Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
CES Odontología
Print version ISSN 0120-971X
CES odontol. vol.30 no.1 Medellìn Jan./June 2017
Revisión de tema
Clinical aspects of dental fluorosis according to histological features: a Thylstrup Fejerskov Index review
Aspectos clínicos da fluorose dentária de acordo com as características histológicas: revisão do índice Thylstrup Fejerskov
Aspectos clínicos de la fluorosis dental de acuerdo con las características histológicas: una revisión del índice de Thylstrup Fejerskov
Jéssica Patrícia Cavalheiro1, Diego Girotto Bussaneli2, Manuel Restrepo2 Camila Maria Bullio Fragelli3, Rita de Cássia Loiola Cordeiro4, Alfonso Escobar Rojas5 Lourdes Santos-Pinto6, Fabiano Jeremias7
1DDS, MSc, PhD Student, Department of Orthodontics and Pediatric Dentistry, Araraquara School of Dentistry, UNESP - Univ Estadual Paulista, Araraquara/SP, Brazil.
2DDS, MSc, PhD, Professor, School of Dentistry, Department of Pediatric Dentistry, Universidad CES Colombia.
3DDS, MSc, PhDt, Department of Orthodontics and Pediatric Dentistry, Araraquara School of Dentistry, UNESP - Univ Estadual Paulista, Araraquara/SP, Brazil.
4DDS, MSc, PhD, Professor, Department of Orthodontics and Pediatric Dentistry, Araraquara School of Dentistry, UNESP - Univ Estadual Paulista, Araraquara/SP, Brazil.
5HC, Professor, School of Dentistry, Department of Pediatric Dentistry, Universidad CES Colombia.
6DDS, MSc, PhD, Full Professor, Department of Orthodontics and Pediatric Dentistry, Araraquara School of Dentistry, UNESP - Univ Estadual Paulista, Araraquara/SP, Brazil.
7DDS, MSc, PhD, Assistant Professor, Department of Orthodontics and Pediatric Dentistry, Araraquara School of Dentistry, UNESP - Univ Estadual Paulista, Araraquara/SP, Brazil.
Forma de citar: Cavalheiro JP, Girotto-Bussaneli D, Restrepo M, Bullio-Fragelli CM, Loiola-Cordeiro RdC, Escobar-Rojas A, Santos-Pinto L, Jeremias F. Clinical aspects of dental fluorosis according to histological features: a Thylstrup Fejerskov Index review. Rev. CES Odont 2017; 30(1):41-50.
Recibido: enero de 2017. Aceptado: mayo de 2017
Abstract
Dental fluorosis is a developmental defect of enamel caused by chronic and excessive fluoride intake resulting in a hypomineralized enamel with increased porosity. It is clinically identified as spots ranging from mild white lines to opaque spots covering all or part of the enamel surface and breakdown after teeth eruption. However, the clinical definition of the fluorosis degree in teeth is not an easy task, having been presented many indices that generally qualify the severity degree with variations in the details. As the choice of treatment is closely linked to the defect severity, the purpose of this article is to present the clinical aspects of dental fluorosis represented through the Thylstrup-Fejerskov Index. The severity scores are presented according to histological features and the differences between them will be discussed in order to enable the dentist to correctly diagnose and choose the most appropriate treatment for the patient with DF.
Keywords: dental fluorosis; diagnosis; classification.
Resumo
A fluorose dental (FD) é um defeito de desenvolvimento do esmalte causado pela ingestão crônica e excessiva de flúor, resultando em um esmalte hipomineralizado com maior porosidade. Clinicamente é identificada como manchas que vão desde delicadas linhas brancas até manchas opacas que cobrem parte ou toda a superfície do esmalte podendo sofrer pigmentações ou fraturas após a irrupção. No entanto, a definição clínica do grau de comprometimento dos dentes não é uma tarefa fácil e tem sido apresentada na forma de índices que geralmente qualificam o grau de severidade com maior ou menor detalhes. Como a escolha do tratamento está intimamente ligada à gravidade do defeito, o objetivo deste artigo é apresentar os aspectos clínicos da fluorose dental representadas por meios do índice de Thylstrup-Fejerskov (1978). Os escores de severidade são apresentadas de acordo com as características histológicas e as diferenças entre eles serão discutidas a fim de permitir ao dentista diagnosticar corretamente e escolher o tratamento mais adequado para o paciente com FD.
