Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev Col Gastroenterol v.27 n.2 Bogotá abr./jun. 2012
A ruptured spleen following colonoscopy is a rare, but potentially lethal complication
Jorge E Rodríguez Fajardo, MD. (1), Javier Carrera S., MD. (2), Heinz Ibáñez, MD. (2), Carlos Martínez, MD. (2), Lina Mateus, MD. (2)
(1) Coloproctology Fellow at the Universidad Militar Nueva Granada, Bogotá, Colombia.
(2) Coloproctologist at the Hospital Militar. Bogotá, Colombia.
Received: 30-08-11 Accepted: 15-05-12
Abstract
Colonoscopy is the paramount diagnostic tool for polyps and lesions in the colon and rectum. Although, the most common cause of complications are bleeding and perforations, diagnostic colonoscopy generally has a low incidence of complications. Less common complications include pneumomediastinum, pneumoperitoneum and splenic injuries. We describe a clinical case of a spleen injury following colonoscopy in the colorectal surgery section of the Army Hospital and Nueva Granada University in Bogotá, Colombia. This splenic injury was discovered 48 hours after surgery. Splenic injury could be considered a very unusual cause of abdominal pain following colonoscopy but it could potentially be dangerous. A CT scan is a remarkable diagnostic tool but it is not considered to be useful for deciding on surgical treatment. Clinical observation with follow up, IV fluids, transfusions and antibiotics is one treatment option. Splenectomy is the most common option found in our review. Clinical suspicion and early diagnosis are the cornerstones for avoiding morbidity and mortality in this rare endoscopic complication.
Key words
Spleen, colonoscopy, splenectomy, splenic injury.
Although colonoscopy is considered to be the most important tool used for detection of malignant or benign lesions, it is not exempt from complications even though most of these procedures are diagnostic. In the last 5 years the 145,000 new cases of colorectal cancer recorded in the United States produced more than 56,000 deaths per year. In the last 5 years early detection has been associated with up to 90% decreases in mortality rates as curative treatment in the early stages of localized disease has led to improved survival. Although colonoscopy provides an excellent image of the colon, it also allows us to treat the majority of polyps and to take biopsies of any masses found. Nevertheless, performance of this procedure is not exempt from complications. The probability of complications such as perforation and severe bleeding is about 6.4 per 100,000 colonoscopies. Also, the probability of perforations during therapeutic colonoscopies is 0.4% while the probability of bleeding is 1.2%, which are both less than the probabilities with diagnostic procedures (2). Nevertheless colonoscopy is a safe procedure: intraluminal bleeding occurs in only 0.3% to 2.1% of cases while perforations occur in between the 0.1% to 2.5% of cases. Other less frequent complications include mesentery disruptions, pneumomediastinum, pneumothorax, pneumoscrotum, retroperitoneal emphysema, sepsis, diverticulitis, appendicitis, volvulus and methane gas explosions.
CLINICAL CASE
A 61 year old woman came to the Hospital Militar Central coloproctology out patient service for a diagnostic colonoscopy for lower gastrointestinal tract bleeding (rectal bleeding) associated with abdominal distension and gastrointestinal postprandial symptoms. She mentioned no family history of colorectal cancer.
A diagnostic colonoscopy found only diverticular disease without complications in the descending and sigmoid colon. The performance of the exam was described as difficult due to problems during intubation.
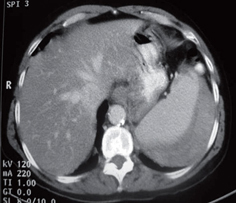
Five days later the patient came to the emergency department with severe left side and upper left quadrant abdominal pain which did not improve with the use of analgesics. The only relevant background was that she is a regular smoker (one pack of cigarettes per day). Her hemoglobin levels were within normal limits, and she did not have leukocytosis. It was decided to hospitalize the patient and to perform an abdominal CT scan to rule out perforation. The CT scan revealed a hematoma covering 20% of the spleen (Figure 1).
Figure 1. Initial CT scan.
Patient was hospitalized for observation and management. During hospitalization, detection of an 8.0 g/dl decrease of hemoglobin levels was treated with transfusion of red blood cell packs. Administration of pain control and antibiotics continued.
