Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957versión On-line ISSN 2500-7440
Rev Col Gastroenterol v.26 n.4 Bogotá oct./dic. 2011
Incidental foreign body in the gastrointestinal tract. Report of three cases and literature review
Luis Alberto Ángel Arango, MD (1), Lina Paola León Sierra, MD (2), Diana Carolina Martínez Gutiérrez, MD (2), Marcela Jurado Grisales, MD (3)
(1) Internist, Gastroenterologist, and Nutritionist. Tenured Professor at the Universidad National de Colombia in Bogotá, Colombia.
(2) Surgeon at the Universidad Nacional de Colombia. Bogotá, Colombia.
(3) 12th Semester Medical Student at the Universidad Nacional de Colombia. Bogotá, Colombia
Translation from Spanish to English by T.A. Zuur and The Language Workshop
Received: 24-07-11 Accepted: 11-10-11
Abstract
Foreign body ingestion is a common condition in the emergency department. Although most objects get away without symptoms, events occur depending of their location and characteristics or may go unnoticed and later cause severe complications that threaten the patients life. We report three cases of foreign bodies identified during upper gastrointestinal endoscopy as an incidental finding and a review of the epidemiology of this condition, and the variety of clinical presentations depending on the organ involved, secondary complications and diagnostic approaches. Finally, we propose a flow chart diagnosis and treatment that unifies those proposed in the literature.
Key words
Foreign body, incidental, digestive tract, complications, flow chart.
INTRODUCTION
Foreign body ingestion is a condition commonly seen in emergency departments (1-6). In most serious cases, the foreign body is ingested by accident (3, 7-9). Accurate diagnosis and timely treatment to prevent complications and reduce morbidity and mortality associated with foreign body ingestion constitute a challenge for gastroenterology, pediatrics, and surgery (6, 24-26).
In most cases, foreign object ingestion in adults is accidental, although it may be linked to physiological, anatomical, mechanical, social and psychiatric factors (2,10,13-23). The frequency of voluntarily ingested objects is higher among children and teenagers than in any other age group (6, 24-26). In most cases, patients who see the doctor due to foreign object ingestion present transitory symptomatology. Less people go to the doctor because of persistent clinical manifestations or secondary manifestations of previous complications. In other cases, the foreign body is found incidental to another medical procedure (13, 20, 27-42).
The foreign body can generate various symptoms, depending on its anatomical location. Because this clinical condition is so varied, the approach to the patient must start with a complete and detailed clinical history plus a physical assessment to corroborate the patients symptomatology and to identify the emergency cases. Imaging can be of great assistance in some cases to locate foreign objects, reveal complications, confirm diagnosis and suggest therapeutic options such as endoscopy or more invasive interventions such as surgery.
Here we present three clinical in which foreign bodies were found incidental to endoscopies and a literature review of the issue. The review is limited to foreign objects in the upper GI tract, since most foreign objects found in distal portions of the digestive tract are the result of voluntary events (14, 43).
CLINICAL CASES
Case 1. An asymptomatic 57 year old woman undergoing a gastroenterological examination was referred for an endoscopy because of dyspeptic symptoms. An upper digestive tract endoscopy revealed normal caliber and normal esophageal mucosa with a tear in the right posterior wall below the gastroesophageal (GE) junction produced by nausea triggered during the exam. The gastric mucosa showed patchy congestion, the pylorus was normal, and the patient tested positive in the Helicobacter pylori rapid urease test. A one-centimeter foreign object was found embedded at the back of the posterior wall of the duodenal bulb (Fig.1A). Upon removal with biopsy forceps it could be clearly seen that it was a three-centimeter long fishbone (Figure 1B). The procedures presented no complications. When asked, the patient said that she had eaten fish the day before. When something bothered her pharynx, she ate some yuca (Cassava) which successfully soothed the malaise.
Figure 1A) Duodenal bulb. Foreign body embedded in posterior wall.
Figura 1B. Cuerpo extraño en bulbo duodenal. Extracción endoscópica.
Case 2. An 80 year old woman patient was referred to a gastroenterologist for removal of a percutaneous endoscopic gastrostomy (PEG) tube one year after it had been placed. Placement was due to a severe swallowing disorder after cerebrovascular event. After her feeding and swallowing improved, it was decided to remove the PEG tube. During endoscopy a foreign object was could be seen in the subglottic region (Figure 2A), which seemed to be fishbone under magnification (Figure 2B). There was no evidence of any alteration in the esophagus. The PEG tube was removed successfully and the patient was referred to pulmonology and otolaryngology for foreign-body extraction.
Figure 2A. Foreign body in the subglottic region.
Figure 2 B. Detail.
Case 3. A 60 year old man was referred for endoscopy because of dyspeptic symptoms. One month later endoscopy results showed gastric fluid with few black traces of blood and punctuated erosions of the fundic mucosa with traces of recent bleeding. The antrum presented patchy erythema alternating with depressed areas and a raised lesion near the junction of the corpus and antrum over the greater curvature towards the back wall of the stomach. Biopsies of the lesions were taken. A foreign body was embedded in the side (fig 3-A) wall in the middle of the junction with the duodenum (Figure 3B). The object was a three-and-a-half-centimeter chicken bone (Figure 3D) which was extracted without complications (Figure 3C). When asked, the patient said he had not noticed any symptoms and that he had not been aware of the foreign object in his stomach. He also stated that he had eaten chicken 48 hours prior to the examination without symptoms during or after ingestion of the bone.
Figure 3A-D. Duodenum. Foreign body (bone fragment). Endoscopic extraction.
EPIDEMIOLOGY
80% to 90% of ingested foreign objects pass through the gastrointestinal tract (GIT) without causing injuries. In fact, it is estimated that only 1% of these cases present some kind of associated complications such as lacerations, impaction, obstruction and visceral perforation which require surgical treatment (2, 3, 6, 24, 44, 45).
The average reported age of occurrence in adults is between 43 and 63 years old (10, 11, 30, 46) while the highest incidence among children occurs in patients under the age of 5 (6, 9, 50, 51). Some predisposing factors for foreign body ingestion have been observed in adults and senior adults (Table 1). These include the natural narrowness of the male esophagus, the use of dental prostheses due to reduced sensitivity of the covered area of the palate, mental retardation, psychiatric history associated with episodes of pica disorder, and convicts who seek to escape imprisonment when sent to a hospital or a mental health unit (2, 4, 13, 20, 21, 27-42, 47-49).
Table 1. Factors which predispose patients for ingestion of a foreign object.