Palabras clave: fluorose dentária; diagnóstico; classificação.
Resumen
La fluorosis dental (FD) es un defecto del desarrollo del esmalte dental causado por la ingesta crónica y excesiva de fluoruro, que resulta en un esmalte hipomineralizado y poroso. Clínicamente se manifiesta desde manchas y delicadas líneas blancas hasta manchas opacas que cubren parte o toda la superficie del esmalte, el cual es susceptible a pigmentaciones o fracturas post-eruptivas. Sin embargo, establecer el grado de compromiso de los dientes no es una tarea fácil y para esto se han presentado índices que determinan el grado de severidad con mayor o menor detalle. Como la decisión de tratamiento está estrechamente relacionada a la gravedad del defecto, el objetivo de este artículo es presentar los aspectos clínicos de la fluorosis dental de acuerdo al índice de Thylstrup-Fejerskov (1978). Los grados de severidad son representados de acuerdo con las características histológicas y las diferencias entre ellos son discutidas para que el odontólogo pueda diagnosticas correctamente y escoger el tratamiento más adecuado para el paciente con FD.
Palabras clave: fluorosis dental; diagnóstico; clasificación.
Introducción
The dental fluorosis (DF) results from chronic and excessive ingestion of fluoride during the period of amelogenesis, resulting in a hypomineralized enamel with varying levels of porosity (1). Clinically, the enamel presents streaks and/or opacities that may vary in color white, yellow or brown (2), and can be accompanied by structural losses (3). The diagnosis of DF is not an easy task for the dentist because clinically the affected enamel is very similar to other conditions found in the clinical practice, as white spots suggestive of incipient carious lesions, non-fluorotics enamel defects, molar-incisor hypomineralization (MIH), amelogenesis imperfecta, dentinogenesis imperfecta and tetracycline stains (4).
Regarding etiology, the most important risk factor for DF is the amount of fluoride consumed in a given period, from several sources (5). The definite evidence that fluoride can induce dental fluorosis by affecting the enamel maturation was given by Richards et al (6). The period of risk for the dental fluorosis development comprises maturation stage of tooth enamel (1,7,8). The fluoride acts on the rates at which enamel matrix protein breakdown or rates at which the byproducts of enamel matrix degradation are withdrawn, resulting in retardation of crystal growth in enamel maturation stage (9). There are several dietary sources of access to fluoride, however, toothpastes and fluoride supplements, in addition to infant formula ingested before seven years of age are the three main risk factors for dental fluorosis, because they can reach excessive levels in the body (7).
It is a fact that fluoride is effective in preventing tooth decay (10), but does not remove the cause of the disease permanently (3). Rather, their action can lead to weakness of the tooth tissue, since the amended structure of enamel is also more susceptible to demineralization (3,11). This may be the possible reason for high caries experience in areas with high concentrations of fluoride (3).
There are a variety of indices described in the literature used in epidemiological studies to classify the DF severity (12). The Thylstrup and Fejerskov index (TF index) is complete and sensitive, because evaluates dental fluorosis in all severity levels (4) correlating clinical features with histological features of the affected enamel (13,14). In their classification has scores ranging from zero to nine, allowing the determination of mild to more severe levels, i.e, higher scores indicate greater severity (12).
In clinical practice, the degree of severity determines the type of treatment that is highly complex (15) due to occurrence of cracks, loss of enamel, hypersensitivity and impairment of masticatory efficiency, and may also affect the patientâs life quality due to the aesthetic standard (16). In this context, the aim of this article is to present the clinical characteristics of dental fluorosis through Thylstrup and Fejerskov Index (1978) (13), enabling the dentist to correct diagnosis and choose the most appropriate treatment for patients with DF.