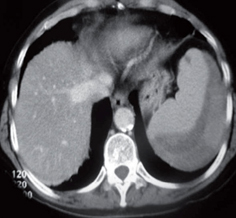
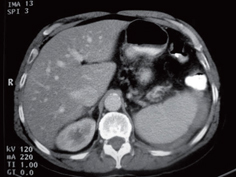
The patient improved but a follow-up abdominal CT scan showed a 40% increase in the size of the hematoma (Figure 2) without further progression. Patient continued under observation without any need for additional new transfusions. Administration of antibiotics continued until she showed clinical improvement and was discharged with ambulatory postoperative controls (Figure 3).
Figure 2. CT scan 48 hours later.
Figure 3. Follow-up CT scan.
DISCUSSION
The first ruptured spleen associated with diagnostic colonoscopy was reported in 1974 by Wherry and Zehner (4-5). The incidence of ruptured spleens associated with diagnostic colonoscopy has been reported at between 0.00005% and 0.017% with a mortality rate of 5%. Despite its dramatic development it is commonly diagnosed late since symptoms such as those in this case can also be attributed to distention due to excessive insufflation, serositis or post-therapeutic polypectomy colonoscopies. There can also be cases of voluntary under registration of morbidity during these procedures. Due to lack of suspicion in these cases, they remain unregistered and are treated symptomatically with antispasmodics (4 -14).
The majority of the patients that present this type of injury arrive at urgency services 24 hours after the procedure suffering from abdominal pain (5). Hypotension, anemia, leukocytosis, abdominal distension, and Kehr's sign (pain in the left upper quadrant region radiating to the ipsilateral shoulder) can occur in more complicated cases. The appearance of Kehr's sign is not related to the need for laparotomy or to the success of conservative management (4). Seventy to eighty such cases have been reported to date, although the number reported has increased since 2006 during which time about 35 cases have been described (5-7). In Fong's review of 66 cases (77.3% female, 21% male, average age 65 years), injuries of the spleen were not related to prior histories of surgery.
Diagnosis of this type of injury with CT scans which are more accurate than other diagnostic methods is now the norm. In Shah's review of 35 cases (5, 6), 50% of the cases reviewed were diagnosed by CT. Only two of the cases were diagnosed with ultrasound while 25% were diagnosed during laparotomy for hemodynamic compromise. Difficulties during colonoscopies were not associated with injuries to the spleen. Only 1% of the cases were reported as "difficult" (4, 17) while only 12% of these cases required additional maneuvers for cecal intubation. In the cases reviewed in the literature, 29% were diagnosed with laparotomy. Most likely these cases occurred before 1991 and had hemodynamically unstable clinical presentations (4-7). 2% were diagnosed at autopsy.
Clinical presentation of symptoms described in 74% of the cases occurred within the first 24 hours following procedures while 81% of patients developed symptoms within 48 hours of procedures. Nevertheless, there are reports of diagnoses as late as 15 days after procedures. (4, 13)
The principal symptoms are abdominal pain. This occurred in the left hypochondrium in almost 36% of cases while generalized abdominal pain was found in 30% of the cases. Hemodynamic instability occurred in 48% of cases. Of the patients sent to surgery more than half had splenic hematomas, lacerations and ruptures.
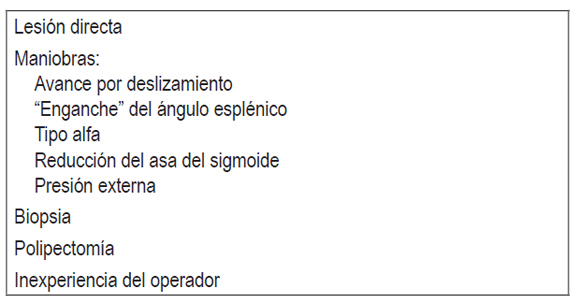
Multiple mechanisms leading to injury during colonoscopy are possible, but have not yet been definitively established. Some factors depend on the endoscopist while others depend on the patient (Tables 1 and 2). However, the most common theory is that these lesions are caused by splenic ligament colic strain resulting from excessive handling associated with poor mobility of the spleen due to adhesions to the colon. Avulsion of the capsule is also possible, and is more common than rupture. Excessive traction on the ligaments from external pressure in the left upper quadrant corrected to maintain the endoscope (sic) (Figure 4). Some classical maneuvers exist to advance on the splenic flexure. They include as sliding forward maneuvers, reducing the sigmoid loop and hooking onto the splenic flexure to correct the sigmoid loop (Figure 4). Other maneuvers unrelated to splenic flexure sometimes involve excessive torque used to enter the terminal ileum. The left lateral decubitus position appears to be a factor which protects the supine position because it allows the spleen and ligaments to fall to the left and decreases the tension on the splenic colic ligament (4-15).