While it is true that there are many different types of foreign bodies that can reach the gastrointestinal tract, they vary according to group (Table 2) (1, 5,45, 50). Most objects swallowed by children are metallic (coins, batteries, etc.) (44, 50-53). Among adults fish bones (Cases 1 and 2) (4, 49) and chicken bones (Case 3) (13, 15, 16, 30, 49) are the most common followed by dental prostheses (1, 8, 41, 54), toothpicks (10, 20, 23, 30, 32, 40, 47, 49) and needles (36, 48, 49, 55). In addition to these, other objects such as bezoars (2, 10, 34, 56, 57), toothbrushes (1,58) safety pins (50, 56), pens (33) and seashells (28, 37, 61) are swallowed. In fact, sharpness and large size of the foreign object (6cm high, 2cm long or 2,3 inches high and 0,7 inches long) facilitate its retention (10, 25, 44, 45, 49, 50, 56 59, 60).
Table 2. Foreign body distribution in GI tract according to age.
There are anatomical regions where foreign objects can cause greater impacts, penetration or even perforation of an organ due to the structures natural narrowness or angles (2, 19, 28, 30-32, 35, 48, 51). Narrow passages include the hypopharynx (4, 25), the esophagus, the upper esophageal sphincter, the aortic arch, the esophageal hiatus (2, 25, 30, 38, 53, 63), stomach (1, 28, 50, 60), and the ileal cecal region (21, 29, 60). Angular regions include the duodenum (Cases 1 and 3) (1, 32, 50, 58, 60) and the rectal sigmoid (Table 3) (14, 29, 43, 48). Other conditions such as anatomical birth anomalies and anastomosis increase the risk of foreign object retention (1, 3, 5, 6, 19, 25, 62).
Table 3. Anatomical location of foreign objects in GI tract.
CLINICAL MANIFESTATIONS
Clinical manifestations during the acute course of the event may vary between patients who are able to inform another person about ingestion of foreign body, and those such as very young children and patients with a mental condition who cannot. These manifestations depend on where the object is located. When the object is in the esophagus, the patient presents odynophagia, nausea, vomiting, hypersalivation or respiratory symptoms such as coughing fits and dyspnea (2, 4, 5, 25, 28, 51, 64). These are related to compression of the trachea and larynx, the structures of the upper respiratory system which are adjacent to the esophagus. In addition, retrosternal pain is common (2, 4, 13, 50, 51). It may be relieved as the object passes to the stomach or it may persist if its passage causes a lesion or it becomes impacted in the esophageal mucosa. When the foreign body reaches the duodenum and passes through the intestine, abdominal pain can occur in association with obstruction or partial obstruction (13, 19, 30, 50). If the object passes through to the rectum, the patient may develop rectal bleeding (14, 29, 51, 63).
Although in most cases foreign bodies pass through the upper GI tract without causing any alteration (1, 2, 30, 45), 1% of these patients show complications because of the retention of the object and will require specific treatment. The most common complications are lacerations, perforations (13, 19, 32, 36, 44, 48), impactions and obstructions of the GI tract (13, 32, 36, 44). These depend on the nature of the foreign object and on the anatomical features of the region where the object is retained (3, 11, 44, 51, 56, 67). Often, after ingesting a foreign body, patients try to deal with the situation by eating bread, potatoes, yucca, bananas, or other food to facilitate movement or impaction. In some cases patients are not even aware of the situation and only visit the doctor months or even years after ingestion when the complications arise (27, 28, 47, 48, 65) (patient 2), when tissue lesions are evident, or when even more critical circumstances which can put patients lives at risk (such as severe organ damage) develop (1, 2, 17, 47, 48).
The most frequent clinical manifestations which present themselves are weight loss (47, 48), anorexia (35, 47, 48), asthenia, adynamia, emesis (29, 31-34, 47, 48), abdominal pain (with or without signs of peritoneal irritation) (29, 35, 36, 47, 48, 50), obstruction (13), fever (28, 29,31, 35, 47, 48), hematemesis (3, 15, 41, 66), jaundice (20, 47, 48) and signs of systemic inflammatory response (20, 28, 29, 35). In cases where there has been perforation, the omentum prevents progress in the initial stage and covers the wound which is why the symptoms appear so insidiously and progressively (33, 36).
The incidence of severe complications in the esophagus due to foreign body ingestion are very low, from 0% to 3% (67, 68). They are usually linked to the place where the object is retained and the time elapsed between the moment of ingestion and medical consultation. Perforation of the esophagus is a severe complication that is usually accompanied with pain, dyspnea, fever, or dysphagia (2, 4, 7, 25, 38, 64, 69, 70). Very rarely it is accompanied by subcutaneous emphysema (64, 70). However, foreign bodies common cause mild esophageal complications such as erosion, superficial laceration, edema and hematoma due to (2, 4, 38, 64).
Perforation of the GI is produced by sharp objects such as bone fragments, fish bones, toothpicks and paper clips (1, 5, 45, 50) that often pierce the ileocecal and rectosigmoid regions and the duodenum producing bleeding which can spread to adjacent organs (53, 66, 67, 71). Perforation can also produce fistulas (13, 15, 20), abscesses (13, 35, 39, 48), and systemic problems such as peritonitis and sepsis (13,35, 39, 48, 63, 71). When the duodenum is perforated, commonly occurring lesions include formation of abscesses in the liver (17, 35, 39, 48, 71, 72), right kidney hydronephrosis, duodenum-kidney fistulas (20, 73, 74) and damage to vascular structures including the aorta (44, 46) and the vena cava (20, 47).
DIAGNOSIS
Patients who go to the doctor due to foreign body ingestion might or might not present symptoms. Those who are not aware that the episode has occurred do not visit a doctor. In these cases, the normal course of events is for the object to be expelled naturally (2, 3, 6, 24, 44, 45). Sometimes complications arising from movement of the object into the GI tract lead to identification of the FO as the source of the problem (14, 15, 17, 28, 29, 30, 36, 38, 50, 58, 74, 76). In the cases such as those described above, identification of the FO is incidental to other procedures including X-rays, endoscopy, and surgery (13, 27, 29, 31-35, 37, 39, 40-42, 73, 75).
During medical consultation, older children and adults without histories of psychiatric illnesses remember the event easily. In most cases, they can locate the area where they feel discomfort or pain. Even though this localization is not completely reliable, it can be an aid to examination and diagnosis (3). When taking the patients medical history it is important to inquire about the characteristics of the object, time of occurrence, actions taken after ingestion and associated symptoms (2-4, 25, 56). Precedents are very important for identifying factors predisposing ingestion. Predisposing factors include diverticulitis (13), diverticulosis (29) Mackles diverticulum (13), congenital GI tract diseases and intestinal anastomosis (13).
Vital signs must be checked during physical examination to look for systemic involvement or hemodynamic instability. The physician should check for signs of compromised air passage and esophageal perforation such as erythema, neck sensitivity or neck and upper thorax crepitus (2-4, 64). If the patient can identify the location of pain, the doctor must listen to hear any bowel or peristaltic sounds, and examine the location for signs of palpable masses, peritoneal irritation and intestinal obstruction.
