Introduction
Diseases that affect the salivary glands are frequent and may manifest clinically through increases in volume and functional impairments. The origin of these alterations can be autoimmune, infectious, neoplastic, traumatic and even drug-induced. Its diagnosis is based on clinical and histopathological aspects, and sometimes on complementary analyses. However, in some cases the clinical diagnostic impression is enough to establish a definitive diagnosis.
Dysfunction of the salivary glands involves a constellation of manifestations ranging from hypofunction and xerostomia to subjective and objective sialorrhea. Xerostomia is described as the subjective sensation of dry mouth reported by the patient; on the other hand, the hypofunction of salivary glands is an objective measure reflected in the decrease of saliva secretion. Interestingly, their symptoms may be secondary to qualitative and/or quantitative changes in the composition of saliva. Chronic xerostomia may affect denture-wearing, speech, chewing, swallowing and general well-being and, when it is secondary to hyposalivation may also result in rampant dental caries, periodontal disease, oral fungal infections, taste reduction, halitosis or burning mouth. More than 100 different medications have been reported with high and moderate levels of evidence to cause these alterations 1,3.
Xerostomia is a debilitating condition that is diagnosed clinically by means of questionnaires and subjective analogous scales that have been used in several studies over the last decades 4,8. On the other hand, there are the histopathological diagnostic methods commonly used to identify the diseases that affect the salivary glands.
In Brazil, Fonseca et al. 9 and Moreira et al. 10 analyzed the data from two histopathological diagnostic services. Since they did not include an oral medicine service, which reduces the number of eminently clinical diagnoses like xerostomia and sialolithiasis, they found a greater number of salivary gland neoplasms.
It is for this reason that we aimed to identify the most frequent salivary gland diseases diagnosed at the Diagnostic Histopathological Service and in an Oral Medicine Service in the Araraquara School of Dentistry, São Paulo State University (FOAr-UNESP), from 2009 to 2013.
Materials and methods
Ethical considerations
The protocol of this study was approved by the Ethics Committee of the Araraquara School of Dentistry, São Paulo State University (FOAr-UNESP) Júlio Mesquita Filho (CEP: 15608213.4.0000.5416).
Data Collection
We identified all patients who were diagnosed with conditions associated with salivary glands attended in the period 2009 to 2013. The medical records were retrieved from the archive of the Diagnostic Histopathological Service of the Department of Physiology and Pathology (n= 1,217) and from the Oral Medicine Service (n= 2,236). Clinical reports were compiled for one year, two expert oral pathologists meticulously re-evaluated histopathological reports and patient case notes. Samples with erroneous, doubtful and controversial diagnoses were excluded. Two experienced oral and maxillofacial pathologists from the Department of Physiology and Pathology perform the histological diagnosis independently for each biopsy, mainly based on staining sections of hematoxylin-eosin embedded in paraffin. Sometimes the conjunction of immunohistochemical staining and / or histochemical staining was used. All diagnoses were confirmed by a review of the slides and, if a disagreement was identified in the diagnosis, a consensus was reached through a discussion.
Clinical variables such as age, sex, race, location of the lesion, medical history, medication, and radiographic aspects were collected and tabulated. The World Health Organization (WHO) standard, known as topographic classification for diagnosis of oral mucosal lesions, was used to determine the location of the lesions 11. Xerostomia diagnosis was established by experienced board-certified stomatologist using a careful evaluation of signs and symptoms, with clinical extra-oral and intra-oral examinations, assessment of salivary gland function by measurement of resting and stimulated flow rates, and, in some cases, biopsy of minor salivary glands.
Data Analysis
The data were analyzed in Prism 5.0b (GraphPad Software, Inc) to destribe the distribution of data. Contingency table analysis in Chi-square test, two-tailed, confidence intervals 95% with additional calculations of Odds ratio and relative risk were used to verify the relative risk to xerostomia in gender.
Results
From a total of 2,236 medical records and 1,217 histopathological reports reviewed, 254 alterations associated with salivary glands were diagnosed in 253 patients (only one patient had two diagnoses simultaneously). The mean age of the patients was 45.6 years (median 50, SD 21 years). The proportion of females/males was 1.52. Regarding race, light-skinned people accounted for 62.8% the study population, followed by mixed race (7.6%) and dark-skinned people (3.8%). The most frequently reported glandular diseases are described below (Table 1).
Table 1 Diagnostic distribution of salivary gland diseases, Araraquara School of Dentistry, São Paulo State University (FOAr-UNESP), 2009-2013.
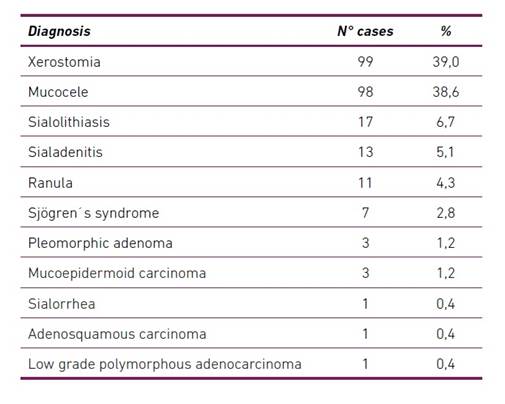
A common clinical finding was xerostomia (39%), mainly in patients on medication treatment. In these patients, an average age of 59.7 years (median of 60 years, SD 12.1 years) and predominance of females (3.04 F / M) with a relative risk of 0.69 (Odds ratio 0.27 to 0.93) were observed. In addition, it was identified that 45% of patients with xerostomia used more than one medication (52.1% two medications, 36.9% three medications and 10.8% four medications) (Table 2).