Clinical characteristics of Dental Fluorosis
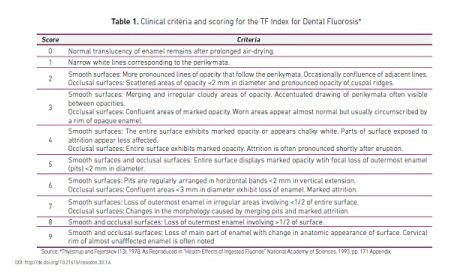
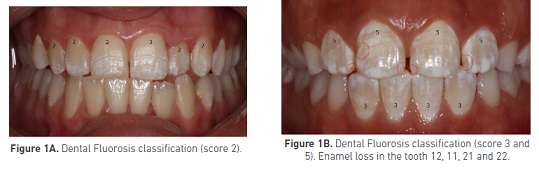
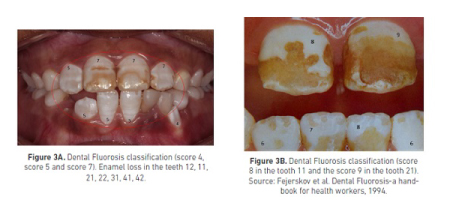
Clinically, the dental fluorosis appearance varies according to its gravity (17). The earliest manifestation of dental fluorosis is an increase in enamel porosity along the striae of Retzius (18). These lines, corresponding to perikymata, may or not be fused, forming white spots with chalk aspect (4,19) (Figure 1A). In more severe cases, such porous areas can acquire a brown color, with the possibility of tooth structure loss due to friable feature of the stained area (20) (Figure 1B - 3B). The table 1 shows the criteria for classification based on biological aspects to the dental fluorosis index proposed by Thylstrup and Fejerskov (13).
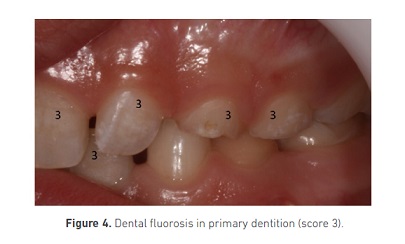
In primary dentition with dental fluorosis (Figure 4), the lesions may also have an asymmetrical pattern, however, the risk of structural loss is smaller, considering that the severity is less when compared to permanent dentition (4). Discussion
The use of fluoride, either systemically or topically, has fostered significant improvements in oral health by reducing dental caries rates (9). However, the undesirable effect of excessive ingestion of fluoride, dental fluorosis (4,21), also has been identified today. As explained above, this enamel defect is characterized by a hypomineralization resulting of the proteins retention in enamel matrix during the early stage of mineralization (22). Clinical manifestations depend on the amount of fluoride ingested, exposure time, age, weight, nutritional status of the individual (23); in addition to the fact that children with weak health and systemic conditions are more likely to present developmental defects of enamel (24).
Among the various sources of fluoride most common, which reach population levels, are the public measures of fluoride addition artificially in drinking water and salt (25). Water fluoridation is effective method preventing tooth decay when used at optimal concentration, according to the local average temperature (26). The temperature factor directly affects the amount of water intake, increasing the fluid intake, especially in tropical areas (27). In Brazil, the concentration recommended to minimize the DF risk is 0.07mg fluoride/day/kg body weight (28). According to Marthaler (29) (2013), the fluoride salt has the same cariostatic potential that fluoridated water; in Germany, about 67 % of the population consume fluoridated salt and in Switzerland, about 85 %. Salt fluoridation schemes are reaching more than one hundred million in Mexico, Colombia, Peru and Cuba. In Latin America, there are more than 100 million users, and several countries have arrived at coverage of 90 to 99 %. Salt fluoridation is by far the cheapest method of caries prevention, and billions of people throughout the world could benefit from this method.