After taking the medical history and performing the physical examination, the diagnosis can confirmed through x-rays of the neck, thorax and abdomen. These images facilitate diagnosis in cases where there are radiopaque objects like batteries, coins and other metallic objects (6, 44, 45, 51, 56). R. Palta et al. (60) managed to visualize the foreign object in 85% of 222 different cases they studied. Conversely, W. Cheng et al. (68) only performed x-rays on 934 (74%) of 1265 cases and detected foreign bodies in only of 43% of those x-rayed. 100% of the metallic objects were detected, 86% of the glass objects were detected, but only 26% of the fish bones were detected. The low percentage of fish bones detected is due to the thinness of the bones, to soft tissue wrapped around the bones and to fluids accumulated around the lesion (16). X-rays also allow detection of complications when there are gasses in the mediastinum or the peritoneal cavity (3, 48, 53).
When it is impossible for a simple X-ray to identify an object, but the object is a large, radiolucent foreign body, then a barium sulfate X-ray is better (50). Contrasting means for this kind of X-ray must be used with caution, because full obstruction of the esophagus could cause bronchoaspiration of the barium sulfate suspension (3, 56).
To detect non-metallic radiolucent materials such as plastic and wood ultrasound or computerized axial tomography (CAT scan) is recommended (35, 48, 56, 57, 77). Ultrasound is not routine for detecting foreign bodies even though it is very useful for the study of soft tissue complications such as abscess formation in the liver (35, 36, 48). It is also very useful for those cases in which the physician Bly suspects a foreign object has been ingested, but for which X-rays show no evidence (56). The CAT scan is a sensitive method for diagnosing the presence of foreign bodies such as fish bones (49) and bezoars (57). CAT scans also provide the precise location of the object and its surrounding lesions which it is why it is the most frequently used method for diagnosis of complications associated with ingestion. When there is a possible esophageal perforation, esophagography with water-soluble contrast medium (70) or a CAT scan can locate the perforation or lesion with 78% sensitivity and 96% specificity (61).
Unlike the methods mentioned above, endoscopy can be used for both diagnosis and treatment. This procedure is frequently performed in the general public and sometimes finds foreign bodies incidentally, as in the cases we discussed. Endoscopy is the preferred method for handling foreign body ingestion in the GI and respiratory tracts. In the general western population, endoscopies are requested for removal of swallowed objects in 10% to 20% of all cases (3, 16). However, in Asia, endoscopy procedures have increased to include 90% of all cases of foreign body ingestion. There are three main reasons (1):
1. There are more cases of foreign body ingestion, mostly fish bones which need to be removed to avoid further damage.
2. Endoscopies are less expensive in Asia.
3. American studies are based in a series of cases that are not really sufficient for Asian standards.
Endoscopic treatment avoids surgery, is cost effective, and decreases morbidity (1, 5, 9-11, 50, 61). Its disadvantage is that it depends on an expert to perform and interpret the procedure. When performed properly, endoscopy allows location of the foreign body and visual observation of factors predisposing to lesions and of lacerations of the mucosa caused by the foreign body or by the method used to extract it. It is best to perform the endoscopy at an early stage before the object moves to another area, before the mucosa heals, and before the object causes perforation or further complications.
When a patient presents secondary complications to asymptomatic foreign body ingestion, it is harder to give a medical diagnosis because diagnosis possibilities vary a lot due to the changes in the medical picture and the lack of evidence of ingestion. This makes diagnosis of foreign body ingestion one of the last options to be considered. Considerations must be taken depending on the patients age, symptom progression, duration of medical pictures and patients medical history (3, 5, 45, 67). Under these conditions, clinical suspicion is one of the most reliable tools to diagnose (3), just as observing the patients development and making diagnostic images to rule out any other entities. When these procedures are not enough, surgery procedures will determine diagnosis and treatment. In more extreme and rare cases where the patient has died without any explainable reason, autopsy has been the determining factor to diagnose foreign object ingestion (19, 20, 66).
TREATMENT
Since in most cases physical examination does not show any evidence of anomaly, the first thing to do in managing foreign body ingestion is to write a rigorous clinical history which emphasizes the patients recollection of events (6, 56). Treatment of foreign body ingestion depends on the material, shape, size and location of the object swallowed as well as upon the progression of the object through the GI tract, medical manifestations and complications associated with it. The doctor must determine if the patient requires any immediate medical or surgical intervention (3).
When a patient sees the doctor due to foreign body ingestion, but does not show any clear symptoms, management depends on the characteristics of the ingested object. If the object is radiopaque and the doctor considers that it is possible that it will be spontaneously eliminated without causing any further complications (most frequent situation), then the object needs to be constantly monitored through serial X-rays (3, 5, 10, 25, 36, 44). Most objects can pass through the GI tract in 4 to 6 days, but some may stay for as long as 4 weeks (3, 5, 44, 50). In cases where the object is radiolucent, treatment should be on an outpatient basis, with close evaluation for symptoms. The patient should be kept well informed about symptoms such as intense thoracic or abdominal pain, dysphagia, hematemesis, melena, fever or general discomfort that may need immediate attention. Depending on diagnosis procedures such as GI endoscopy, thorax or abdominal X-rays, ultrasonography, and CAT scans may be needed. If the foreign body is radiopaque and has been monitored radiographically for 72 hours without being found, a determination must be made as to whether there has been penetration into the mucosa or if the object has become embedded somewhere else (5, 25, 36, 45, 67).
For patients who develop additional symptoms resulting from foreign body ingestion, endoscopy or surgery is required. Endoscopy may be used for whether the object ingested is radiolucent or radiopaque (6, 8, 9, 45, 51, 56, 61, 67). Specialized international literature suggests that due to safety issues it is sometimes s better to leave the embedded object where it is instead of removing it (50). In other cases, the object must be removed immediately to avoid complications (Table 4). Batteries need to be removed as soon as possible because of the high risk of necrosis due to liquefaction of tissue (52, 53). Sharp, pointy objects increase the chance of perforated bowels (24, 47), as do swallowed dental prostheses that are being observed. Immediate endoscopic extraction is the best choice in these cases (54). Ingestion of more than one magnet may cause tissue compression and necrosis (24). Those patients who have tried to transport latex bags filled with cocaine or heroin within their bodies should be urged to undergo surgery and must be subjected to endoscopy which could have fatal consequences if any of the bags are torn (22, 45).
Table 4. Indications for foreign body extraction from GI tract.
Although it is a safe procedure, endoscopy can produce complications including perforations, tissue lacerations, and formation of abscess and mediastinitis (10, 61) which inevitably lead to surgical intervention. Both rigid and flexible endoscopes are safe with a mortality rate of 0.08% (45, 78). Despite this endoscopy with flexible endoscopes is preferred because they are easier to handle and allow better exploration of organs like the stomach and the duodenum (3, 8, 11, 45, 61).