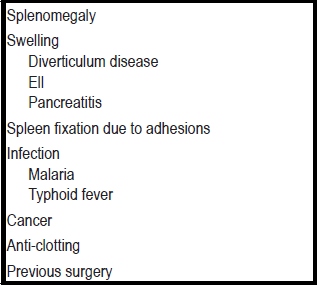
Table 1. Patient-dependent factors.
Table 2. Endoscopist factors.
Figure 4. Intubation Maneuver.
70% of cases of ruptured spleens were invasively managed through splenectomies while conservative management was used in only 29% of the cases. Conservative management included hospitalization with bed rest, intravenous antibiotics, strict monitoring of vital signs, and resuscitation with crystalloids or blood transfusions if the patient required hemoglobin control. The number of units of red blood cells used was higher for patients who had medical management. The decision to management a patient conservatively was always based on CT scan findings, but CT scans cannot consistently predict whether conservative management will be successful. Also, the decision to perform a splenectomy was based principally on patient instability rather than on CT scan findings (7, 16). Embolization was a therapeutic option in only 2% of the cases.
In the Hospital Militar, over 2200 diagnostic and therapeutic colonoscopies are performed annually. Of these, 30% are therapeutic colonoscopies. The rate of perforations is 0.2% while that for bleeding complications is 0.1%. The lesion presented in this article was first ever recorded in our service (0.00045%).
CONCLUSION
Injury to the spleen following a colonoscopy is a rare complication which nevertheless should be considered as a possible cause for abdominal pain after a colonoscopy. The emergence of new cases demonstrates the importance of recording such complications. The majority of these patients consulted doctors during the first 48 hours after the procedure as soon as symptoms began. Diagnoses were done with abdominal CT scans. Treatment decisions and the success of conservative management were not related to CT scan follow-up. Follow-up and clinical suspicion promote early diagnosis and prompt treatment of these injuries reducing the possibility of death.
REFERENCES
1. Nash GM. Advanced colon and rectal cancer. American Society of Colon and Rectal Cancer; 2011. Disponible en: www.fascrs.org.
2. Markowitz AW. Colorectal cancer screening and surveillance. Colorectal cancer. Evidence-based chemotherapy strategies. Leonard Saltz, editor. New Jersey: Human Press; 2007. p. 51-68.
3. O'Brien MJ, Winawer SJ, Zauber AG, Gottlieb LS, Sternberg SS, Diaz B, et al. The National Polyp Study. Patient and polyp characteristics associated with high-grade dysplasia in colorectal adenomas. Gastroenterology 1990; 98(2): 371-9.
4. Fong Ha J, Minchin D. Splenic injury in colonoscopy: a review. Int J Surg 2009; 7(5): 424-7.
5. Shah PR, Raman S, Haray PN. Splenic rupture following colonoscopy: rare in the UK? Surgeon 2005; 3(4): 293-5.
6. Sarhan M, Ramcharan A, Ponnapalli S. Splenic injury after elective colonoscopy. JSLS 2009; 13(4): 616-9.
7. Lalor PF, Mann BD. Splenic rupture after colonoscopy. JSLS 2007; 11(1): 151-6.
8. Harbrecht BG. Is anything new in adult blunt splenic trauma? Am J Surg 2005; 190(2): 273-8.
9. Volchok J, Cohn M. Rare complications following colonoscopy: case reports of splenic rupture and appendicitis. JSLS 2006; 10(1): 114-6.
10. Espinal EA, Hoak T, Porter JA, Slezak FA. Splenic rupture from colonoscopy. A report of two cases and review of the literature. Surg Endosc 1997; 11(1): 71-3.