The TF index allows carefully classify the affected tooth, by correlating clinical and histological aspects (13,14) and avoid underestimating the real pattern of severity of the affected tooth, which could compromise the effectiveness of established treatment. As noted in the cases illustrated in this article, the DF does not always present a symmetrical pattern. This uneven occurrence of the enamel defect, in a dentition as a whole, suggests that ameloblasts are affected in a very specific stage of development, being that not all of them are capable to repair against an insult; and as a result, is observed opaque areas in dental enamel, characterized by mineral deficiency (30).
While in the permanent dentition, the teeth may appear completely stained (Figures 1B â 3A) and even with structural loss (Figure 3B), in the primary dentition, mildest levels of hypomineralization are observed (Figure 4). These differences between dentition are due to the fact that the mineralization phase of deciduous teeth is smaller than that of the permanent teeth (31), besides having smaller enamel thickness and featured whitish color, which difficult the detection of fluorosis in milder degrees (32). Furthermore, the mineralization of deciduous teeth occurs before birth. Thus, the placenta functions as a passive barrier against the passage of high fluoride concentrations from maternal plasma to the fetus (33).
In clinical practice, the diagnosis of DF can be even more challenging since there are enamel defects that may be confused. Thus, the clinician must establish the differential diagnosis for the following defects: non-fluorotics enamel defects, white spots suggestive of incipient carious lesions, molar-incisor hypomineralization (MIH), amelogenesis imperfecta, dentinogenesis imperfecta and tetracycline stains. Didactically, opacities not induced by fluoride are typically delimited and centralized, with rounded shape and normal enamel thickness (34). White spots lesions have a diffuse opaque area, extending in the cervical region and are associated with the presence of dental plaque or gingivitis (35). The MIH has demarcated and asymmetric opacities, located in the middle third of the tooth, especially, being more common in permanent teeth (first molar and central incisor) (36). The hypomineralized amelogenesis imperfecta, dentinogenesis imperfecta and stains occasioned by tetracycline are those that generate less confusion to diagnose, with the first two there is always a correlated inheritance pattern and the spots by tetracycline fluoresce under ultraviolet light (4). It is important not to confuse any of these defects with enamel hypoplasia, as this is a quantitative defect resulting of disturbance in enamel matrix secretion phase. Clinically, lesions have rounded and symmetrical cavities, with smooth and glossy surface, with no opacity signal (34).
The treatment of dental fluorosis is closely related to the lesions severity (15). In general, for the scores 1, 2 and 3, the microabrasion becomes the treatment of choice because reestablish aesthetics, providing a smoother and lossy surface (37). Because the technique is safe and minimally invasive it can be combined with teeth whitening, when necessary (37). The use of sodium fluoride is also recommended to promote the remineralization process in the demineralized enamel areas (38). From score 4 to 9, more invasive treatments are necessary. Options range from resin-based composite restorations, faceting of affected teeth or even total crowns (39). In each of the treatment options described above, each one has its own advantages and disadvantages; a good clinician should be aware of all the treatment options available assess its merits and demerits and select the best treatment option according to individual patient needs.
The knowledge is essential for the diagnosis and treatment of DF. Parents have the responsibility for control the fluoride intake by their children until the age of 7 years. The clinician should pass on knowledge about the associated factors, in addition to establishing the correct diagnosis of this dental enamel defects, based on severity, to obtain success in the treatment instituted.
Conclusion
The establishment of a proper diagnosis of dental fluorosis, based on clinical and histological features that depict the condition severity, is essential for family counseling and therapeutic decision.
Acknowledgements
Professor Ole Fejerskov by authorizing the reproduction of Figure 3B (Source: Fejerskov et al. Dental Fluorosis-a handbook for health workers, 1994).