Table 2 Distribution of drug use between women and men diagnosed with xerostomia, Araraquara School of Dentistry, São Paulo State University (FOAr-UNESP), 2009-2013.
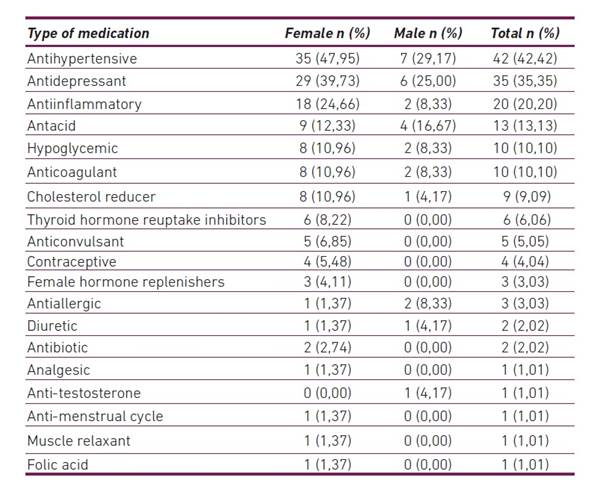
Due to the high prevalence of the female gender among patients diagnosed with xerostomia, we separated the data by gender. We observed that antihypertensive and psychiatric drugs remained as the most frequently associated with xerostomia in both genders. We also found that drugs used to treat gastric ulcers gained importance in the male gender, appearing as the third class of medications most frequently associated xerostomia.
With regard to patients with a clinically diagnosis of mucocele or ranula, we observed that the most frequent histopathological diagnosis was mucus extravasation (85.2%), followed by fibrous scar or chronic sialadenitis (4.9%) and mucus retention phenomenon (3.2%). The most frequent location of the mucocele was the lower lip (60.1%), followed by the buccal mucosa (8.3%), the tongue (5.5%), the upper lip (2.7%) and palate (0.92%); as for the ranula, it was the floor of the mouth (22.2%). The mean age of the patients with mucocele was 30.5 years (median 28; SD 18,1 years), while for the patients with ranula was 32 years (median 38; SD 18,2 years).
Patients diagnosed with sialolithiasis had a mean age of 57.7 years (median 59; SD 11,9 years), with a predominance of females (1.4 F / M). The most frequent location was the region of submandibular glands with 64.3%, followed by the upper lip and the parotid region (14.3% each), and the sublingual region (7.1%). We also verified that in 70% of the cases the diagnosis was confirmed with a histopathological examination. The remaining cases were diagnosed using radiographic examinations only.
The patients diagnosed with sialadenitis had a mean age of 57.6 years (median 59,5; SD 10 years). The gender was equally distributed and the most common location was the parotid (40%), followed by the buccal mucosa (20%) and lips (10%).
Among the diagnosed neoplasms, we found a predominance of malignant neoplasms (62.5%) compared to benign neoplasms (37.5%). We also observed a strong predominance of malignancies diagnosed in minor salivary glands: palate (37.5%), lower lip (12.5%), floor of the mouth and alveolar ridge (12.5%). Only one case was diagnosed in the submandibular salivary gland (12.5%). Patients diagnosed with malignant neoplasms had a mean age of 53 years (median 60; SD 21 years), and all were males. All diagnosed mucoepidermoid carcinomas occurred on the palate and floor of the mouth. The adenosquamous carcinoma and low-grade polymorphic adenocarcinoma occurred in the inferior alveolar ridge and the palate, respectively.
All benign neoplasms diagnosed in the study population corresponded to pleomorphic adenomas and were found in three different locations: hard palate, submandibular region and lower lip. The relationship between female and male gender was 2.0 (F / M). The mean age of the patients was 35.3 years (median 33; SD 19,6 years).
Discussion
The present retrospective descriptive study was based on 2,236 clinical records and 1,217 digital data from the Oral Medicine Service and the Diagnostic Histopathological Service of the Araraquara School of Dentistry (FOAr-UNESP), respectively. We identified 254 diseases of salivary glands. We found a high prevalence of mucoceles, followed by sialolithiasis, sialoadenitis and ranula. Cases of Sjögren’s syndrome, pleomorphic adenoma, mucoepidermoid carcinoma, sialorrhea, adenosquamous carcinoma and low-grade polymorphic adenocarcinoma were few in our sample. The most frequent clinical finding was xerostomia, especially in individuals under treatment with antihypertensive, psychiatric and anti-inflammatory drugs.
