started. As diagnostic possibility of Posterior Reversible Encephalopathy Syndrome (PRES) was considered; that same day tacrolimus serum levels were reported in 30 ng/ ml (NV: 10-15 ng/ml) and it was suspended. The ninth day the patient was drowsy with sodium levels in 149 mmol/L, fluctuating between 147 mmol/L and 156 mmol/L from day 9 to 25 (Figure 1). At day twelfth, the patient was stuporous with hyporesponsive midriatic pupils, hypotonia, generalized hyperreflexia and bilateral Babinski sing. Brain MRI on day thirteenth showed anisohyperintensity, which involved the central pons (Figure 2). The electroencephalography had diffuse slowing and asymmetry of electric activity with greater involvement of the left side, and transient triphasic waves activity in the right parieto-occipital region. The fifteenth day after surgery the patient became comatose; that same day cyclosporine started. The patient persisted in coma, with deconjugated gaze palsy and severe flaccid quadriparesis. At seventeenth day, she had pancreatitis secondary to cyclosporine, and azathioprine was started instead. Liver enzymes were elevated immediately after transplantation (ALT 5666 mU/mL; AST 5692 mU/mL) according to expected, and its levels decreased progressively until twenty-first day, when elevation of serum levels was noticed (ALT 46,5 mU/mL; AST 61 mU/mL). The patient died at thirty-ninth day after transplantation.

Figure 1 Clinical manifestations and variation of sodium, potassium and tacrolimus serum levels over time. Description of the variation through time in serum levels of sodium (Na+), potassium (K+) and tacrolimus. Serum levels are shown in the vertical axis, days after surgery are shown in the horizontal axis. Tacrolimus serum levels are shown independently. Vertical arrows show the clinical manifestations in chronological order.
DISCUSION
CPM was first described in 1932 as post-mortem finding, but just until 1959 Adams described as a demyelinating disorder affecting the central pons, typically malnourished, alcoholic, and chronically debilitated patients. 2. The original description included rapididly evolving quadriplegia, dysarthria, dysphagia, and mutism. Categories at risk of developing demyelinating disorders including septic, burn, diabetic, human immunodeficiency virus, and liver transplanted patients, demonstrated the presence of electrolyte imbalances (especially hyponatremia) and a possible too rapid correction thereof.
CPM represents 50% of the osmotic demyelination syndrome and Extrapontine Mylinolysis (EPM) represents another 25%, and a combination of both, CPM and EPM, the other 25%. General incidence of this entity is unknown, although some post-mortem case series have demonstrated typical lesions in 0,25% of necropsies (9 cases of 3548 necropsies). The general incidence among population is in people between 30-50 years old, especially in those with chronic alcoholism and liver transplant 3.
CPM was first described after liver transplantantation by Starzl et al in 1978. It is ones of the most serious neurologic complications and the incidence varies from 0.94% to 3% in current clinical series, occur within the first week after surgery and in another cohort more than 50% of neurologic symptoms varying from stupor to locked-in syndrome appear within the 7th postoperative day. 4
Neurological complications are a common complication in patients undergoing liver trasplant. In fact, the receptors of LT suffer a more incidence of neurological complications in patients underwent to heart, kidney or lung transplant. The main causes of this complication are pretransplant disease, surgical complications, metabolic disorders and neurotoxicity of immunosuppressive drugs. The average incidence of neurological complications after LT is 30%, with a median time to onset of 7 days. The most severe and frequent symptoms were seizures, which appeared in 72% of cases. It described that neurotoxicity immunosuppressive therapy is the most common cause of seizures after LT.