References
1. Buzalaf MAR, Cury JA, Whitford GM. Fluoride exposures and dental fluorosis: A literature review. Rev Fob. 2001; 9(1/2): 1-10. [ Links ]
2. Molina-Frechero N, Gaona E, Angulo M, Sánchez Pérez L, González González R, Nevarez Rascón M, et al. Exposure Effects and Dental Fluorosis in Children in Mexico City. Med Sci Monit. 2015; 21: 3664-3670. [ Links ]
3. Vijayran M, Manuja N, Chaudhary S, Sinha A, Chaitra TR. Co-relation of body mass index, dental caries and periodontal status fluorosis in different high fluoridated areas of Haryana state. Indian J Dent Res. 2014; 25(6): 722-728. [ Links ]
4. Fejerskov O, Baelum V, Manji F, Moller IJ. Fluorose dentária: um manual para profissionais de saúde. São Paulo: Editora Santos; 1994. [ Links ]
5. Whelton HP, Ketley CE, McSweeney F, O'Mullane DM. A review of fluorosis in the European Union: prevalence, risk factors and aesthetic issues. Community Dent Oral Epidemiol. 2004; 32 (1 Suppl): 9-18. [ Links ]
6. Richards A, Kragstrup J, Josephsen K, Fejerskov O. Dental fluorosis developed in post-secretory enamel. J Dent Res. 1986; 65(12): 1406-9. [ Links ]
7. Alvarez JA, Rezende KM, Marocho SM, Alves FB, Celiberti P, Ciamponi AL. Dental fluorosis: Exposure, prevention and management. Med Oral Patol Oral Cir Bucal. 2009; 14(2): 103-107. [ Links ]
8. Everett ET. Fluoride's effects on the formation of teeth and bones, and the influence of genetics. J Dent Res. 2011; 90(5): 552-560. [ Links ]
9. Aoba T, Fejerskov O. Dental fluorosis: chemistry and biology. Crit Rev Oral Biol Med. 2002; 13(2): 155-170. [ Links ]
10. Tenuta LM, Cury JA. Fluoride: its role in dentistry. Braz Oral Res. 2010; 24(1 Suppl): 9-17. [ Links ]
11. Montero MJ, Douglass JM, Mathieu GM. Prevalence of dental caries and enamel defects in Connecticut Head Start children. Pediatr Dent. 2003; 25(3): 235-239. [ Links ]
12. Rozier, RG. Epidemiological indexes for mensuring the clinical manifestations of dental fluorosis: overview and critique. Adv Dent Res. 1994; 8(1): 39-55. [ Links ]
13. Thylstrup A, Fejerskov O. Clinical appearance of dental fluorosis in permanent teeth in relation to histological changes. Community. Dent Oral Epidemiol. 1978; 6(6): 315- 328. http://onlinelibrary.wiley.com/doi/10.1111/j.1600-0528.1978.tb01173.x/epdf [ Links ]
14. Pereira AC, Moreira BH. Analysis of three dental fluorosis indexes used in epidemiologic trials. Braz Dent J. 1999; 10(1): 29-37. [ Links ]
15. Alkhatib MN, Holt R, Beti R. Aesthetically objectionable fluorosis in the United Kingdom. Br Dent J. 2004; 197(6): 325-328. [ Links ]
16. Azevedo MS, Goettems ML, Torriani DD, Demarco FF. Factors associated with dental fluorosis in school children in southern Brazil: a cross-sectional study. Braz Oral Res. 2014; 28(1): 1-7. [ Links ]
17. Oliveira BH, Milbourne P. Fluorose dentária em incisivos Superiores permanentes em crianças de escola pública do Rio de Janeiro. Rev Saúde Pública. 2001; 35(3): 276-282. [ Links ]
18. Fejerskov O, Johnson NW, Silverstone LM. The ultrastructure of fluorosed human dental enamel. Scand J Dent Res. 1974; 82(5): 357-72. [ Links ]
19. Den Besten PK. Biological mechanisms of dental fluorosis relevant to the use of fluoride supplements. Community Dent Oral Epidemiol. 1999; 27(1): 41-47. [ Links ]