There are many tools that can be attached to the endoscope to extract foreign bodies. They include rat-tooth forceps (1, 24, 37), alligator clips, forceps (23, 37, 45), polypectomy forceps and snares (23, 45), Dormia baskets (5, 62) with foreign body protecting caps (1, 55) and endoclips used for damaged tissue hemostasis (16). The instrument is chosen according to the characteristics of the object being extracted (5). Biopsy forceps, rat-tooth forceps and alligator clips have been used to deal with foreign objects located anywhere in the upper GI tract with a success rate of 95.8%. However, S. Zhang and his team recommend using a Dormia basket when a foreign object is located in the esophagus because evidence has shown it to be 10% more successful (5). Even though the use of laryngoscope with Magill forceps has been suggested for the pediatric patient with a foreign body in the proximal esophagus (67), some authors suggest that the initial procedure should be endoscopy (4).
A Dormia basket is used for pieces of food which can be extracted in blocks or in fragments, especially when they are located in the stomach or duodenum (1, 5). Coins or other blunt objects benefit from handling with rat-tooth forceps and Dormia basket (1, 5). Pointy objects are best handled with forceps or polypectomy snares with latex protective caps to avoid injuring the tissue during the extraction procedure (3, 75). A double channel endoscope is used to extract complex and ultra long objects such as dental prostheses and toothpicks (1).
Endoscopy rarely fails (Table 5), but when it does the object is usually a dental prostheses located in the esophagus, deeply nestled magnets or fish bones, or failure occurs in patients with morbid medical conditions (1, 5).
Table 5. Cases in which initial endoscopies failed.
Surgery is the best therapeutic procedure when the object cannot be extracted through endoscopy (5,6,48,54), when there are multiple foreign bodies (54), when there is any complication (perforation, abscess, etc.) (28, 29, 42), or if encapsulated narcotic substances are involved (22, 45). Cervicotomy, thoracotomy and laparotomy are the options when there is a visceral rupture, infection or hemodynamic compromise (11, 13, 23, 63, 70). In recent years, laparoscopy has emerged as an accurate procedure for visual evaluation of the intra-abdominal cavity (24, 33, 36, 71). It is faster and less invasive than laparotomy (54). Combining laparoscopy and endoscopy is a new method for avoiding open surgery which can be done when endoscopy is not satisfactory or too dangerous. This combinations advantages over laparotomy lie in the fact that it is less painful when the patient is recovering from surgery, it requires less analgesia and it allows a quicker recovery in general reducing hospitalization and recovery times. In terms of technique, handling the case combining laparoscopy and endoscopy facilitates location and extraction of the object and allows verification of the integrity of the suture after finishing the procedure (54). When there is perforation, the appropriate procedure is to suspend oral ingestion, and administer parenteral liquids with anaerobic and Gram positive antibiotics. Treatment should be conservative. Enteral feeding should be included, but only when continuity has been restored without any evidence of pleural contamination (hydrothorax or pneumothorax), patient has no symptoms or only minor symptoms such as incomplete perforations or intramural hematoma (70). Linear esophageal perforations that are promptly detected and show no evidence of systematic compromise can be treated with hemoclips. Plastic prostheses can also be used when there is a tear that compromises less than 50% of the circumference (16, 79).
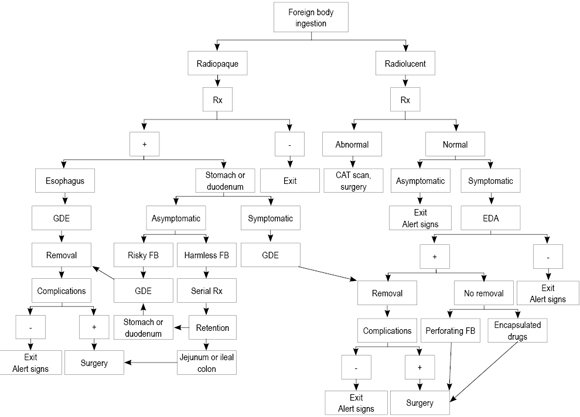
Since there are a number of diagnostic and therapeutic approaches which depend on each teams experience, each group must propose its own algorithm to facilitate their medical practice (11, 25, 44, 51, 68, 78). In the algorithm of Figure 4, we present a proposal based on the present evidence on how to handle foreign body ingestion in adults.
Figure 4. Flow chart of appropriate procedures for foreign bodies in the GI tract.
CONCLUSIONS
1. Foreign body ingestion is a frequent reason for emergency medical examinations especially in the pediatric population.
2. Most patients who see the doctor due to foreign body are asymptomatic. Initially the physician must observe and be alert to any alarming signs.
3. Only 1% of the patients that see the doctor because of foreign body ingestion or related complications require surgery.
4. Occasionally, foreign bodies are incidentally detected while undergoing a medical procedure. They may be associated with critical consequences which are hazardous to the patients life.
5. A flow chart is proposed for successful handling of foreign body ingestion.
REFERENCES
1. Li Z, Sun Z, Zou D, Xu G, Wu R, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc 2006; 64(7): 485-492.
2. Ashraf O. Foreign body in the esophagus: a review. Sao Paulo Med J 2006; 124(6): 346-349.
3. Eisen GM, Baron TH, Dominitz JA et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002; 55(7): 802-806.
4. Gonzáles M, Gómez M, Otero W. Cuerpos extraños en esófago. Rev Col Gastroenterol 2006; 21(3): 150-161.
5. Zhang S, Cui Y, Gong X, Gu F, Chen M. Endoscopic management of de foreign bodies in the upper gastrointestinal tract un south China: a retrospective study of 561 cases. Dig Dis Sci 2009; 55(5): 1305-1312.
6. Yalcin S, Karnak I, Ciftci A, Senocak M, Tanyel F. Foreign body ingestion in children: an analysis of pediatric surgical practice. Pediatr Surg Int 2007; 23: 755-761.
7. Herrera P, Fernández J, Arroyo B, Sánchez F, De Saa M, García R. Cuerpos extraños esofágicos. Medicina General 2002; 47: 660-663.
8. Supaporn O, Thawatchai A, Asada M, Jatuporn S, Mongkol L. Endoscopic Management of Foreign Body in the Upper Gastrointestinal Tract: A Tertiary Care Center Experience. J Med Assoc Thai 2009; 92(1): 17-21.
9. Wong K, Fang C, Tam P. Selective upper endoscopy for foreign body ingestion in children: an evaluation of management protocol after 282 cases. J Ped Surg 2006; 41: 2016-2018.
10. Katsinelos P, Kountouras J, Paroutoglou G, Zavos C, Mimidis K, Chatzimavroudis G. Body Ingestion and Food Bolus Impaction in the Upper Gastrointestinal Tract: A Retrospective Analysis of 139 Cases. J Clin Gastroenterol 2006; 40: 784-789.