Studies show an increased incidence of neurotoxicity in patients receiving cyclosporine (27%) was administered compared to those treated with tacrolimus (19%), although the differences were not statistically significant. Described that extrapontine myelinolysis is characteristic of cyclos-porine neurotoxicity, and central pontine myelinolysis are related to sudden changes in serum sodium concentration and hypomagnesemia in patients undergoing to LT, strict sodium levels before and after the transplant control can help reduce the incidence of these complications. 5
CPM mainly affects the basis pontis and sometimes spreads through the lower midbrain as a symmetric central lesion due to the tight linear conformation of the axons and glial cells in the pons, which limits the expansive mechanic axonal flexibility and its way to adapt to hyperosmolar disturbances such as sodium, potassium, myoinositol, taurine and glutamate loss; also limits the storage and transport of glucose, accentuated by a low blood perfusion. EPM locates commonly in cerebellum, lateral geniculated body, external capsule, hippocampus, putamen, thalamus, cerebral cortex and caudate nucleus, as these are areas where many white and grey matter elements are present, and predisposition to greater damage is higher with the release of myelinotoxic substances secondary to osmolality changes 4. In patients with exclusive extra-pontic compromise, pathologies such as Wilson's disease, Wernicke's encephalopathy, Leigh's disease, or carbon monoxide poisoning should be considered 7.
Pedraza and colleagues reported a case of osmotic demyelination syndrome after liver transplantation, with the use of cyclosporine related to white matter lesions and seizures, proposing the neurotoxic effect of cyclosporine as secondary to the energetic mitochondrial metabolism blockage 8. In a case series by Céline Odier and colleagues, 25% of patients CPM after liver transplantation and immunosup-pression with tacrolimus, depression of consciousness was the most frequent clinical manifestation; in these patients a poor prognosis with 100% mortality was reported during the first four months 9. In other case report by Kyota Fukazawa and colleagues, a patient treated with tacrolimus after liver transplantation developed aphasia, apraxia, paraplegia and locked-in syndrome; the author stated several pathogenic hypotheses to explain this association, such as the neurotoxic effect of tacrolimus in the central nervous system, vasoconstriction induced by tacrolimus followed by ischaemia, and intraoperative air embolization 1.
Electrolytic disturbances are also associated with CPM. Abrupt changes in serum sodium levels have been reported as probable causes. Some authors have related rapid correction of hyponatremia with establishment of CPM, especially in patients with liver transplant 1,5. Pathophy-siology suggests that cells conditioned to hyponatremia may have a diminished adaptive capability to osmotic stress leading to significant dehydration of nervous cells with water mobilization into extracellular space, it produces an axonal demyelination secondary to mechanical detachment and posterior necrosis of oligodendroglia 3. Based on this statement some authors set different alternatives for hypo-natremia correction rates, in ranges from 12 mmol/day to 15 mmol/day; others are more conservative and propose 8-10 mmol/day 6. This mechanism could not be the only explanation in the case report, since sodium levels, although very fluctuating (Figure 1), they did not vary more than 7 mmol/day in its correction. On the other hand isolated hypernatremia has also been related to CPM.
Pretransplant high serum sodium levels were independently associated with increased risk of neurological complications. In a case reported by Van der Helm-van Mil and colleagues, a patient admitted with confusion and somnolence during a hunger strike, had hypernatremia with sodium levels of 187 mmol/L and the brain MRI showed lesions consistent with CPM and EPM 10. Chang and colleagues reported a case of a woman who presented EPM secondary to central diabetes insipidus, with consciousness involvement and serum sodium levels in 172 mmol/L, and a brain MRI nine days after admission showed lesions in the cerebral peduncles and splenium of the corpus callosum suggesting EPM. The pathophysiological mechanism in hypernatremia suggests rapid neuronal dehydration caused by hypernatremia which turns into the unraveling of the axonal myelin sheet 11.
Disturbances in potassium levels have also been associated to this entity 12. Sugimoto and colleagues reported a case with a possible association between low serum potassium levels and CPM, other laboratory tests were normal, no history of alcoholism or hepatic disease was found, and potassium levels were in 2,8 mEq/L before hospitalization, reaching a minimum level of 2,5 mEq/L (13). In this reported case, low potassium levels were noted with a minimum of 2,48 mmol/L (Fig 1), which could be possible triggering factor for CPM.
In a recent case report, the relationship between metabolic and electrolytic abnormalities related to CPM was analyzed and hypokalemia was included as independent risk factor for its development 14.