11. Janes SE, Cowan IA, Dijkstra B. A life threatening complication after colonoscopy. BMJ 2005; 330(7496): 889-90.
12. Olshaker JS, Deckleman C. Delayed presentation of splenic rupture after colonoscopy. J Emerg Med 1997; 17(3): 455-7.
13. de Vries J, Ronnen HR, Oomen AP, Linskens RK. Splenic rupture following colonoscopy, a rare complication. Neth J Med 2009; 67(6): 230-3.
14. Zenooz NA, Win T. Splenic rupture after diagnostic colonoscopy: a case report. Emerg Radiol 2006; 12(6): 272-3.
15. Galperin-Aizenberg M, Blachar A, Gayer G. Iatrogenic injury to the spleen-CT appearance. Semin Ultrasound CT MR 2007; 28(1):52-6.
16. Reissman P, Durst AL. Splenic hematoma. A rare complication of colonoscopy. Surg Endosc 1998;12(2): 154-5.
17. Peterson CR, Adamsen S, Gocht-Jensen P, Arnesen RB, Hart-Hansen O. Splenic injury after colonoscopy. Endoscopy 2008; 40(1): 76-9.
1. Nash GM. Advanced colon and rectal cancer. American Society of Colon and Rectal Cancer; 2011. Disponible en: www.fascrs.org. [ Links ]
2. Markowitz AW. Colorectal cancer screening and surveillance. Colorectal cancer. Evidence-based chemotherapy strategies. Leonard Saltz, editor. New Jersey: Human Press; 2007. p. 51-68. [ Links ]
3. O'Brien MJ, Winawer SJ, Zauber AG, Gottlieb LS, Sternberg SS, Diaz B, et al. The National Polyp Study. Patient and polyp characteristics associated with high-grade dysplasia in colorectal adenomas. Gastroenterology 1990; 98(2): 371-9. [ Links ]
4. Fong Ha J, Minchin D. Splenic injury in colonoscopy: a review. Int J Surg 2009; 7(5): 424-7. [ Links ]
5. Shah PR, Raman S, Haray PN. Splenic rupture following colonoscopy: rare in the UK? Surgeon 2005; 3(4): 293-5. [ Links ]
6. Sarhan M, Ramcharan A, Ponnapalli S. Splenic injury after elective colonoscopy. JSLS 2009; 13(4): 616-9. [ Links ]
7. Lalor PF, Mann BD. Splenic rupture after colonoscopy. JSLS 2007; 11(1): 151-6. [ Links ]
8. Harbrecht BG. Is anything new in adult blunt splenic trauma? Am J Surg 2005; 190(2): 273-8. [ Links ]
9. Volchok J, Cohn M. Rare complications following colonoscopy: case reports of splenic rupture and appendicitis. JSLS 2006; 10(1): 114-6. [ Links ]
10. Espinal EA, Hoak T, Porter JA, Slezak FA. Splenic rupture from colonoscopy. A report of two cases and review of the literature. Surg Endosc 1997; 11(1): 71-3. [ Links ]
11. Janes SE, Cowan IA, Dijkstra B. A life threatening complication after colonoscopy. BMJ 2005; 330(7496): 889-90. [ Links ]
12. Olshaker JS, Deckleman C. Delayed presentation of splenic rupture after colonoscopy. J Emerg Med 1997; 17(3): 455-7. [ Links ]
13. de Vries J, Ronnen HR, Oomen AP, Linskens RK. Splenic rupture following colonoscopy, a rare complication. Neth J Med 2009; 67(6): 230-3. [ Links ]
14. Zenooz NA, Win T. Splenic rupture after diagnostic colonoscopy: a case report. Emerg Radiol 2006; 12(6): 272-3. [ Links ]
15. Galperin-Aizenberg M, Blachar A, Gayer G. Iatrogenic injury to the spleen-CT appearance. Semin Ultrasound CT MR 2007; 28(1):52-6. [ Links ]
16. Reissman P, Durst AL. Splenic hematoma. A rare complication of colonoscopy. Surg Endosc 1998;12(2): 154-5. [ Links ]
17. Peterson CR, Adamsen S, Gocht-Jensen P, Arnesen RB, Hart-Hansen O. Splenic injury after colonoscopy. Endoscopy 2008;40(1): 76-9. [ Links ]











 texto em
texto em