11. Gmeiner D, von Rahden B, Meco C, Hutter J, Oberascher G, Stein H. Flexible versus rigid endoscopy for treatment of foreign body impaction in the esophagus. Surg Endosc 2007; 21: 2026-2029.
12. Lana R, Mendoza J, Lérida A. Accidental ingestion of unusual metallic foreign body. Rev Esp Enferm Dig 2004; 96(12): 874-875.
13. Akhtar S, McElvanna N, Gardiner K, Irwin S. Bowel perforation caused by swallowed chicken bones A case series. Ulster Med J 2007; 76(1): 37-38.
14. Barone J, Sohn N, Nealon T. Perforations and Foreign Bodies of the Rectum: Report of 28 Cases. Ann Surg 1976; 184(5): 1976.
15. Ramos R, Duarte P, Vicente C, Casteleiro C. Upper gastrointestinal bleeding triggered by foreign body ingestion. Rev Esp Enferm Dig 2008; 100(4): 238-239.
16. Kim J, Kim H, Cho Y et al. Extraction and clipping repair of a chicken bone penetrating the gastric wall. World J Gastroenterol 2008; 14(12): 1955-1957.
17. Perkins M, Lovell J, Gruenewald S. Life-threatening pica: Liver abscess from perforating foreign body. Australas Radiol 1999; 43: 349-352.
18. Lanitis S, Filippakis G, Christophides T, Papaconstandinou T, Karaliotas C. Case Report: combined Laparoscopic and Endoscopic Approach for the Management of Two Ingested Sewing Needles: One Migrated into the Liver and One Stuck in the Duodenum. J Laparoendosc Adv Surg Tech A 2007; 17(3): 311-314.
19. Chiu H, Chen C, Mol L. Toothpick Perforation of the Duodenum: A Case Report. J Intern Med Taiwan 2004; 15: 219-222.
20. Schwartz J,Graham D. Toothpick Perforation of the Intestines. Ann Surg 1977; 85(1): 64-66.
21. Bisharat M, ODonnell M, Gibson N, et al. Foreign Body Ingestion in Prisoners The Belfast Experience. Ulster Med J 2008; 77(2): 110-114.
22. Sánchez G, Osorio E, Barrera A, Cardona C. Cuerpos extraños en tracto gastrointestinal asociados a trastorno mental. Reporte de caso. Rev Col Gastroenterol 2009; 24(1): 79-85.
23. Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009; 69(3): 426-433.
24. Dominguez S, Wildhaber B, Spadola L, Mehrak A, Chardot C. Laparoscopic extraction of an intrahepatic foreign body after transduodenal migration in a child. J Ped Surg 2009; 44: E17-E20.
25. Gilger M, Jain A, McOmber M. Foreign bodies of the Esophagus and gastrointestinal tract in children. Disponible en: http://www.uptodate.com/contents/foreign-bodies-of-the-esophagus-and-gastrointestinal-tract-in-children
26. Echandia C. Aspiración de cuerpo extraño. Colombia Med 1995; 26: 21-26.
27. Hsu S, Chan D, Liu Y. Small-Bowel Perforation Caused by Fish Bone. World J Gastroenterol 2005; 11(12): 1884-1885.
28. Goh B, Chow P, Quah H et al. Perforation of the Gastrointestinal Tract Secondary to Ingestion of Foreign Bodies. World J Surg 2006; 30: 372-377.
29. Rodríguez J, Cañete N, Artigau E, Gironés J, Planellas P, Codina C. Small bowel perforation by an unusual foreign body. Rev Esp Enferm Dig 2009; 101(9): 639-641.
30. Piñero A, Fernandez J, Carrasco M, Riquelme J, Parrilla P. Intestinal Perforation by Foreign Bodies. Eur J Surg 2000; 166: 307-309.
31. Honaas T, Shaffer E. Endoscopic removal of a foreign body perforating the duodenum. CMAJ 1997; 116(22): 164-69.
22. Wiest J, Follette D, Traverso W. Toothpick Perforation of the Duodenum. West J Med 1980; 132: 157-159.
33. Golffier C, Holguin F, Kobayashi A. Duodenal perforation because of swallowed ballpoint pen and its laparoscopic management: report of a case. J Ped Surg 2009; 44: 634-636.
34. Losanoff J, Kjossev K. Foreign body impaction in the duodenum. J Gastroenterol 1999; 34: 294-295.
35. Kadowaki Y, Tamura R, Okamoto T, Mori T, Mori T. Ruptured Hepatic Abscess Caused by Fish Bone Penetration of the Duodenal Wall: Report of a Case. Surg Today 2007; 37: 1018-1021.
36. Bulakçı M, Agayev A, Yanar F, Sharifov R, Taviloğlu K, Uçar A. Final destination of an ingested needle: the liver. Diagn Interv Radiol 2009; 17(1): 64-66.
37. Jin H,Yeol J,Chul H et al. An Impacted Clamshell in the Duodenum Mistaken for a Gall Stone. Korean J Intern Med 2007; 22: 292-295.
39. Clarencon F, Scatton O, Bruguiere E et al. Recurrent Liver Abscess Secondary to Ingested Fish Bone Migration:Report of a Case. Surg Today 2008; 38: 572-575.
40. Son Y, Woo Y, You S et al. Toothpick impaction with sigmoid colon pseudodiverticulum formation successfully treated with colonoscopy. World J Gastroenterol 2008; 14(6): 948-950.
41. Haidary A, Leider JS, Silbergleit R. Unsuspected Swallowing of a Partial Denture. Am J Neuroradiol 2007; 28: 1734-1735.
42. Cross KM, Holland A. Gravel Gut Small Bowel Perforation Due to a Blunt Ingested Foreign Body. Pediatr Emerg Care 2007; 23(2): 106-108.
43. Chad G, Wyrzykowski AD, Sullivan P, Feliciano D. Intussuscepted intestine through a rectal foreign body. Can J Surg 2009; 52: E191-192.
44. Uyemura M. Foreign Body Ingestion in Children. Am Fam Physician 2005; 72(2): 287-291.
45. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 1995; 41(1): 39-51.
46. Hidalgo A, Garcés R, Hwang H, Córdoba J, Argonz J. Experiencia en resolución de cuerpos extraños en el aparato digestivo alto. Acta Gastro 2006; 36(2): S42.
47. Lacroix S, Ferland A, Gilbert P, Lemieux M, Bilodeau L, Poirier P. Cardiac hazard associated with eating habits. A case of infected intrapericardial foreign body due to an ingested toothpick. Can J Cardiol 2009; 25(7): E263-264.
48. Chintamani, Singhal V, Lubhana P, Durkhere R, Bhandari S. Liver abscess secondary to a broken needle migration- A case report. BMC Surg 2003; 3: 8.
49. Goh B, Yong W, Yeo A. Pancreatic and Hepatic Abscess Secondary to Fish Bone Perforation of the Duodenum. Dig Dis Sci 2005; 50(6): 1103-1106.