Bettio et al.12 when evaluating the histopathological diagnosis file in a brazilian university, in a period between 1999 and 2008, reported the presence of 73 (3.6%) cases of diseases of the salivary glands of a total of 1,990 records. These authors described a higher prevalence of mucoceles (79.4%), followed by pleomorphic adenoma (9.5%), other reported lesions were sialadenitis and adenoid cystic carcinoma (2.7% each), mucoepidermoid carcinoma, Sjögren’s syndrome and ranula (1.3% each). In this case, it should be noted that histopathological examination reports were exclusively evaluated, therefore, findings such as hyposalivation, xerostomia and sialorrhea that are diagnosed clinically may be missed if the studies do not include the patient’s clinical records. Our sample was obtained from an Oral Medicine Service, which shows differences in the frequency of the alterations diagnosed according to the origin of the data. The same year Moreira et al.10, carried out an epidemiological study with a sample of 20 years. The authors reported that the source of their data was the “Maranhense Institute of Oncology: Aldenora Bello”. Their data show that the most frequent diseases were pleomorphic adenoma (27.7%), sialoadenitis (19.2%), cystic adenoid carcinoma (14.6%) and mucocele (11.9%). We can observe a tendency related to the source of data collection (Institute of Oncology) that led to the greater diagnosis of neoplasms, to the detriment of the routine clinical diagnosis of an oral medicine service.
Several researches have studied the prevalence of salivary gland tumors (9,13-16). Most have been performed in pathology laboratories of universities (9,13-14) such as in the present study, and others in pathology services of local hospitals (15-16). In general they report an average age of patients with malignant neoplasms between 47.9 and 60.9 years, which coincides with our findings (53 years), while in the case of benign neoplasms they report average ages between 38.2 and 53.3 years, our population being slightly younger (35.3 years). Regarding the proportion of malignant and benign neoplasms, they report between 25.1% to 53.5% of malignant, and between 46.5% to 74.8% of benign neoplasms. In our study, malignant neoplasms (62.5%) were more frequent, such as mucoepidermoid carcinoma (1.2%), adenosquamous carcinoma (0.4%) and low-grade polymorphic adenocarcinoma (0.4%), and affected almost all cases to the minor salivary glands of the palate (37.5%). As for the benign neoplasms, all were pleomorphic adenomas located on the palate, submandibular gland and lower lip, which coincides with the aforementioned studies, except in the location, since they report the parotid gland in the first place and the palate in second place. These differences may have been explained by the variations in the populations, however, our sample was too small to make generalizations.
Our most frequent finding in the clinical records was the diagnosis of xerostomia. Xerostomia can be the result of systemic diseases of endocrine, autoimmune, infectious and granulomatous type among others; and local factors such as the use of certain medications, radiation therapy of the head and neck, and some lifestyle habits 17. Recently, Wolff et al. 1 suggested the association between xerostomia and medications used to treat conditions in almost all systems of the body. Some medications alone may not be enough to produce xerostomia but consuming them in combination with others may result in drug interactions and subsequent xerostomia. Niklander et al. 7 evaluated the frequency, associated factors and quality of life of 556 patients with xerostomia. They found that the prevalence of xerostomia in patients who took some type of medication was 17.92%, while 70.5% of patients with xerostomia took one or more medications, and that the possibility of having xerostomia increased 1.12 times with each additional medication that was taken. They found a statistically significant association between the use of antidepressants, antihypertensives and antihistamines with xerostomia. In terms of age and gender, they report that women are 1.56 times more likely to have xerostomia and that for each additional year of life the possibility of having a dry mouth increases 1.01 times. They conclude that sex, age and medication were independent risk factors for the development of xerostomia and that the quality of life of these patients was significantly reduced. Our findings coincide in some aspects, since xerostomia also prevailed in the female gender (3.04 F / M) and in elderly patients (59.7 years), the drugs most used by patients with xerostomia were antihypertensive (42.4%) and psychiatric (35.3%) type, and in 45% of the cases they ingested more than one medication at a time. However, the quality of life was not evaluated since it was a retrospective study and it was not the objective of it.
A decrease in the rate of salivary flow in middle-aged and elderly people has been shown, however, this could be the result of a greater number of systemic diseases and the use of drugs for their treatment than to an inherent change by the age 18. There is controversial literature supporting the idea that aging is associated with decreased salivary flow independently of drug use, and especially affects the sublingual and submandibular salivary glands 19.
Finally, the objective analysis of the salivary flow is recommended since our results are based on the subjective sensation reported by patients who use drugs. The severity of the reduction of the salivary flow and the presence of xerostomia could be dose dependent, therefore it would be important to report the dose and the time of drug use in later studies.
Conclusions
Our findings show the importance of a careful diagnosis, not only for neoplastic lesions, but also for pathologies of autoimmune, inflammatory and traumatic origin, which make up a greater number of cases. The diagnosis of these lesions allows the adequate treatment of the patient, through surgical procedures, drug treatment, or even referral of the patients to other specialized professionals for a more complete approach.
In addition, the high frequency of patients affected by xerostomia highlights the importance of not only performing the histopathological diagnosis of salivary gland diseases but also a careful clinical diagnosis of conditions associated with them, given the relationship with the intake of medicines with xerogenic effects.