Clinical manifestations include dysarthria, dysphagia and paraparesis or flaccid quadriparesis; pupillary defects, eye movement abnormalities and locked-in syndrome are also observed. Less commonly psychiatric symptoms, ataxia and movement disorders are seen 3. Conscious state varies among stupor and coma 4. In the present case, initial clinical manifestations were seizures with following conscious deterioration, initially thought to be a relatively frequent condition in patients treated with immunosuppressants after transplantation, known as PRES 15.
When the is clinical suspicion of CPM use of neuroi-maging is recommended. CT is less sensitive than MRI, but somethimes it may show a medial pontine hypodensity. MRI is the technique of choice; it shows a symmetric hypoin-tense image in the basis pontis in T1 without tegmentum or ventrolateral pons involvement, and a hyperintense image in T2, protonic density and FLAIR. Knowing that lesions appear days or even weeks after the establishment of the clinical condition is important 1,3. Diffusion imaging is ideal in early diagnosis because it shows increased signal and lesions appear earlier, (16). Head CT in this patient two days after the first neurological symptom was normal, whilst MRI, five days after CT, showed a pontine hyperintensity in T2 (Figure 2).
The first differential diagnosis made in this case was PRES. It characterizes by headache, visual disturbances and seizures; brain imaging suggests asymmetric bilateral subcortical edema in parieto-occipital regions and has favorable prognosis, with regression of edema and imaging normalization in less than 15 days, only with reduction of immunosuppressant dosage 15. This entity should be considered when diagnosing CPM, because of its clinical similarities.
CPM diagnosis has improved with the new imaging methods, even though this process does not necessarily implies a change in prognosis, especially for those patients with liver transplant. In a case series of patients with CPM, signs and symptoms, sodium levels, causes, imaging and outcomes in 12 patients were compared; 50% had hydroelec-trolitic disturbances, 25% had chronic alcoholism and other 25% underwent liver transplantation. The results showed poor prognosis given by death (at four months 33% and three years 16,6%) and permanent cognitive deficit (16,6%); only two patients had minor neurological deficit 9.
Some treatments have been used among them steroids, which regulate the blood brain barrier permeability secondary to hyperosmolarity derived from swift correction of hyponatremia; intravenous immunoglobulin, which reduces myelinotoxic substances and antimyelin antibodies formation; plasmapheresis with a mechanism of action similar to immunoglobulin; with apparent good results 3,6. This evidence corresponds to case reports and case series, hitherto clinical trials have not been performed to determine their efficacy. So far the principal management in patients with risk factors is the slow reposition of sodium, strict sodium levels before and after the transplant control can help reduce the incidence of these complications, in case of patients treated with immunosuppressants, the maintenance of immunosuppressant levels inside the therapeutic range 13,15. Prevention of this pathology has vital importance in patients with chronic alcoholism, malnutrition and immu-nosuppressants intake after liver transplant. In these patients chronic hyponatremic state, other concomitant hydroelec-trolitic disturbances and serum immunosuppressant levels, which in the case of tacrolimus should not exceed 15 ng/ ml, has special importance.
Patients with CPM have several predisposing conditions for this kind of pathologies, and interaction of conditions like malnutrition, metabolic and electrolytic disturbances, hypoperfusion and toxic effect of immunosuppressants can potentiate the risk of developing CPM in patients with liver transplantation.
CONCLUSION
Central pontine myelinolysis is a demyelinating disease with multifactorial origin, where factors such as immuno-suppressants, electrolitic disturbances, comorbidities and health state before transplantation are very important. Its incidence is low within general community, but high in patients with alcoholism, malnutrition and hepatic transplant. Its pathophysiology is still unknown, but some hypotheses exist. Treatment is supportive, although some medications have been used. It is important to stand out that prevention and early clinical suspicion is primordial in patients with risk factors to avoid fatal outcome or permanent disability. We propose these factors as potential tools for identifying high-risk patients, allowing their prompt assessment and treatment to improve morbidity and survival in these patients.