50. Lin C, Chen A, Tsai J, Wei S, Hsueh K, Lin W. Endoscopic removal of foreign bodies in children. Kaohsiung J Med Sci 2007; 23: 447-452.
51. Ospina J, Posada ME. Cuerpos extraños en tracto gastrointestinal en niños. Rev Col Gastroenterol 2008; 23(3): 233-238.
52. Bakes K. Alarming Rise in Major Complications from Button Battery Ingestions. Disponible en: http://www. emergency-medicine.jwatch.org/cgi/content/full/2010/625/1
53. Sinclair K, Hill I. Button Battery Ingestion. Disponible en: http:// www.uptodate.com/contents/button-battery-ingestion
54. Olson J, Weinstock L, Brunt L. Combined endoscopic and laparoscopic approach to remove a sharp gastric foreign body. Gastrointest Endosc 2000; 51(4): 500-502.
55. Enjoji A, Nagata Y, Furuichi A, Kawakami S, Saiwai H, Furui J. Successful removal from the duodenum of swallowed sewing needles using devised endoscopic forceps. Endoscopy 2004; 36(2): 193.
56. Tokar B, Cevik AA, Ilhan H. Ingested gastrointestinal foreign bodies: predisposing factors for complications in children having surgical or endoscopic removal. Pediatr Surg Int 2007; 23(2): 135-139.
57. Ripollés T, García-Aguayo J, Martínez MJ, Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. Am J Roentgenol 2001; 177: 65-69.
58. Chao HH, Chao TC. Perforation of the duodenum by an ingested toothbrush. World J Gastroenterol 2008; 14(27): 4410-4412.
59. Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg 1996; 20(8): 1001-1005 (Abstract).
60. Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009; 69(3): 426-433.
61. Luk WH, Fan WC, Chan RY, Chan SW, Tse KH, Chan JC. Foreign body ingestion: comparison of diagnostic accuracy of computed tomography versus endoscopy. J Laryngol Otol 2009; 123(5): 535-540.
62. Ko H. Review of food bolus management. Can J Gastroenterol 2008; 22(10): 805-808.
63. Steele S, Goldgerg J. Rectal Foreign Bodies. http://www.uptodate.com/contents/rectal-foreign-bodies.
64. Türkyilmaz A, Aydin Y, Yilmaz O, Aslan S, Eroğlu A, Karaoğlanoğlu N. Esophageal foreign bodies: analysis of 188 cases. Ulus Travma Acil Cerrahi Derg 2009; 15(3): 222-227.
65. Gilchrist BF, Valerie EP, Nguyen M, Coren C, Klotz D, Ramenofsky ML. Pearls and perils in the management of prolonged, peculiar, penetrating esophageal foreign bodies in children. J Pediatr Surg 1997; 32(10): 1429-1431.
66. Song Y, Liu Q, Shen H, Jia X, Zhang H, Qiao L. Diagnosis and management of primary aortoenteric fistulas - experience learned from eighteen patients. Surgery 2008; 143(1): 43-50.
67. Athanassiadi K, Gerazounis M, Metaxas E, Kalantzi N. Management of esophageal foreign bodies: a retrospective review of 400 cases. Eur J Cardiothorac Surg 2002; 21(4): 653-656.
68. Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg 1999; 34(10): 1472-1476.
69. Lafuente NI, Argibay JC, Castro A. Absceso retrofaríngeo tras ingesta de cuerpo extraño. Medifam 2002; 12(5): 344-347.
70. Amir AI, van Dullemen H, Plukker JT. Selective approach in the treatment of esophageal perforations. Scand J Gastroenterol 2004; 39(5): 418-422.
71. Dominguez S, Wildhaber BE, Spadola L, Mehrak AD, Chardot C. Laparoscopic extraction of an intrahepatic foreign body after transduodenal migration in a child. J Ped Surg 2009; 44(11): E17-20.
72. Akçam M, Koçkar C, Tola HT, Duman L, Gündüz M. Endoscopic removal of an ingested pin migrated into the liver and affixed by its head to the duodenum. Gastrointest Endosc 2009; 69(2): 382-384.
73. Nigri GR, di Giulio E, di Nardo R et al. Duodenal perforation and right hydronephrosis due to toothpick ingestion. J Emerg Med 2008; 34(1): 55-57.
74. Newman B. Duodenorenal fistula. Pediatr Radiol 2004; 34(4): 343-347.
75. Kalayci A, Tander B, Kocak S, Rizalar R, Bernay F. Removal of open safety pins in infants by flexible endoscopy is effective and safe. J Laparoendosc Adv Surg Tech A 2007; 17(2): 242-245.
76. Thompson MH. Endoscopic removal of a duodenal foreign body. Br Med J 1975; 4: 502-503.
77. Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol 2009; 39(3): 299-301.
78. Balasubramaniam SK, Bray D, Black MI, Salama NY, Mitchell DB. A review of the current management of impacted foreign bodies in the oesophagus in adults. Eur Arch Otorhinolaryngol 2008; 265(8): 951-956.