20. Denbesten P, Li W. Chronic fluoride toxicity: dental fluorosis. Monogr Oral Sci. 2011; 22: 81-96. [ Links ]
21. McDonagh MS, Whiting PF, Wilson PM, Sutton AJ, Chestnutt I, Cooper J, et al. Systematic review of water fluoridation. BMJ. 2000; 321(7265): 855-859. [ Links ]
22. Limeback H. Enamel formation and the effects of fluoride. Community Dent Oral Epidemiol, 1994; 22(3): 144-147. [ Links ]
23. Frazão P, Peverari AC, Forni TIB, Mota AG, da Costa LR. Dental fluorosis: comparison of two prevalence studies. Cad. Saúde Pública, Rio de Janeiro. 2004; 20(4): 1050-1058. [ Links ]
24. Pascoe L, Seow WK. Enamel hipoplasia and dental caries in Australian Aboriginal children: prevalence and correlation between the two diseases. Pediatr Dent. 1994; 16(3): 193-199. [ Links ]
25. Marthaler TM. Increasing the public health effectiveness of fluoridated salt. Schweiz Monatsschr Zahnmed. 2005; 115(9): 785-792. [ Links ]
26. Moimaz SAS, Saliba O, Chiba FY, Sumida DH, Garbin CAS, Saliba NA. Fluoride concentration in pubic water supply: 72 months of analysis. Braz Dent J. 2012; 23(4): 450-456. [ Links ]
27. Broffitt B, Levy SM,Warren JJ, Heller KE. Seasonal variation in fluoride intake: the Iowa fluoride study. J Public Health Dent. 2004; 64(4): 198-204. [ Links ]
28. Moura MS, Gomes LMA, Castro MRP, Teles JBM, Moura LFAD. Dental fluorosis in 12-year-old adolescents. RGO. 2010; 58(4): 463-468. [ Links ]
29. Marthaler TM. Salt fluoridation and oral health. Acta Med Acab. 2013; 42(2): 140- 55.
[ Links ]
30. Alaluusua S, LukinmaaPL, Koskimies M, Pirinen S, Hölttä P, Kallio M, et al. Developmental dental defects associated with long breast feeding. Eur J Oral Sci. 1996; 104(5-6): 493-497.
[ Links ]
31. Mehta DN, Shah J. Reversal of dental fluorosis: A clinical study. J Nat Sci Biol Med. 2013; 4(1): 138-144. [ Links ]
32. Campos C, Toledo AO, Bezerra AC. Prevalence of dental fluorosis in school children from Brasília-Federal District. Rev Odontol Univ São Paulo.1998; 12(3): 225-230. [ Links ]
33. Thylstrup A. Is there a biological rationale for prenatal fluoride administration?. ASDC J Dent Child.1981; 48(2): 103-108. [ Links ]
34. FDI Commission on Oral Health. A review of the developmental defects of enamel index (DDE Index). Int Dent J. 1992; 42(6): 411-426. [ Links ]
35. Denis M, Atlan A, Vennat E, Tirlet G, Attal JP. White defects on enamel: diagnosis and anatomopathology: two essential factors for proper treatment (part 1). Int Orthod. 2013; 11(2): 139-165. [ Links ]
36. Weerheijm KL, Duggal M, Mejà re I, Papagiannoulis L, Koch G, Martens LC, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003; 4(3): 110-113. [ Links ]
37. Pini NI, Sundfeld-Neto D, Aguiar FH, Sundfeld RH, Martins LR, Lovadino JR, et al. Enamel microabrasion: An overview of clinical and scientific considerations. World J Clin Cases. 2015; 3(1):34-41. [ Links ]
38. Sundfeld RH, Sundfeld-Neto D, Machado LS, Franco LM, Fagundes TC, Briso AL. Microabrasion in tooth enamel discoloration defects: three cases with long-term follow-ups. J Appl Oral Sci. 2014; 22(4): 347-54. [ Links ]
39. Sherwood IA. Fluorosis varied treatment options. J Conserv Dent. 2010; 13(1): 47-53. [ Links ]