Introduce
The formation of calcific concretions in the salivary duct or glands is a common disorder 1. Salivary calculi are usually small, measuring from 1 mm to less than 1 cm, and especially are in the submandibular glands 1. Drage et al. mentioned finding parotid and submandibular stones, averaging 3.4 mm (range from 1.5 to 9 mm) in size and a 1.67 (range from 1 to 5) in quantity per one patient, 2.
Different aetiological hypotheses about salivary gland calculi were described: mechanical, inflammatory, chemical, neurogenic, infectious, strange bodies, etc. Anyway, it seems that the combination of these factors usually determines the precipitation of the amorphous tricalcic phosphate, which, once crystallized and transformed into hydroxyapatite becomes the initial focus 3.
Parotid calculi represent only a small proportion of all salivary calculi 4, more than 6% of the sialoliths occur in the parotid gland 5. This case was never reported in the literature and describes a rare coexistence of a cutaneous fistula with salivary stones located in the superficial lobe of the parotid gland that was removed under local anesthesia.
Relate Case
A 54-years-old, female patient, came to Piracicaba Dental School (UNICAMP), referred by her dentist, her major complaint was the growth of a “lump” in her face about a year and a half ago, and when palpated had painful symptomatology. The patient reported that six months ago a extraoral fistula had occurred in the right parotid region with intermittent episodes of acute exacerbation; previously the patient had been treated in other services, according to her, she was medicated with amoxicillin and azithromycin for 15 days with no improvement of her the clinical condition. Later it was performed the extraction of the teeth # 13, 15, 16 and 18; which caused the worsening of the clinical course. Patient suspected she had skin disease and began to use topical ointments in the region but no improvement was observed.
Intra oral physical examination revealed good oral hygiene, without periodontal disease or fistulous processes. There was not clinical sign of infection in the cicatrization process of the teeth sockets. In extra oral physical examination was observed an ulcerated fistula process in right parotid gland region (Figure 1), without deficit in facial expression muscles, pain on palpation of the affected gland but without apparent lesion or purulent secretions drainage through the fistula and orifice duct.
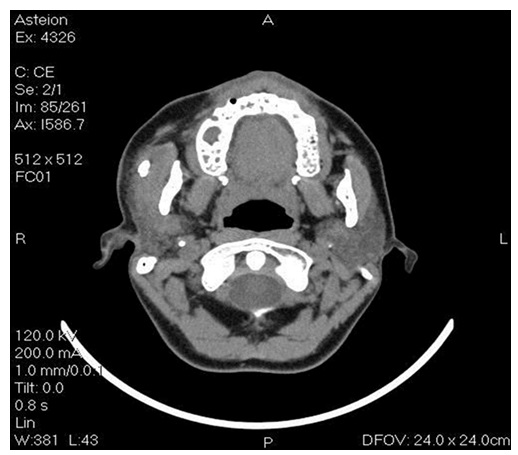
Computed tomography (CT) showed the presence of a spherical radiopaque image suggested a possible sialolith with diameter of approximately 12 mm, located superficially at the right parotid gland (Figure 2). During the initial evaluation, it was not observed the presence of this lesion in her panoramic radiograph.
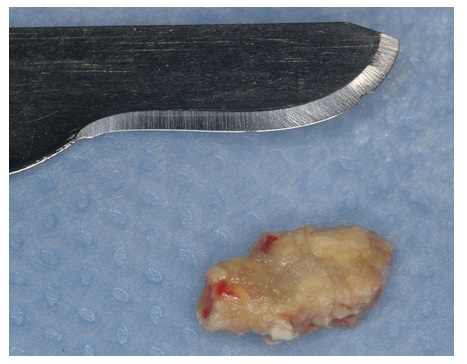
Sialolith exeresis was performed under local anesthesia through a skin incision with approximately 2 cm with careful dissection to avoid injuries to the glandular tissue and facial nerve preventing future salivary fistulas and facial paralysis (Figure 3). The anatomopathological exam revealed the presence of hard tissue, measuring 9x5x4 mm with an irregular shape; yellowish color (Figure 4) without the presence of salivary glands confirming the diagnosis of sialolith. After two weeks, in the prostoperative visit it was observed remission of the ulcerated fistula process; parotid gland with normal salivary function, permeable Stensen duct and without alterations of facial expression muscles.
Discussion
As in other disease processes, the most important components in the diagnosis of salivary gland disorders are patient’s history and clinical examination. In our clinic evaluation, the patient had clinical signs commonly observed in malignant tumors including, pain, numbness, weakness and swallowing trouble. However, lump formation or salivary glands swelling can also arise from non-neoplastic causes, including infection, sialolithiasis, sarcoidosis, amyloidosis and Sjogren syndrome 6. The professional should perform a detailed clinical evaluation accompanied by an appropriate imaging examination, it is important in the differentiation of benign and malignant lesions.
Shenoy V.S et al., 2015 7, described a case of coexistence of salivary calculi in the deep lobe and adenoid cystic carcinoma (ACC) in the superficial lobe infiltrating to the deep lobe of the parotid gland. They concluded that ACC of parotid etiology isn't fully understood and the coexistence of ductal calculi and ACC of parotid is a rare fenemen with few litterature reports; and that confirmatory studies are required to understand the mutual pathological association of calculi and carcinoma 7. In our case, the patient had an extraoral ulcer in the right parotid region that could not be healed, yet another health service, suggested a possible diagnosis of cancer without doing a single biopsy exam. A imaging exam was performed and revealed a close calcification in the region that could be the injury etiology. Lee et al., 2014 cited that the management of benign and malignant tumors in the salivary gland are different, and correct identification of the nature of the tumor can lead to completely different management recommendations 6. In this report, the salivary calculi diagnostic was obtained through clinical evaluation and CT’s support.
Magnetic resonance (MR) imaging is the method of choice for patients with palpable masses and a strong suspicion that the lesion is neoplastic 8, however the CT is the method of optimal in patients suspicious for inflammatory disease (abscess, calculi, major salivary duct dilatation, and acute inflammation) or in patients with contraindication for MR imaging. For CT imaging both pre- and post-contrast studies must be performed in order to detect calcifications (pre-contrast) and enhancement pattern (post-contrast). In our report, the panoramic radiograph did not show any changes which may have confused other colleagues, so we requested a more accurate imaging study to facilitate the diagnosis and treatment planning. CT have information on the exact localization and extent of the lesion, addresses neighboring structures, so, after seeing that the lesion was not close to important structures (facial nerve) and its location was superficial to the parotid gland, sialolith exeresis was held. The facial nerve cannot usually be visualized by imaging, however a virtual line drawn from the lateral border of the posterior belly of the digastric muscle and the retromandibular vein to the lateral edge of the mandible can be used as an anatomical landmark 8.
Conclusion
This patient provides a good illustration of the difficulty there may be in establishing the diagnosis of parotid calculus:as shown in this report, the patient had previous evaluations that did not appoint any presence of sialolith. Such analysis led the first evaluation dentist to a false assumption with odontogenic infection as a possible cause of extraoral fistula. As a result, an extraction of elements that were close to the fistula was wrongly performed. We hope that this rare case report will help health professionals, reinforcing the importance of proper diagnosis based on clinical and imaging evaluations therefore to be finally be capable to categorize the pathology as reactional, obstructive, inflammatory, infectious, metabolic, neoplastic, and traumatic or development causes.