79. Siersema PD. Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena. Gastrointest Endosc 2005; 61(7): 897-900.
1. Li Z, Sun Z, Zou D, Xu G, Wu R, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc 2006; 64(7): 485-492. [ Links ]
2. Ashraf O. Foreign body in the esophagus: a review. Sao Paulo Med J 2006; 124(6): 346-349. [ Links ]
3. Eisen GM, Baron TH, Dominitz JA et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002; 55(7): 802-806. [ Links ]
4. Gonzáles M, Gómez M, Otero W. Cuerpos extraños en esófago. Rev Col Gastroenterol 2006; 21(3): 150-161. [ Links ]
5. Zhang S, Cui Y, Gong X, Gu F, Chen M. Endoscopic management of de foreign bodies in the upper gastrointestinal tract un south China: a retrospective study of 561 cases. Dig Dis Sci 2009; 55(5): 1305-1312. [ Links ]
6. Yalcin S, Karnak I, Ciftci A, Senocak M, Tanyel F. Foreign body ingestion in children: an analysis of pediatric surgical practice. Pediatr Surg Int 2007; 23: 755-761. [ Links ]
7. Herrera P, Fernández J, Arroyo B, Sánchez F, De Saa M, García R. Cuerpos extraños esofágicos. Medicina General 2002; 47: 660-663. [ Links ]
8. Supaporn O, Thawatchai A, Asada M, Jatuporn S, Mongkol L. Endoscopic Management of Foreign Body in the Upper Gastrointestinal Tract: A Tertiary Care Center Experience. J Med Assoc Thai 2009; 92(1): 17-21. [ Links ]
9. Wong K, Fang C, Tam P. Selective upper endoscopy for foreign body ingestion in children: an evaluation of management protocol after 282 cases. J Ped Surg 2006; 41: 2016-2018. [ Links ]
10. Katsinelos P, Kountouras J, Paroutoglou G, Zavos C, Mimidis K, Chatzimavroudis G. Body Ingestion and Food Bolus Impaction in the Upper Gastrointestinal Tract: A Retrospective Analysis of 139 Cases. J Clin Gastroenterol 2006; 40: 784-789. [ Links ]
11. Gmeiner D, von Rahden B, Meco C, Hutter J, Oberascher G, Stein H. Flexible versus rigid endoscopy for treatment of foreign body impaction in the esophagus. Surg Endosc 2007; 21: 2026-2029. [ Links ]
12. Lana R, Mendoza J, Lérida A. Accidental ingestion of unusual metallic foreign body. Rev Esp Enferm Dig 2004; 96(12): 874-875. [ Links ]
13. Akhtar S, McElvanna N, Gardiner K, Irwin S. Bowel perforation caused by swallowed chicken bones – A case series. Ulster Med J 2007; 76(1): 37-38. [ Links ]
14. Barone J, Sohn N, Nealon T. Perforations and Foreign Bodies of the Rectum: Report of 28 Cases. Ann Surg 1976; 184(5): 1976. [ Links ]
15. Ramos R, Duarte P, Vicente C, Casteleiro C. Upper gastrointestinal bleeding triggered by foreign body ingestion. Rev Esp Enferm Dig 2008; 100(4): 238-239. [ Links ]
16. Kim J, Kim H, Cho Y et al. Extraction and clipping repair of a chicken bone penetrating the gastric wall. World J Gastroenterol 2008; 14(12): 1955-1957. [ Links ]
17. Perkins M, Lovell J, Gruenewald S. Life-threatening pica: Liver abscess from perforating foreign body. Australas Radiol 1999; 43: 349-352. [ Links ]
18. Lanitis S, Filippakis G, Christophides T, Papaconstandinou T, Karaliotas C. Case Report: combined Laparoscopic and Endoscopic Approach for the Management of Two Ingested Sewing Needles: One Migrated into the Liver and One Stuck in the Duodenum. J Laparoendosc Adv Surg Tech A 2007; 17(3): 311-314. [ Links ]
19. Chiu H, Chen C, Mol L. Toothpick Perforation of the Duodenum: A Case Report. J Intern Med Taiwan 2004; 15: 219-222. [ Links ]
20. Schwartz J,Graham D. Toothpick Perforation of the Intestines. Ann Surg 1977; 85(1): 64-66. [ Links ]
21. Bisharat M, ODonnell M, Gibson N, et al. Foreign Body Ingestion in Prisoners – The Belfast Experience. Ulster Med J 2008; 77(2): 110-114. [ Links ] 22. Sánchez G, Osorio E, Barrera A, Cardona C. Cuerpos extraños en tracto gastrointestinal asociados a trastorno mental. Reporte de caso. Rev Col Gastroenterol 2009; 24(1): 79-85. [ Links ] 23. Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009; 69(3): 426-433. [ Links ] 24. Dominguez S, Wildhaber B, Spadola L, Mehrak A, Chardot C. Laparoscopic extraction of an intrahepatic foreign body after transduodenal migration in a child. J Ped Surg 2009; 44: E17-E20. [ Links ] 25. Gilger M, Jain A, McOmber M. Foreign bodies of the Esophagus and gastrointestinal tract in children. Disponible en: http://www.uptodate.com/contents/foreign-bodies-of-the-esophagus-and-gastrointestinal-tract-in-children [ Links ] 26. Echandia C. Aspiración de cuerpo extraño. Colombia Med 1995; 26: 21-26. [ Links ] 27. Hsu S, Chan D, Liu Y. Small-Bowel Perforation Caused by Fish Bone. World J Gastroenterol 2005; 11(12): 1884-1885. [ Links ] 28. Goh B, Chow P, Quah H et al. Perforation of the Gastrointestinal Tract Secondary to Ingestion of Foreign Bodies. World J Surg 2006; 30: 372-377. [ Links ] 29. Rodríguez J, Cañete N, Artigau E, Gironés J, Planellas P, Codina C. Small bowel perforation by an unusual foreign body. Rev Esp Enferm Dig 2009; 101(9): 639-641. [ Links ] 30. Piñero A, Fernandez J, Carrasco M, Riquelme J, Parrilla P. Intestinal Perforation by Foreign Bodies. Eur J Surg 2000; 166: 307-309. [ Links ] 31. Honaas T, Shaffer E. Endoscopic removal of a foreign body perforating the duodenum. CMAJ 1997; 116(22): 164-69. [ Links ] 32. Wiest J, Follette D, Traverso W. Toothpick Perforation of the Duodenum. West J Med 1980; 132: 157-159. [ Links ] 33. Golffier C, Holguin F, Kobayashi A. Duodenal perforation because of swallowed ballpoint pen and its laparoscopic management: report of a case. J Ped Surg 2009; 44: 634-636. [ Links ] 34. Losanoff J, Kjossev K. Foreign body impaction in the duodenum. J Gastroenterol 1999; 34: 294-295. [ Links ] 35. Kadowaki Y, Tamura R, Okamoto T, Mori T, Mori T. Ruptured Hepatic Abscess Caused by Fish Bone Penetration of the Duodenal Wall: Report of a Case. Surg Today 2007; 37: 1018-1021. [ Links ] 36. Bulakci M, Agayev A, Yanar F, Sharifov R, Taviloglu K, Ucar A. Final destination of an ingested needle: the liver. Diagn Interv Radiol 2009; 17(1): 64-66. [ Links ] 37. Jin H,Yeol J,Chul H et al. An Impacted Clamshell in the Duodenum Mistaken for a Gall Stone. Korean J Intern Med 2007; 22: 292-295. [ Links ] 38. Rathore PK, Raj A, Sayal A, Meher R, Gupta B, Girhotra M. Prolonged foreign body impaction in the oesophagus. Singapore Med J 2009; 50(2): E53-54. [ Links ] 39. Clarencon F, Scatton O, Bruguiere E et al. Recurrent Liver Abscess Secondary to Ingested Fish Bone Migration:Report of a Case. Surg Today 2008; 38: 572-575. [ Links ] 40. Son Y, Woo Y, You S et al. Toothpick impaction with sigmoid colon pseudodiverticulum formation successfully treated with colonoscopy. World J Gastroenterol 2008; 14(6): 948-950. [ Links ] 41. Haidary A, Leider JS, Silbergleit R. Unsuspected Swallowing of a Partial Denture. Am J Neuroradiol 2007; 28: 1734-1735. [ Links ] 42. Cross KM, Holland A. Gravel Gut Small Bowel Perforation Due to a Blunt Ingested Foreign Body. Pediatr Emerg Care 2007; 23(2): 106-108. [ Links ] 43. Chad G, Wyrzykowski AD, Sullivan P, Feliciano D. Intussuscepted intestine through a rectal foreign body. Can J Surg 2009; 52: E191-192. [ Links ] 44. Uyemura M. Foreign Body Ingestion in Children. Am Fam Physician 2005; 72(2): 287-291. [ Links ] 45. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 1995; 41(1): 39-51. [ Links ] 46. Hidalgo A, Garcés R, Hwang H, Córdoba J, Argonz J. Experiencia en resolución de cuerpos extraños en el aparato digestivo alto. Acta Gastro 2006; 36(2): S42. [ Links ] 47. Lacroix S, Ferland A, Gilbert P, Lemieux M, Bilodeau L, Poirier P. Cardiac hazard associated with eating habits. A case of infected intrapericardial foreign body due to an ingested toothpick. Can J Cardiol 2009; 25(7): E263-264. [ Links ] 48. Chintamani, Singhal V, Lubhana P, Durkhere R, Bhandari S. Liver abscess secondary to a broken needle migration- A case report. BMC Surg 2003; 3: 8. [ Links ] 49. Goh B, Yong W, Yeo A. Pancreatic and Hepatic Abscess Secondary to Fish Bone Perforation of the Duodenum. Dig Dis Sci 2005; 50(6): 1103-1106. [ Links ] 50. Lin C, Chen A, Tsai J, Wei S, Hsueh K, Lin W. Endoscopic removal of foreign bodies in children. Kaohsiung J Med Sci 2007; 23: 447-452. [ Links ] 51. Ospina J, Posada ME. Cuerpos extraños en tracto gastrointestinal en niños. Rev Col Gastroenterol 2008; 23(3): 233-238. [ Links ] 52. Bakes K. Alarming Rise in Major Complications from Button Battery Ingestions. Disponible en: http://www. emergency-medicine.jwatch.org/cgi/content/full/2010/625/1. [ Links ] 53. Sinclair K, Hill I. Button Battery Ingestion. Disponible en: http:// www.uptodate.com/contents/button-battery-ingestion [ Links ] 54. Olson J, Weinstock L, Brunt L. Combined endoscopic and laparoscopic approach to remove a sharp gastric foreign body. Gastrointest Endosc 2000; 51(4): 500-502. [ Links ] 55. Enjoji A, Nagata Y, Furuichi A, Kawakami S, Saiwai H, Furui J. Successful removal from the duodenum of swallowed sewing needles using devised endoscopic forceps. Endoscopy2004; 36(2): 193. [ Links ] 56. Tokar B, Cevik AA, Ilhan H. Ingested gastrointestinal foreign bodies: predisposing factors for complications in children having surgical or endoscopic removal. Pediatr Surg Int2007; 23(2): 135-139. [ Links ] 57. Ripollés T, García-Aguayo J, Martínez MJ,Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. Am J Roentgenol2001; 177: 65-69. [ Links ] 58. Chao HH, Chao TC. Perforation of the duodenum by an ingested toothbrush. World J Gastroenterol 2008; 14(27): 4410-4412. [ Links ] 59. Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg 1996; 20(8): 1001-1005 (Abstract). [ Links ] 60. Palta R, Sahota A, Bemarki A, Salama P, Simpson N,Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc2009; 69(3): 426-433. [ Links ] 61. Luk WH, Fan WC, Chan RY, Chan SW, Tse KH, Chan JC. Foreign body ingestion: comparison of diagnostic accuracy of computed tomography versus endoscopy. J Laryngol Otol2009; 123(5): 535-540. [ Links ] 62. Ko H. Review of food bolus management. Can J Gastroenterol 2008; 22(10): 805-808. [ Links ] 63. Steele S, Goldgerg J. Rectal Foreign Bodies. http://www.uptodate.com/contents/rectal-foreign-bodies. [ Links ] 64. Türkyilmaz A, Aydin Y, Yilmaz O, Aslan S, Eroglu A, Karaoglanoglu N. Esophageal foreign bodies: analysis of 188 cases. Ulus Travma Acil Cerrahi Derg2009; 15(3): 222-227. [ Links ] 65. Gilchrist BF, Valerie EP, Nguyen M, Coren C, Klotz D, Ramenofsky ML. Pearls and perils in the management of prolonged, peculiar, penetrating esophageal foreign bodies in children. J Pediatr Surg1997; 32(10): 1429-1431. [ Links ] 66. Song Y, Liu Q, Shen H, Jia X, Zhang H,Qiao L. Diagnosis and management of primary aortoenteric fistulas - experience learned from eighteen patients. Surgery2008; 143(1): 43-50. [ Links ] 67. Athanassiadi K, Gerazounis M, Metaxas E, Kalantzi N. Management of esophageal foreign bodies: a retrospective review of 400 cases. Eur J Cardiothorac Surg2002; 21(4): 653-656. [ Links ] 68. Cheng W,Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg1999; 34(10): 1472-1476. [ Links ] 69. Lafuente NI, Argibay JC, Castro A. Absceso retrofaríngeo tras ingesta de cuerpo extraño. Medifam 2002; 12(5): 344-347. [ Links ] 70. Amir AI, van Dullemen H, Plukker JT. Selective approach in the treatment of esophageal perforations. Scand J Gastroenterol2004; 39(5): 418-422. [ Links ] 71. Dominguez S, Wildhaber BE, Spadola L, Mehrak AD, Chardot C. Laparoscopic extraction of an intrahepatic foreign body after transduodenal migration in a child. J Ped Surg2009; 44(11): E17-20. [ Links ] 72. Akçam M, Koçkar C, Tola HT, Duman L, Gündüz M. Endoscopic removal of an ingested pin migrated into the liver and affixed by its head to the duodenum. Gastrointest Endosc2009; 69(2): 382-384. [ Links ] 73. Nigri GR,di Giulio E,di Nardo R et al. Duodenal perforation and right hydronephrosis due to toothpick ingestion. J Emerg Med 2008;34(1):55-57. [ Links ] 74. Newman B. Duodenorenal fistula. Pediatr Radiol2004; 34(4): 343-347. [ Links ] 75. Kalayci A, Tander B, Kocak S, Rizalar R, Bernay F. Removal of open safety pins in infants by flexible endoscopy is effective and safe. J Laparoendosc Adv Surg Tech A2007; 17(2): 242-245. [ Links ] 76. Thompson MH. Endoscopic removal of a duodenal foreign body. Br Med J1975; 4: 502-503. [ Links ] 77. Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol2009; 39(3): 299-301 [ Links ] 78. Balasubramaniam SK, Bray D, Black MI, Salama NY, Mitchell DB. A review of the current management of impacted foreign bodies in the oesophagus in adults. Eur Arch Otorhinolaryngol2008; 265(8): 951-956. [ Links ] 79. Siersema PD. Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena. Gastrointest Endosc 2005; 61(7): 897-900. [ Links ]











 texto en
texto en